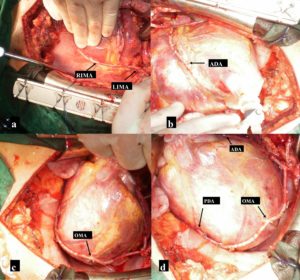
First, we grafted the pedicled LITA to the LAD with an end-to-side anastomosis (Fig. 2 b). Then obtuse marginal branch (OM), and PDA of RCA were anastomosed sequentially with RITA side-to-side and end-to-side respectively (Fig. 2 c y d). All anastomoses were performed with 8-0 Prolenesuture. Rest of the surgical procedure was completed in the usual fashion without complications. Duration of extracorporeal circulation was 83 minutes. Postoperative course and convalescence progressed uneventfully. After ten days of in hospital postoperative care the patient was discharged with evident clinical and hemodynamic recovery. Eighteen months after hospital discharged he was asymptomatic (New York Heart Association Class I, Canadian Cardiovascular Society Class I). Transthoracic echocardiography showed normal function and size of both ventricles. Postoperative multi-slice computed tomographic angiography showed patency of every graft.
Comments
Saphenous vein graft atherosclerosis continues to be the major cause of coronary artery bypass grafting late failure. The use of both internal thoracic arteries for coronary revascularization has been demonstrated to be advantageous over the use of single LIMA in combination with vein grafts with respect to survival, freedom from angina and repeated revascularization procedures. Complete arterial myocardial revascularization is the procedure of choice in young adults and in patients with porcelain aorta. Benefits of complete arterial revascularization are well established as reported in the research by Fiori et al., (1990). When employing composite grafts, arterial flow to the revascularized left ventricular myocardium can be provided exclusively by in-situ LITA. In our patient the LITA flow was over 100 ml per minute. Semiskeletonized, and skeletonized techniques harvesting internal thoracic arteries result in longer arterial conduits which can reach the lateral and posterior wall of the heart, such as in our case. Sometimes, RITA is too short for grafting coronary arteries in the posterior wall of the heart. Alternatively, when the LAD lesion is proximal, a transected short segment of distal LIMA could be anastomosed to the distal RITA to accomplish complete revascularization. We have used this technique in several patients with good results. A short segment of the radial artery or saphenous vein may be used as well as disclosed by a paper by Davierwala (2013).
We consider off-pump beating heart coronary artery surgery as the best choice in PA patients with hemodynamic stability meanwhile in patient without hemodynamic stability we prefer on-pump beating heart revascularization with a combination of peripheral arterial cannulation and central venous drainage for cardiopulmonary bypass.
References
1. Davierwala, P. M. (2013) “No-touch aorta off-pump coronary bypass operation: arteriovenous composite grafts may be used as a last resort,” Annals of Thoracic Surgery, 95 (3) 846-852.
Publisher – Google Scholar
2. Fiore, A. C, Naunheim, K. S, Dean, P.(1990) “Results of internal thoracic artery grafting over 15 years: single versus double grafts,” Annals of Thoracic Surgery, 49:202—209.
Publisher – Google Scholar
3. Hokenek, F, Gursoy, M, Ozgol, I, Gulcan, F. and Kınoglu, B. (2011) “A new proximal anastomosis technique in two patients with severely calcified aorta,” Annals of Thoracic Surgery, 92 (5)1914—1916.
Publisher – Google Scholar
4. Emmert, M. Y, Seifert, B, Wilhelm, M, Grünenfelder, J, Falk, V, Salzberg, S. P. (2012) “Aortic no-touch technique makes the difference in off-pump coronary artery bypass grafting,”Journal of Thoracic and Cardiovascular Surgery, 143 (4) 995.
5. Kumar, K, Deval, M, Manoria, P, Chand, P. and Jagdale, L. (2011) “Off pump CABG with aortic-no-touch using bilateral in-situ IMA: a new technique,” Indian Journal of Thoracic and Cardiovascular Surgery 27 (4)165—168.
Publisher – Google Scholar