Introduction
It well is recognized and documented that malignant tumor of oral cavity invading mandibular bone require partial or total mandibulectomy in order to provide adequate margins. To predict the range of malignant tumor invasion into the mandible preoperatively is very important for clinician. Exactly preoperative assessment the extent of mandibular invasion by malignant tumor is very important to ensure getting a safe tissue margin, Gu, D.H. et al (2010) thought it could reserve most well-being bone tissue, and it is significance to patien’s prognosis. Ljungberg, M. (2011) hought SPECT (Single photon emission computed tomography) was functional imaging modality, high sensitivity, but lack the structural delineation. So it is difficult to accurate locate focus. Perren, E. (2011) thought CT (Computered Tomography) was anatomical imaging modality, provides accurate morphological information necessary for tumor localization and detection of structural abnormalities, but can not reflect the functional or metabolic activity of the tumor. Goerres, G.W. et al (2005) mentioned the coregistration of structural (CT) and functional (SPECT) imaging information can improve the identification of bone invasion. But the value of SPECT/CT to determine the extent of malignant tumour invading mandibule had not be reported.
The aim of this study was to compare the accuracy of SPECT/CT and helical CT to determine the extent of mandibular invasion by moderately differentiated squamous cell carcinoma of the oral cavity, and to evaluate SPECT/CT’s diagnostic value in determining the extent of mandibule invasion by moderately differentiated squamous cell carcinoma of oral cavity and hope to provide guidance for surgeon.
Materials and Methods
Materials
Main Instruments
Lightspeed16 spiral CT (GE Co, American); Millennium VG (Haw Keye) SPECT/CT fusion imaging system (GE Co, American); 99mTc generator (Beijing atom high technology Co, China).
Main Experiment Agentia
MDP (methylene diphosphonate) kit (Beijing Shihong medicine development centre, China); 99mTc-MDP photographic developer.
Patients
This study had local ethics committee approval, and all patients gave written informed consent.51 patients with moderately differentiated squamous cell carcinoma of the oral cavity were investigated, they were determined underwent SPECT/CT fusion imaging and CT scan that the mandibular invision by squamous cell carcinoma in the Department of Oral & Maxillofacial Sugery of the Affiliated Hospital of Qingdao University Medical College from 2003.10 to 2009.3.The samples consisted of 34 men and 19 women (mean age, 49.24±10.1 years ;range, 28-71 years). In order to study more precise, this research only investigated candidates of mandibular segmental or total mastectomy. Tumor staging on the results of this study have little effect, so clinical staging information was ignored.
Methods
Clinical Procedure
All the patients underwent SPECT/CT and CT within 1 week before surgery. then they were treated with complete or near complete surgical resections of the tumor, which were determined by the surgeon based on the clinical, imaging, intraoperative, and fast-frozen histologic findings. The results of SPECT /CT and CT scan were compared to the results of histopathology findings which was considered as the reference standard.
Imaging
740- 1100 Mbq of technetium-99m methylene diphosphonate (99Tcm MDP) were injected intravenously, then acquisitions were obtained 21/2 h later (±30 min) using a low energy all purpose collimator through SPECT/CT fusion imaging system. This hybrid imaging system combines a dual-detector, variable angle gamma camera with a low-dose x-ray tube that is attached to the same rotating gantry as the gamma camera. This device provides, together with SPECT data, cross-sectional x-ray transmission images that accurately locate the anatomical sites of radiotracer accumulations. Moreover, the gamma camera is capable of MDP imaging using coincidence detection.
For acquiring the transmission data, the x-ray tube and linear detector array rotate together around the patient in a fixed geometry, with a single slice imaged in 14 seconds. Multiple transmission slices are obtained by moving the table, the full field of view consists of 40 slices with the slice thickness fixed at 1 cm. At the completion of the first type of acquisition (transmission or emission), the patient is automatically repositioned so that the 40-cm axial field that was just scanned matches the 40-cm axial field of view of the second imaging modality. Images are reconstructed in the workstation and transmission data are integrated in the nuclear medicine database, the alignment of slices is automatically performed, then matching pairs of x-ray and scintigraphic images are fused generating new images overlying SPECT and CT data. The CT scan were performed in the axial plane with 3-mm-thick contiguous sections from the skull base to the thoracic inlet. All studies were reconstructed with soft-tissue and bone algorithms. The bone algorithm settings were a width of 3500 H and level of 700H.
