Introduction
Breast cancer is the most common type of diagnosed cancer in women worldwide, and it is estimated that 226,870 new cases will be diagnosed in the United States in 2012 (American Cancer Society, 2012). Cancer patients experience distress during the course of their disease that likely will be exacerbated at some point by pain. Indeed, a diagnosis of cancer likely elicits greater distress than any other diagnosis, regardless of the prognosis (National Cancer Institute, 1997), with a cascade of co-morbid distressing symptoms (Cimprich,1999; McCorkle and Quint-Benoliel, 1983). For example, symptoms such as pain and fatigue may continue well after treatment ends (Dodd et al., 2001; Esper and Heidrich, 2005).While there have been tremendous advances in the treatment of cancer over the past several decades, cancer-related pain is under-treated, and opioids remain the medical standard for treatment (Blasco, Berzosa, Iranzo, and Camps, 2009; Portenoy, 2005).The purpose here was to investigate the efficacy of an eight-week mindfulness-based stress reduction program (MBSR) on pain and distress factors in women diagnosed with breast cancer. A review of pain anxiety, pain catastro-phizing, symptoms of distress, and fatigue in women diagnosed with breast cancer now will be presented.
Literature Review
Pain is the most persistent and incapacitating symptom as well as the most distressing symptom experienced by cancer patients (Wells, Murphy, Wujcik, and Johnson, 2003). The prevalence of chronic pain post-surgery for breast cancer frequently is attributed to postmastectomy pain syndrome (PMPS), which occurs in at least 20–68% of patients, yet it is often not identified as such (American Cancer Society. 2012; Vilholm, Cold, Rasmussen, and Sindrup, 2008). There is no standard definition for PMPS, however the International Association for the Study of Pain (IASP) has defined this pain as that persisting beyond the normal healing time of 3 months (IASP, 1986). While PMPS is a recognized complication of breast surgery, little is known about the long-term outcome of this chronic pain condition (MacDonald et al., 2005). Furthermore, the exact mechanism by which this pain syndrome develops is unknown, however, it likely is a chronic neuropathic condition due to damaged nerves in the chest wall and/or axilla during surgery.
Pain Anxiety
Pain is a multidimensional experience that can be influenced by a number of individual factors, which in turn, can strongly affect a patient’s subjective adaptation to pain (Bishop and Warr, 2003). One such factor is pain anxiety, which is a central construct of fear-avoidance models (e.g., Vlaeyen and Linton, 2000). Specifically, fear–anxiety–avoidance models of chronic pain emphasize pain-related anxiety as a key diathesis in both the development and maintenance of chronic pain (Asmundson and Taylor, 2006). Also, fear–anxiety–avoidance models of chronic pain involve patterns similar to anxiety disorder models; anxiety disorders either follow from, or are exacerbated by unpleasant experiences associated with behavioral avoidance, catastrophic cognitions, and major distress (Vlaeyen and Linton, 2000). To date, one published study has investigated the effects of a mindfulness-based intervention on pain anxiety in women with breast cancer. The data showed a significant decrease in pain-related anxiety scores pre-to-post (Tacón, 2011).
Pain Catastrophizing
Another factor that influences pain is pain catastrophizing. Pain catastrophizing (PC) is a cognitive-affective pattern characterized by a preoccupation with pain as well as a set of appraisals about the meaning of pain experiences (Sullivan, Bishop, and Pivik, 1995). Pain catastrophizing, as a multi-dimensional construct is defined as “an exaggerated negative mental response to pain consisting of rumination (continued focus on the pain), magnification (tendency to exaggerate the consequences of pain), and helplessness” (Sullivan et al., 1995, p. 526).Catastrophizing plays a central role in the fear-avoidance model of chronic pain because it is viewed as the cognitive route through which fear of pain develops (Vlaeyen, Kole-Snijders, Boeren, and van Eek, 1995); also, this negative perspective accounts for 7–31% of the variance in pain severity (Sullivan et al., 2001). Thus, addressing such cognitive distortions through complementary interventions may interfere with or interrupt the fear-avoidance cycle and benefit those in pain. In cancer pain, catastrophizing is associated with higher negative affect, greater pain intensity, and increased pain behaviors (Schroevers, Kraaij, and Garnefski, 2008). It is likely that individuals experiencing pain may appraise pain experiences as a significant threat, which biases their attention to focus directly on the pain. Moreover, negative emotions typically are viewed as resulting from catastrophizing which serves to increase distress in patients already depleted with suffering from their condition (Michael and Burns, 2004). One published MBSR intervention study that investigated mindfulness effects on pain anxiety in a group of women with breast cancer reported a significant decrease in pain castastrophizing scores pre-to-post the eight-week program (Tacón, 2011).
Symptoms of Distress
Symptom distress is a subjective interpretation of a lived, personal experience with a uniquely given set of symptoms for an individual patient, and it must be kept in mind that the most salient symptoms presented are not automatically the most distressing (McCorkle and Young, 1978). As mentioned earlier, co-morbid symptoms are common to the disease course of cancer and can occur before diagnosis, during treatment and continue through recovery. According to McCorkle and Young, symptoms are subjective phenomena indicating a condition departing from normal function, sensation or appearance (1978). The subjective nature of these phenomena, undoubtedly, is the reason that individual reports of distress symptoms vary and have such wide ranges of frequency and severity. Subjective physical symptoms are usually associated with appearance, appetite, bowel patterns, breathing, fatigue, nausea, and pain; moreover, visible signs typically consist of diarrhea, hair loss, vomiting and weight loss (e.g., Dalal, Del Fabbro, and Bruera, 2006)). Of clinical significance is the relationship between symptoms and outcomes; that is, symptoms of distress may be important predictors of patient outcomes (McCorkle, 1987). A single MBSR study has investigated the program’s effectiveness in reducing the global or overall score for symptoms as defined by McCorkle’s Symptoms of Distress Scale (SDS) developed for cancer patients (McCorkle and Young, 1978).
The most well-documented symptom cluster associated with cancer is the combination of pain, fatigue, and sleep disturbance (Hoffman et al., 2007). Pain and cancer-related fatigue (CRF) are two common symptoms that mutually influence each other, for pain depletes one’s energy which further reduces resources for dealing with pain. Pathologic, debilitating fatigue, which can arise from physical and psychological stressors (Portenoy and Itri, 1999), negatively and severely impacts a patient’s quality of life. CRF severely affects over 75 percent of cancer patients due not only to the disease process, but also, to cancer treatment (Komurcu, 2000; Portenoy and Itri, 1999). Moreover, the end of treatment does not automatically mean the end of fatigue; cancer survivors report that chronic fatigue may last for months or even years after treatment is completed (Portenoy and Itri, 1999). Previous MBSR studies with cancer patients have used fatigue scores as measured by the Profile of Moods (POMS) subscale (e.g., Carlson and Garland, 2005; Speca, Carlson, Goodey, and Angen, 2000).
While fatigue was not a specific focus of Speca and colleagues (2000), Carlson and Garland (2005) reported a significant improvement in both fatigue and sleep disturbance among cancer patients who participated in an eight-week MBSR intervention. Lastly, another MBSR intervention study by Kieviet-Stijnen et al.(2008) in patients with various types of cancer, measured multiple symptoms including fatigue by the Rotterdam Symptom Checklist (de Haes, van Knippenberg, and Neijt, 1990) found no within-group improvement in fatigue. Due to the relationship between pain and fatigue, fatigue is a symptom of import in this mindfulness study.
Mindfulness Meditation
Mindfulness meditation, such as Kabat-Zinn’s secular eight-week program that originated at the University of Massachusetts Medical Center, is an example of inclusive meditation that involves including rather than excluding stimuli from the field of consciousness (Kabat-Zinn, 1990). Basically, meditation is the disciplined practice of paying attention to the present moment with uncritical, non-judging acceptance. This discipline fosters detached, nonjudgmental observation or witnessing of thoughts, perceptions, sensations, and emotions, which provides a means of self-regulating one’s arousal and awareness. Mindfulness-Based Stress Reduction (MBSR) programs have demonstrated beneficial effects in multiple health populations such as cancer, chronic pain, and heart disease (see Shigaki, Glass, and Schopp, 2006).