Image Interpretation
The CT scans were displayed in gray scale and printed on film. Two radiologists viewed the CT scans obtained in all patients with knowledge of the clinical data but without knowledge of the results of the other imaging examinations. The bone and soft-tissue windows were assessed in consensus. Bone invasion was suggested when tumor tissue was visible outside the cortical bone and the cortical bone was seen to be partially eroded or totally destroyed. Two radiologists were asked to mark extent of bone erosion.
The SPECT images were displayed in gray scale, in which dark areas corresponded to regions with increased tracer uptake and bright areas to regions with low or absent tracer uptake. The CT images were assessed by using bone and soft-tissue windows. The SPECT/CT images were displayed with tracer uptake overlaid in color on the CT images. The quality of image coregistration was visually controlled. The window settings were those used to evaluate bone and soft tissues. Two nuclear medicine physicians visually assessed all images on a computer screen. Images were read in consensus and with knowledge of clinical information but without knowledge of the results of other imaging examinations. The mandibular invasion was suggested when tracer uptake abnormalities increase.
Histopathology Examination
The fresh mandibulectomy specimens after the soft tissue was sectioned were fixed in 10% formalin solution and decalcified in 5% nitric acid for a period of 1-4 days. Once the bone had softed, it was cut into 3 mm thick sequential slices in transverse ,every slice was cut into several 1.5mm long sequential smaller slice again, subsequently processed in paraffin wax, one 5 micron section stained with haematoxylin and eosin was examined from each block, with step serial sections examined as necessary. One pathologist who was unaware of the imaging findings carried out pathological examination and measured length of proximal mandibular invasion. The length of the mandible was as the extent of invasion.
Statistical Analysis
Differences among SPECT/CT 、 CT images and histopathology examination were analyzed using the Statistical Package for the Social Sciences (SPSS) version 12.0. Probabilities of <0.05 was considered to indicate a significant difference.
Results
All of the patients, the diagnosis of mandibular invasion by moderately differentiated squamous cell carcinoma were identified underwent pathology.43 patients were with gingival carcinoma, 8 patients with central carcinoma of jaw.
A case of central moderately differentiated squamous cell carcinoma of jaw, CT scan showed no mandibular invasion before surgery (fig. 1), but SPECT/CT scan showed abnormal increase tracer ingestion (“hot area”) in mandible (fig. 2).
Fig.1: A Case of Central Carcinoma of Jaw, CT Scan Showed no Mandibular Invasion before Surgery

Fig. 2: As the Same Case, SPECT/CT Scan Showed Increased Tracer Uptake (“Hot Area”) in Mandible. Which was Carcinoma Invasion Demonstrated Underwent Pathological Examination.
The way mandibular invasion of central carcinoma (outward infiltration) is difference with gingival carcinoma which invade mandibule from cortical bone to bone marrow. So we divided 51 patients into two groups, A group included 43 patients with gingival squamous cell carcinoma, and B group (primary intra-osseous carcinoma) included 8 patients with central carcinoma of jaw.
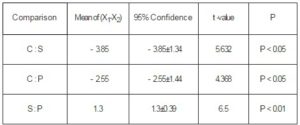
In the A group, the extent of mandibular invasion underwent SPECT/CT was larger 1.02±0.20cm than that determined underwent histopathology examination, and that of CT scan was smaller 1.42±0.35cm than that underwent histopathology examination, while the extent of SPECT/CT scan was larger than that of CT scan 2.44±0.33cm. The difference between SPECT/CT and CT scan was high statistically significant (t=14.44;P<0.01). The difference among histopathology examination、SPECT/CT and CT were high statistically significant too(t=8.0,10.25;P<0.01) (table 1).
Table 1: The Comparison of Bone Invasion Extent with Three Examinations in Group A
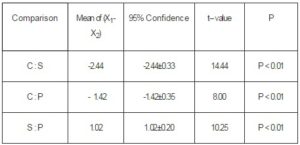
C=CT, S= SPECT/CT, P= histopathology examination
Table 2: The Comparison of Bone Invasion Extent with Three Examinations in Group B
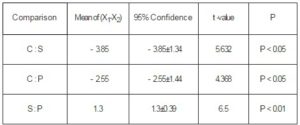
C=CT, S= SPECT/CT, P= histopathology examination
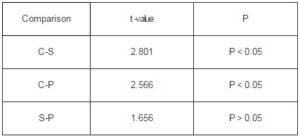
Table 3: The Differential Analysis of Examinations between Group A and Group B
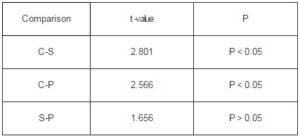
C=CT, S=SPECT/CT, P=histopathology examination
In the B group, the extent of mandibular invasion underwent SPECT/CT scan was larger 1.3±0.39cm than that histopathology examination(t=10.067;P<0.01), and the extent of SPECT/CT scan was larger 3.85±1.3cm than that of CT (t=5.632; P<0.05), while the extent of CT was smaller 2.55±1.44cm than that histopathology examination,they were showed in table 2.