Mindfulness and Cancer
Multiple literature reviews exist regarding MBSR effects in cancer populations (i.e., Matchin and Armer, 2007; Matchim, Armer, and Stewart, 2011; Musial et al., 2011). Data indicate that the MBSR is effective in significantly reducing stress levels and symptoms, scores for anxiety and depression, and insomnia in cancer patients (Carlson and Garland,2005; Speca, Carlson, Goodey, and Angen, 2000; Tacón, Caldera, and Ronaghan, 2004, 2005). Furthermore, MBSR interventions in those with cancer have found significant improvements pre-post in quality of life, positive mood shifts, improved coping and mental adjustment to cancer, and health locus of control (Tacón, 2006; Tacón, Caldera, and Ronaghan, 2004, 2005). Despite abundant mindfulness research indicating significant and beneficial outcomes with cancer patients, a paucity of literature exists as to the effects of mindfulness interventions specifically on pain-related factors in this population. Two studies specifically investigated MBSR intervention effects on pain intensity in breast cancer patients, which showed significant decreases in scores before and after the interventions (Tacón, 2006, 2011). Most investigations have focused on outcomes such as stress levels and symptoms, depression and anxiety or coping (e.g., Speca et al., 2000). Thus, similar to an absence of mindfulness studies in general regarding pain reduction, one published study exists as to the effects of the MBSR on pain anxiety and pain catastrophizing in women with cancer (Tacón, 2011).
The aims of the present study were to investigate and/or replicate the effects of an MBSR intervention in women diagnosed with breast cancer on the following factors: pain anxiety, pain catastrophizing, and overall symptoms of cancer distress. Lastly, an interest of this study is cancer-related fatigue, which will be assessed by a standardized fatigue instrument. Previous MBSR studies with cancer patients have used fatigue scores as measured by the Profile of Moods (POMS) subscale (e.g., Carlson & Garland, 2005). Based on limited findings, it was hypothesized that significant improvements would be found pre-post scores for pain anxiety and catastrophizing, overall symptoms of cancer distress and fatigue.
Method
Following Human Subjects Approval, participants were recruited through medical facilities by fliers, media advertisements, and referrals from physicians and the American Cancer Society in a southwestern community of approximately 200,000 residents. Eighty-five women diagnosed with breast cancer were approached about participating in this study, yet only 57 women agreed to participate. The final sample consisted of 57 participants, of which, the majority suffered chronic pain from initial surgical treatment with a mean age of 54 years. The majority were post adjuvant therapy (83%) Stage I consisting of chemotherapy and radiation; six women had metastatic disease (11%) Stage II; and the remaining participants (6%) were survivor status, see Table 1. The majority were Protestant (96%), Caucasian (86%), and married (78%), with a modal family income between $35,000 and $77,999 (57%), and a beyond-high-school education level (79%). Less than half of the sample (46%) worked outside the home part-time. Seven women (12%) indicated a family history of cancer. Individuals with cancer-related pain were defined as patients with a diagnosis of cancer experiencing pain from direct tumor involvement and/or a form of cancer treatment,” (Bruera and Kim, p. 2477), which was confirmed by the attending oncologist . Time from diagnosis ranged from nine-months to six years at the time of the study.
Table 1. Participant Cancer Status

Exclusion criteria included: no cancer associated pain or chronic pain status, current primary sites other than breast, less than 18 years of age, and psychopathology. Initially, potential participates contacted the investigator by phone for early screening, during which time, a standard script was followed with probes as needed. A second screening and standardized interview occurred, at which time the investigator described the proposed study and expectations for participation. Assurances of confidentiality, anonymity, and the right to withdraw at any time were provided. Once consent forms were signed at interview, questionnaires were completed at that time. Individuals displaying psychopathology (i.e., psychotic symptoms or suicidal ideation) were referred to appropriate healthcare services. All participants maintained their standard medical care during the program.
The modified MBSR program of Kabat-Zinn (1990) was held in a counseling center for 1.5 hours/week over eight-weeks which did not include the standard one-day retreat. Two groups were trained by a facilitator with 14 years’ experience conducting MBSRs as well as a mindfulness-trained assistant facilitator. Participants were trained in the mindfulness practices of: body scan, sitting meditation, hatha yoga, and walking meditation. The body scan involves a gradual sweeping of attention through-out the entire body with non-critical acceptance of sensations or feelings, and suggestions of breath awareness and relaxation. Sitting meditation involves mindful attention of the breath and nonjudgmental awareness of distractions. Hatha yoga involves simple stretches and postures to develop mindful movement of the body or meditation in motion. Walking meditation involves walking mindfully while paying attention to all sensations. Participants received compact discs to facilitate daily homework of the learned techniques.
Weekly homework sheets, distributed to the participants in binder form, were turned in each week to indicate the amount of homework conducted for each mindfulness technique daily. At the end of the intervention program, participants again completed questionnaires.
The Pain Anxiety Symptoms Scale-20 (PASS-20) was used to measure pain-related anxiety (McCracken and Dhingra, 2002). The PASS-20 is a 20-item measure developed as a short-form of the original 40-item measure (McCracken and Gross, 1993; McCracken, Zayfert, and Gross, 1992), and has been used in previous cancer samples (i.e., Gauthier et al., 2009). The PASS-20 measures fear of pain indirectly via pain-related anxiety (e.g., Pain seems to cause my heart to pound or race), rather than directly (Carleton and Asmundson, 2009). Each item is responded to using a 6-point Likert scale from 0 (never) to 5 (always); scores range between 0–100 with higher scores indicating greater levels of anxiety.
The PASS-20 is consists of four distinct components of pain-related anxiety: (1) cognitive anxiety (e.g., I can’t think straight when in pain); (2) pain-related fear (e.g., Pain sensations are terrifying); (3) escape and avoidance (e.g., I try to avoid activities that cause pain), and; (4) physiological anxiety (e.g., Pain makes me nauseous). The PASS-20 is internally consistent (α = .81), and correlates highly, r = .95, with the original version. In sum, the reliability and validity of the PASS-20 are well established (McCracken and Dhingra, 2002). Pain catastrophizing, operationally defined as “an exaggerated negative mental response to pain consisting of rumination (continued focus on the pain), magnification (tendency to exaggerate the consequences of pain), and helplessness,” was measured by the Pain Catastrophizing Scale (Sullivan et al., 1995, p. 526). This 13-item scale, used in previous cancer samples (i.e., Bishop and Warr, 2003), contains a 0 (not at all) to 4 (all the time) Likert- scale with rumination, magnification, and helplessness sub-scales. PC is considered to have a continuous distribution in the population without a clear cut-off level that distinguishes between high or low catastrophizers (Sullivan et al., 2001). Here, a total catastrophizing score was calculated from the sum of all items with higher scores indicating greater levels of catastrophizing. Good psychometric properties of construct validity and reliability in both clinical and non-clinical samples have been demonstrated (Osman et al., 2000; Sullivan et al., 1995).
Symptoms of distress or discomfort associated with cancer were measured by the 10-item version of the Symptom Distress Scale (SDS) developed for use with cancer patients (McCorkle and Young, 1978). Specific symptoms assessed are: nausea, loss of appetite, insomnia, pain, mobility, bowel pattern, fatigue, lack of concentration, changes in appearance, and mood state (20). Each symptom is measured on a Likert-like scale ranging from 1 (no/minimum distress) to 5 (most/maximum distress). The 10 responses are summed to provide a total distress score of symptoms. The SDS has documented validity and reliability (McCorkle and Young, 1978). Lastly, fatigue was measured specifically by the nine-item Brief Fatigue Inventory (BFI), a measure designed to rapidly assess cancer-related fatigue (Mendoza et al., 1999). Patients are asked to rate, on a scale of 0 (none) to 10 (severe), their current level of fatigue, usual fatigue level in the last 24 hours, worst level of fatigue in the last 24 hours, and how fatigue has interfered with: general activity, mood, walking, work, relationships, and life enjoyment. A global fatigue score is obtained by averaging all the items on the BFI with scores ranging from 0 to 10, and higher scores indicating greater fatigue; specifically, score ranges for mild fatigue are (1-3), moderate fatigue (4-6), and severe fatigue (7-10).
This instrument has reported good internal consistency with cronbach alpha reliability ranging from 0.82 to 0.97 (Mendoza et al., 1999).
Results
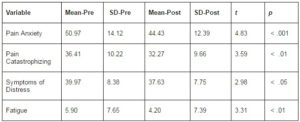
Paired t-test analyses were conducted to assess pre-and-post changes for each outcome variable.
See Table 2.
Table 2. Means and Standard Deviations for Dependent Variables
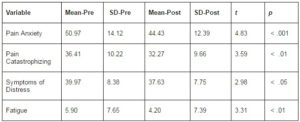
Pain Anxiety and Catastrophizing
The total scores on the PASS -20 were used in analysis of scores at baseline and post-intervention. Baseline scores prior to the intervention (M = 50.97, SD = 14.12) significantly dropped following completion of the intervention (M = 44.43, SD = 15.39), (t = 4.83, p. < .001). The results for this group of women showed significant improvement pre-to-post-intervention on pain anxiety, thus supporting the hypothesis. Total scores on the PCS were used in analysis of scores at baseline and post-intervention. Significant changes in a positive direction occurred between baseline scores (M = 36.41, SD = 10.22) to scores after the end (M = 32.27, SD = 12.66) of the MBSR (t = 3.59, p. < .01). This indicates that the women in this group had a significant decrease in the cognitive process of negatively focusing on pain in the form of catastrophizing about future pain after completing the mindfulness-based intervention. The hypothesis was supported.