The relationship among the extent of mandibular invasion underwent SPECT/CT 、CT and histopathology examination as follows(S、P and C denote SPECT/CT、histopathology examination and CT respectively, the unit is centimeter:
Group A: ① S=P+1.02±0.20 C=P-1.42±0.35
S=C+2.44±0.33
② S=P+1.02±0.20=C+2.44±0.33
Group B: ① S=P+1.3±0.39 C=P-2.55±1.44
S=C+3.85±1.34
② S=P+1.3±0.39=C+3.85±1.34
Between the two groups, the difference among the three examination methods were showed in table 3. The difference between SPECT/CT with histological examination was not statistical significance(t=1.656,0.446;P>0.05),The difference between SPECT/CT with CT was statistically significance(t=2.801,2.566;P<0.05).
Discussion
The mandibule which invaded by malignant tumor usually is resected In order to complete excise primariy tumor and reduce the tumor recurrence. Assessment of mandibular invasion by malignant tumor is very important for the success of ablative surgery. Oral operation usually results in loss of function and deterioration of cosmetic appearance. How to obtain adequate resection margins? Lewis-Jones, H.G.et al (2000) thought that clear margins meant at least 5mm off the tumour front, Lewis-Jones (2000) and Brown (2002) suggested the depth of tumor invasion mandibule within 5mm tumor can be removed using the method of rim or marginal resection, but a segmental mandibulectomy is required when the depth of invasion is greater than this or in some large soft tissue cancers of the tongue and floor of mouth that were deeply invading the soft tissues and where tumor abutment involved the whole depth of the mandible.
In a research study by Van Cann, E.M.at al (2006) show that a high percentage of resected mandibles in oral cancer no evidence of tumor invasion. So, the preoperative information concerning the extent and depth of bone invasion and as far as possible to conserve well-being bone tissue would be significance to patients’ prognosis. Brown, J.S.et al (2001) put forward it was only parvus article which discussed the extent of tumor invasion mandibule, and the article about using SPECT/CT image fuse technique to determine the extent of mandibule invasion was not yet publicated.
In this reaserch, the author through to the histopathological examination results as a reference, and CT examination for comparison, study accuracy of SPECT/CT in determining the extent mandibular invision. Due to postoperative mandibular specimens shrinkage very little, so this research put it ignored.
CT can provide morphological detail. The definition of structural abnormalities is accurate, but physiologic information is not readily generated. Huntley, T.A.et al (1996) and Rybak, L.D. et al (2001) thought it was at least 30–50% mineral loss in the bone before any change was visible on the CT image. So CT’s sensitivity is low.Mukherji, S.K.et al (2001) thought it’s false-negative rate was high to detect mandibular invasion.
SPECT is functional images which can provide physiological information, his sensitivity is supernal, but it can’t present more anatomy information. So, it can’t accurately locate. SPECT/CT is a kind of registration and fusion image system with a structural image can be valuable as an adjunct to interpretation of functional images, as well as offering the possibility to overcome intrinsic limitations in nuclear medicine image. Image fusion is useful to accurately localize tracer accumulations, to detect occult pathology, to characterize metabolically active lesions, and to draw precisely regions of interest for quantitative studies. This hybrid imaging system combines a dual-detector, variable angle gamma camera with a low-dose x-ray tube that is attached to the same rotating gantry as the gamma camera. Schillaci, O. et al (2004) mentioned, together with SPECT data, cross-sectional x-ray transmission images it could accurately locate the anatomical sites of radiotracer accumulations.
SPECT/CT has high sensitivity, it can discover focus before the mandibule has not morphological change. So on SPECT/CT images the extent of mandibular invision is larger than that on the CT images. So, in this study , the extent on the SPECT/CT images is larger 1.02±0.20cm and 1.3±0.39cm than that the pathological examination identified in A and B group, respectively.
Comparing A and B group, the difference between SPECT/CT and histopathology examination is not statistically significance, but the difference between CT and histopathology examination is statistically significance. It shows that the type of tumor do not obviously influenced on the extent of mandibular invasion underwent SPECT/CT, but the influence is obvious underwent CT. So, SPECT/CT is more superior on showing the extent of mandibular invasion than CT. Some scholars consided that clear margins meant at least 5mm of normal tissue between the tumour front and the edge of the resection.On this view,the extent of mandibular invasion on SPECT/CT image just is the extent that must be resected for completely resecting tumor. Because the type of tumor influence on the extent of mandibular invasion on CT image, the extent of being resected must be on the basis of tumor types. For example, the patients in group A, if we want get clear margin, it is at least 1.21(0.75+0.5)cm of normal tissue between the tumour front and the edge of the resection, While B group, it is 1.77(1.27+0.5)cm .