Symptoms of Cancer Distress and Fatigue
Total or global scores on the SDS for symptoms of cancer distress were used for the analyses.
Results indicated a decrease in the scores for this group of women from pre-intervention (M =39.97, SD = 8.38) to the post-intervention period (M =37.63, SD = 7.75). This change was significant (t = 2.98, p < .01). Scores for cancer distress symptoms significantly decreased post-intervention as predicted.
Finally, fatigue scores as measured by the BFI decreased significantly from baseline (M = 5.90, SD = 7.65) to post-intervention (M = 4.20, SD = 7.39), t = 3.31, p. < .01).
Discussion
The purpose of this study was to investigate mindfulness or present moment effects on pain anxiety and pain catastrophizing, symptoms of distress, and fatigue in women with breast cancer. Significant decreases in pain anxiety and pain catastrophizing scores were found from baseline to the end of theintervention eight-weeks later. This is consistent with previous findings from a single published study (Tacón, 2011). It can be argued that anxiety and catastrophizing about one’s pain is the opposite of mindfulness—an intentional and flexible self-regulation of present moment awareness with acceptance of each moment as it—without judgment or attaching a negative bias to one’s experience. Mindful awareness is flexible without conceptual processing (Bishop et al, 2004). Thus, mindfulness, being present-centered with non-judgmental acceptance of the present moment, is conceptually and theoret-ically incongruent with a non-now focus and conceptual processing with the negative bias toward pain such as is involved in anxiety and catastrophizing (Sullivan, Lynch, and Clark, 2005). Moreover, recent hierarchical multiple regression analyses were conducted on data from a heterogeneous sample of chronic pain patients in order to investigate the role of mindfulness in the fear-avoidance model of chronic pain (Schütze, Rees, Preece, and Schütze, 2010). The data revealed that mindfulness not only predicted pain catastrophizing when other variables were controlled, but also moderated the relationship between pain intensity and pain catastrophizing. Based on these results, researchers presented a revised fear-avoidance model of chronic pain that included mindfulness (Schütze et al., 2010). These findings lend support that suggestion.
Having the disease of cancer typically means suffering with co-morbid symptoms that, by their very nature, may be distressing, yet are magnified severely in the context of cancer. Thus, the cancer patient must deal with added layers of subjective suffering from symptoms usually associated with this disease process and its treatment. For example, such distressing and primarily physical symptoms may involve the presence of or changes in appearance, appetite, bowel patterns, breathing, fatigue, nausea, and pain (e.g., Dalal, Del Fabbro, and Bruera, 2006). These co-morbid symptoms associated with cancer are clinically important because they are thought to be important predictors of outcomes for cancer patients (McCorkle, 1987). In this study, a symptoms of distress score was derived from the symptoms of distress scale for cancer patients by McCorkle and Young (1978) that measures multiple symptoms and provides a global distress score. The data showed a significant decrease in pre-to-post scores for overall symptom distress in this group of women. These findings replicate the previous single MBSR study to date that investigated intervention effects on these symptoms using the same measure, and reported a significant reduction in global symptom distress scores.
As previously mentioned, the most well-documented and studied symptom cluster associated with this disease is pain, fatigue, and sleep disturbance (Hoffman et al., 2007). Sleep disturbance was beyond the scope of this study, yet the relation between pain and fatigue was a specific focus.
Specifically, pain and debilitating cancer-related fatigue (CRF) are two common symptoms that influence each other, and can compromise a patient’s quality of life; that is, pain depletes one’s energy, which further reduces a patient’s resources for dealing and living with pain. Chronic fatigue also may last years after treatment has ended (Portenoy and Itri, 1999).Thus, fatigue was a specific symptom of import here because of the relation between pain and fatigue as well as the fact the majority of previous MBSR studies with cancer patients measured fatigue by the Profile of Moods (POMS) subscale (e.g., Carlson and Garland, 2005; Speca, Carlson, Goodey, and Angen, 2000). This study chose the Brief Fatigue Inventory (Mendoza et al., 1999), which specifically was designed to assess cancer-related fatigue. Results showed that fatigue scores decreased significantly by the end of the intervention, indicating positive present moment effects as measured by this cancer-related fatigue instrument. While the hypothesis was supported, further research should continue to explore mindfulness effects by expanding the use of—rather than narrowing the use or selection of—- assessment measures.