In conclusion, the extent of mandibular invasion by moderately differentiated squamous cell carcinoma of the oral cavity underwent SPECT/CT fusion imaging is more precise than CT, The result of SPECT/CT can be as guidance for oral surgeon.
(adsbygoogle = window.adsbygoogle || []).push({});
References
Brown, J. S., Kalavrezos, N., D’Souza, J., Lowe, D., Magennis, P. & Woolgar, J. A. (2002). “Factors that Influence the Method of Mandibular Resection in the Management of Oral Squamous Cell Carcinoma,” Br J Oral Maxillofac Surg, 40(4):275-284.
Publisher – Google Scholar – British Library Direct
Brown, J. S. & Lewis-Jones, H. (2001). “Evidence for Imaging the Mandible in the Management of Oral Squamous Cell Carcinoma: A Review,” Br J Oral Maxillofac Surg, 39(6): 411-418.
Publisher – Google Scholar – British Library Direct
Goerres, G. W., Schmid, D. T., Schuknecht, B. & Eyrich, G. K. (2005). “Bone Invasion in Patients with Oral Cavity Cancer: Comparison of Conventional CT with PET/CT and SPECT/CT,” Radiology ,237(1):281-287.
Publisher – Google Scholar – British Library Direct
Gu, D. H., Yoon, D. Y., Park, C. H., Chang, S. K., Lim, K. J., Seo, Y. L., Yun, E. J., Choi, C. S. & Bae, S. H. (2010). “CT, MR, 18 F-FDG PET/CT, and Their Combined Use for the Assessment of Mandibular Invasion by Squamous Cell Carcinomas of the Oral Cavity,” Acta Radiol, 51(10):1111-1119.
Publisher – Google Scholar
Huntley, T. A., Busmanis, I., Desmond, P. & Wiesenfeld, D. (1996). “Mandibular Invasion by Squamous Cell Carcinoma: A Computed Tomographic and Histological Study,” Br J Oral Maxillofac Surg,34(1):69-74.
Publisher – Google Scholar – British Library Direct
Lewis-Jones, H. G., Rogers, S. N., Beirne, J. C., Brown, J. S. & Woolgar, J. A. (2000). “Radionuclide Bone Imaging for Detection of Mandibular Invasion by Squamous Cell Carcinoma,” Br J Radiol, 73(869): 488-493.
Publisher – Google Scholar – British Library Direct
Ljungberg, M. & SjÖGreen-Gleisner, K. (2011). “The Accuracy of Absorbed Dose Estimates in Tumours Determined by Quantitative SPECT: A Monte Carlo Study,” Acta Oncologica, 50(6): 981-989.
Publisher – Google Scholar
Mukherji, S. K., Isaacs, D. L., Creager, A., Shockley, W., Weissler, M. & Armao, D. (2001). “CT Detection of Mandibular Invasion by Squamous Cell Carcinoma of the Oral Cavity,” AJR Am J Roentgenol, 177(1):237-243.
Publisher – Google Scholar – British Library Direct
Perren, E., Potter, M., Golding, S., Shah, K., Fasanmade, A., Bond, S. & Watt-Smith, S. (2011). ‘The Accuracy of MRI and CT Scans in Assessing Mandibular Invasion in Oral SCC,’ British Journal of Oral and Maxillofacial Surgery, 3(49):188 -189.
Google Scholar
Rybak, L. D. & Rosenthal, D. I. (2001). “Radiological Imaging for the Diagnosis of Bone Metastases,” Q J Nucl Med, 45(1):53-63.
Publisher – Google Scholar
Schillaci, O. & Simonetti, G. (2004). “Fusion Imaging in Nuclear Medicine —–Applications of Dual-Modality Systems in Oncology,” Cancer Biother Radiopharm, 19(1):1-10.
Publisher – Google Scholar – British Library Direct
Van Cann, E. M., Oyen, W. J. G., Koole, R. & Stoelinga, P. J. W. (2006). “Bone SPECT Reduces the Number of Unnecessary Mandibular Resections in Patients with Squamous Cell Carcinoma,” Oral Oncol, 42(4): 409-414.
Publisher – Google Scholar