Limitations must to be acknowledged. First, this study dealt with women with breast cancer, therefore findings cannot be generalized to other chronic or life-threatening disease populations such as cardiovascular disease, or other oncology populations. Secondly, another limitation involves the passage of time. The eight weeks of intervention may have played a role in the findings, for this time period, itself, may have been significant for the continuing adjustment of these participants, regardless of the intervention applied. Next, the participants were primarily Caucasian, which begs the question about how results would differ in women of different ethnic origins. Lastly, participants were not randomly assigned to multiple treatment conditions.
In conclusion, this study adds to the paucity of literature as to the efficacy of present moment or mindfulness effects on pain factors in those with cancer. Findings indicate that studies involving randomized conditions appear feasible. The bottom line is that individuals living with a life-threatening disease need complementary medicine options other than narcotics to help them deal with their pain and suffering.
(adsbygoogle = window.adsbygoogle || []).push({});
References
American Cancer Society. (2012). Cancer Facts and Figures: 00202012. http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-032010.pdf, 2012
Publisher
American Cancer Society. (2012). http://www.sharecare.com/question/what-is-post-mastectomy-pain-syndrome
Publisher
Asmundson, G. J. G. & Taylor, S. (2006). “PTSD and Chronic Pain: Cognitive-Behavioral Perspectives and Practical Implications,” Causality: Psychological Knowledge and Evidence in Court, Springer, New York, NY, 225–241.
Publisher – Google Scholar
Bishop, S., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., Et Al. (2004). “Mindful-Ness: A Proposed Operational Definition,” Clinical Psychology: Research and Practice, 11, 230–241.
Publisher – Google Scholar – British Library Direct
Bishop, S. R. & Warr, D. (2003). “Coping, Catastrophizing and Chronic Pain in Breast Cancer,” Journal of Behavioral Medicine, 26, 265–281.
Publisher – Google Scholar – British Library Direct
Blasco, A., Berzosa, M., Iranzo, V. & Camps, C. (2009). ‘Update in Cancer Pain,’ Cancer Chemotherapy Review, 4, 95-109.
Google Scholar
Bruera, E. & Kim, H. N. (2003). “Cancer Pain,” Journal of the American Medical Association, 290, 2476–2479.
Publisher – Google Scholar – British Library Direct
Carleton, R. N. & Asmundson, G. J. G. (2009). “The Multidimensionality of Fear of Pain: Construct Independence for the Fear of Pain Questionnaire-Short form and the Pain Anxiety Symptoms Scale-20,” Journal of Pain, 10, 29–37.
Publisher – Google Scholar
Carlson, L. E. & Garland, S. N. (2005). “Impact of Mindfulness-Based Stress Reduction (MBSR) On Sleep, Mood, Stress and Fatigue Symptoms in Cancer Outpatients,” International Journal of Behavioral Medicine, 12, 278-286.
Publisher – Google Scholar – British Library Direct
Cimprich, B. (1999). “Pretreatment Symptom Distress in Women Newly Diagnosed with Breast Cancer,” Cancer Nursing, 22, 185-194.
Publisher – Google Scholar – British Library Direct
Dalal, S., Fabbro, E. D. & Bruera, E. (2006). “Symptom Control in Palliative Care–Part I: Oncology as a Paradigmatic Example,” Journal of Palliative Medicine, 9, 391-408.
Publisher – Google Scholar – British Library Direct
De Haes, J. C., Van Knippenberg, F. C. & Neijt, J. P. (1990). “Measuring Psychological and Physical Distress in Cancer Patients: Structure and Application of the Rotterdam Symptom Checklist,” British Journal of Cancer, 62, 1034-1038.
Publisher – Google Scholar
Dodd, M. J., Miaskowski, C. & Paul, S. M. (2001). “Symptom Clusters and Their Effect on the Functional Status of Patients with Cancer,” Oncology Nursing Forum, 28, 465–470.
Publisher – Google Scholar – British Library Direct
Esper, P. & Heidrich, D. (2005). “Symptom Clusters in Advanced Illness,” Seminars in Oncology Nursing, 21, 20–28.
Publisher – Google Scholar
Gauthier, L., Rodin, G., Zimmermannc, C., Warrd, D., Moored, M., Shepherdd, F. & Gagliesea, L. (2009). “Acceptance of Pain: A Study in Patients with Advanced Cancer,” Pain, 143, 147-154.
Publisher – Google Scholar
Hoffman, A. J., Given, B. A., von Eye, A., Gift, A. G. & Given, C. W. (2007). “Relationships among Pain, Fatigue, Insomnia, and Gender in Persons with Lung Cancer,” Oncology Nursing Forum, 34, 785-792.
Publisher – Google Scholar – British Library Direct
International Association for the Study of Pain (IASP). (1986). “Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms,” Pain, 3, S1–S226.
Publisher – Google Scholar
Kabat-Zinn, J. (1990). Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. Dell, New York, NY.
Publisher – Google Scholar
Kieviet-Stinjnen, A., Visser, A., Garssen, B. & Hudig, W. (2008). “Mindfulness-Based Stress Reduction Training for Oncology Patients: Patients’ Appraisal and Changes in Well-Being,” Patient Education and Counseling, 72, 436-442.
Publisher – Google Scholar
Komurcu, S., Nelson, K. A., Walsh, D., Donnelly, S. M., Homsi, J. & Abdullah, O. (2000). “Common Symptoms in Advanced Cancer,” Seminars in Oncology, 27, 24–33.
Publisher – Google Scholar – British Library Direct
Macdonald, L., Bruce, J., Scott, N. W., Smith, W. C. S. & Chambers, W. A. (2005). “Long-Term Follow-Up of Breast Cancer Survivors with Post-Mastectomy Pain Syndrome,” British Journal of Cancer, 92(2), 225–230.
Publisher – Google Scholar
Matchim, Y. & Armer, J. M. (2007). “Measuring the Psychological Impact of Mindfulness Meditation on Health among Patients with Cancer: A Literature Review,” Oncology Nursing Forum, 34, 1059-1066.
Publisher – Google Scholar – British Library Direct
Matchim, Y., Armer, J. M. & Stewart, B. R. (2011). “Mindfulness-Based Stress Reduction among Breast Cancer Survivors: A Literature Review and Discussion,” Oncology Nursing Forum, 38, E61-71.
Publisher – Google Scholar
McCorkle, R. (1987). “The Measurement of Symptom Distress,” Seminars in Oncology Nursing, 3, 248-256.
Publisher – Google Scholar
McCorkle, R. & Quint-Benoliel, J. (1983). “Symptom Distress, Current Concerns and Mood Disturbance after Diagnosis of Life-Threatening Disease,” Social Science and Medicine, 17, 431-438.
Publisher – Google Scholar
McCorkle, R. & Young, K. (1978). “Development of a Symptom Distress Scale,” Cancer Nursing, 1, 373-378.
Publisher – Google Scholar
McCracken, L. M. & Dhingra, L. (2002). “A Short Version of the Pain Anxiety Symptoms Scale (PASS-20): Preliminary Development and Validity,” Pain Research Management, 7, 45–50.
Publisher – Google Scholar – British Library Direct
McCracken, L. M. & Gross, R. T. (1993). “Does Anxiety Affect Coping with Chronic Pain?,” Clinical Journal of Pain, 9, 253-259.
Publisher – Google Scholar – British Library Direct
McCracken, L. M., Zayfert, C. & Gross, R. T. (1992). “The Pain Anxiety Symptom Scale: Develop-Ment and Validation of a Scale to Measure Fear of Pain,” Pain, 50, 67–73.
Publisher – Google Scholar
Mendoza, T. R., Wang, X. S., Cleeland, C. S., Morrissey, M., Johnson, B. A., Wendt, J. K. & Huber, S. L. (1999). “The Rapid Assessment of Fatigue Severity in Cancer Patients: Use of the Brief Fatigue Inventory,” Cancer, 85, 1186-1196.
Publisher – Google Scholar – British Library Direct
Michael, E. S. & Burns, J. W. (2004). “Catastrophizing and Pain Sensitivity among Chronic Pain Patients: Moderating Effects of Sensory and Affect Focus,” Annals of Behavioral Medicine, 27, 185–194.
Publisher – Google Scholar
Musial, F., Bussing, A., Heusser, P., Choi, K. E. & Ostermann, T. (2011). “Mindfulness-Based Stress Reduction for Integrative Cancer Care: A Summary of Evidence,” Forsch Komplementmed, 18, 192-202.
Publisher – Google Scholar
National Cancer Institute. (1997). ‘Cancer Facts,’ American Cancer Society, Washington, D.C.
Osman, A., Barrios, F. X., Gutierrez, P. M., Kopper, B. A., Merrifield, T. & Grittmann, L. (2000). “The Pain Catastrophizing Scale: Further Psychometric Evaluation with Adult Samples,” Journal of Behavioral Medicine, 23, 351–365.
Publisher – Google Scholar – British Library Direct
Portenoy, R. K. (2005). ‘Cancer Pain Management,’ Clinical Advances in Hematological Oncology, 3, 30-32.
Portenoy, R. K. & Itri, L. M. (1999). “Cancer-Related Fatigue: Guidelines for Evaluation and Management,” Oncologist, 4,1–10.
Publisher – Google Scholar
Schroevers, M., Kraaij, V. & Garnefski, N. (2008). “How Do Cancer Patients Manage Unattainable Personal Goals and Regulate Their Emotions?,” British Journal of Health Psychology, 13, 551–562.
Publisher – Google Scholar
Schütz, R., Rees, C., Preece, M. & Schütze, M. (2010). “Low Mindfulness Predicts Pain Catastro-Phizing in a Fear-Avoidance Model of Chronic Pain,” Pain, 148, 120-127.
Publisher – Google Scholar
Shigaki, C. L., Glass, B. & Schopp, L. H. (2006). “Mindfulness-Based Stress Reduction in Medical Settings,” Journal of Clinical Psychology in Medical Settings, 13, 209-216.
Publisher – Google Scholar – British Library Direct
Speca, M., Carlson, L. E., Goodey, E. & Angen, M. (2000). “A Randomized, Wait-List Controlled Clinical Trial: The Effect of a Mindfulness Meditation-Based Stress Reduction Program on Mood and Symptoms of Stress in Cancer Outpatients,” Psychosomatic Medicine, 62, 613–622.
Publisher – Google Scholar – British Library Direct
Sullivan, M. J. L., Bishop, S. R. & Pivik, J. (1995). “The Pain Catastrophizing Scale: Development and Validation,” Psychological Assessment, 7, 524–532.
Publisher – Google Scholar – British Library Direct
Sullivan, M. J. L., Lynch, M. E. & Clark, A. J. (2005). “Dimensions of Catastrophic Thinking Associated with Pain Experience and Disability in Patients with Neuropathic Pain Conditions,” Pain, 113, 310–315.
Publisher – Google Scholar
Sullivan, M. J. L., Thorn, B., Haythornthwaite, J. A., Keefe, F., Martin, M., Bradley, L. A. & Lefebvre, J. C. (2001). “Theoretical Perspectives on the Relation between Catastrophizing and Pain,” Clinical Journal of Pain, 17, 52-64.
Publisher – Google Scholar – British Library Direct
Tacón, A. M. (2006). “Mindfulness Effects on Symptoms of Distress in Women with Cancer,” Journal of Cancer Pain and Symptom Palliation, 2, 17-22.
Publisher – Google Scholar
Tacón, A. M. (2011). “Mindfulness, Cancer, and Pain,” Alternative Medicine Studies, 1, E15-E20.
Publisher – Google Scholar
Tacón, A. M., Caldera, Y. M. & Ronaghan, C. (2004). “Mindfulness-Based Stress Reduction in Women with Breast Cancer,” Families, Systems, and Health, 22, 193–203.
Publisher – Google Scholar – British Library Direct
Tacón, A. M., Caldera, Y. M. & Ronaghan, C. (2005). “Mindfulness, Psychosocial Factors and Breast Cancer,” Journal of Cancer Pain and Symptom Palliation, 1, 45-54.
Publisher – Google Scholar
Vlaeyen, J. W. S., Kole-Snijders, A. M. J., Boeren, R. G. B. & van Eek, H. (1995). “Fear of Movement Injury in Chronic Low Back Pain and its Relation to Behavioral Performance,” Pain, 62, 363–372.
Publisher – Google Scholar
Vlaeyen, J. W. S. & Linton, S. J. (2000). “Fear-Avoidance and its Consequences in Chronic Musculo-Skeletal Pain: A State of the Art,” Pain, 85, 317–332.
Publisher – Google Scholar
Vilholm, O. J., Cold, S., Rasmussen, L. & Sindrup, S. H. (2008). “The Postmastectomy Pain Syndrome: An Epidemiological Study on the Prevalence of Chronic Pain after Surgery for Breast Cancer,” British Journal of Cancer, 99(4), 604–610.
Publisher – Google Scholar
Wells, N., Murphy, B., Wujcik, D. & Johnson, R. (2003). “Pain-Related Distress and Interference with Daily Life of Ambulatory Patients with Cancer with Pain,” Oncology Nursing Forum, 30, 977–986.
Publisher – Google Scholar – British Library Direct