Correctly reported systolic pressure in patients with complicated diabetes (130 mmHg) correlated with younger age of the physician (r=0.330, p=0.007). The correct diastolic pressure in patients with hypertension and complicated diabetes (80 mmHg) correlated with a given local instruction (r=0.295, p=0.020). Otherwise no correlation to demographic factors was seen.
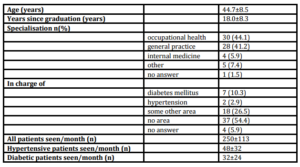
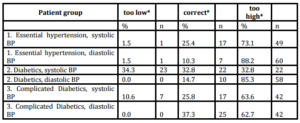
The mean ± SD blood pressure suggested by the physicians was 150.1±10.1 / 91.8±4.8 mmHg, median 150/90 in group 1 essential hypertension, 141.4±8.4 / 87±4.0 mmHg, median 140/85 in group 2 diabetic patients and 135.6±7.2 / 84.1±4.3 mmHg, median 135/85 in group 3 diabetes with complications.
Discussion
The self-reported awareness of the hypertension guidelines was good in Finnish general practice in the present study as also in the earlier Finnish studies by Alanen (2007,2008), at least reported by the physicians themselves. However, in spite of the apparent awareness nearly two thirds of the physicians reported higher trigger blood pressure values for intensifying the antihypertensive treatment compared to the guidelines (2005). Our study confirms the earlier results by Steinman et al (2004) and the Cypriot study (2012) that clinicians overestimate their adherence to hypertension guidelines. In the Cypriot study 95.6 % of the physicians declared to be aware of the hypertension guidelines. However, more than one-fourth of high risk hypertensive patients remained untreated and 60 % of low risk patients received inappropriate medication.
Although only roughly 70% of the physicians selected answered the questionnaire the response was quite satisfactory, compared for example to the 34% seen in the self BP monitoring study of Tyson et al (2003) using mailed questionnaires. Some physicians may have experienced the study as an interrogation of guideline knowledge and thus not answered the questionnaire. The number of general practitioners in Finland is 3500, altogether. Thus, our sample represented only about 2 % of them. However, considering the homogeneity of the Finnish population and physicians, we believe that reliable conclusions can de drawn despite the modest amount of physicians who completed the questionnaire. Previous studies by Alanen et al (2007, 2008) discussing the implementation of guidelines have almost solely been based on the opinions of the chief of the centre or the chief nurses and concerned the implementation in general. The benefit of this study was that the actual values of intensifying antihypertensive treatment were asked from the treating physicians themselves. The physicians were not controlled if they were using the literature for answering, but the results show that they probably did not check the trigger values when answering.
According to a recent Finnish study by Sipilä et al (2011), multifaceted implementation intervention has not lead to significant changes in antihypertensive drug prescribing performance. The results of our study were alike. Despite the self-reported knowledge of the guidelines, the reported trigger values for intensifying the antihypertensive treatment differed from those mentioned in the Finnish guidelines (2005) in over 60% of cases and were about 5-10/5 mmHg higher than those suggested in the guidelines. Particularly alarming were the high trigger values reported in the treatment of patients with uncomplicated essential hypertension. Probably reluctant treatment intensification partly explains the suboptimal treatment results seen in reaching BP targets in recent Finnish studies by Varis et al (2009) and Vartiainen et al (2010). Either the physicians had not read the guidelines thoroughly or they disagreed with them. We cannot find the proper answer from our study. Although the trigger values for essential hypertension followed by the physicians had been 140/90 mmHg for essential hypertension and 130/80 mmHg for diabetics as suggested by the European Society of Hypertension and the European Society of Cardiology (2003) at that time, the trigger values suggested by the physicians in this study were clearly higher.
In an Austrian study by Fürthauer et al (2013) hypertensive patients were quite well controlled, only 17.9 % of the patients were above the blood pressure target. The most important reason was the physician not providing an appropriate treatment due to the lack of awareness of the existence of the guidelines or lack of familiarity of the guideline. Small amount (2.9 %) was due to a deliberate decision to counteract the guideline. Dechend et al (2012) suggested according to their large Prospective 3A registry study that major efforts are required to improve hypertension management as recommended by the current guidelines, also shown in our much smaller study. Also in Ontario, Canada Dickson et al (2013) indicated according to their results that blood pressure measurement according to Canadian Hypertension Education Program was felt to be important, but there is still room for improvement in the conduction.
In a Chinese study among general practitioners by Chen et al (2013), the average accuracy rate of hypertension prevention knowledge was 49.2 %, ranging from 10.5 to 94.7 %. The factors associated to accuracy rate were the education level of the physician and type of centre. According to our study, young age of the physician and local guidelines were important to achieve the knowledge of the guidelines. Most Chinese physicians (87.8 %) reported being willing to attend training courses regularly. The preferred course was medical treatment of hypertension and the most favoured training approach expert lectures.
In an Austrian study (2013) during the eleven year follow-up in pediatric obesity care, screening for co-morbidity increased significantly in overweight and obese children and adolescents. Adherence of guidelines was still insufficient in some institutions. They suggested that quality control based on benchmarking would improve obesity care. In a randomized study in Veterans Affairs outpatient clinics by Petersen et al (2013), individual financial incentives, but not practice-level or combined incentives, lead to a greater blood pressure control or appropriate response to uncontrolled blood pressure. However, none of the incentives resulted in greater use of guideline-recommended medication or increased incidence in hypotension compared with controls.
In contrary, in our study in patients with hypertension and non complicated diabetes systolic BP trigger value was reported as an equal or even lower in one third of the physicians. However, one third of them reported too high values, as over 80 % reported too high diastolic blood pressure. It probably suggests that the guideline message had come through a little better concerning systolic pressure. This is perhaps due to the fact that low BP recommendations for diabetics have been expressed both in diabetic and hypertension guidelines. Of course, it is also possible that it only reflects higher concern of diabetic patients and had nothing to do with the published guidelines. The reported trigger values in patients with complicated diabetes were a little better but still over 60 % of the physicians reported too high values.
Results from the present study support the view that the implementation of hypertension guidelines needs intensifying, especially concerning the patients with uncomplicated essential hypertension. According to the study there has been some activity among physicians concerning local guideline education and community-sponsored conference visits but it seems that it has not succeeded effectively as the guidelines are not followed in everyday practice. Naturally, every patient is an individual and treatment should be tailored accordingly, taking into account patient based factors like for example ortostatism. However, the treatment target is similar in all patients. Despite, as this study suggests, the majority of physicians had chosen target values exceeding those suggested in the guidelines. Also in the study by Hagemeister et al (2001) the impact of hypertension guidelines on actual medical knowledge was modest. Adequate guideline awareness was found in 23.7 % of the total study population of 24 899 German physicians.
The hypertension guidelines in Finland are accessible by the patients in the Internet. If treating physician is satisfied with BP targets exceeding the guidelines, some patients may become astonished and their adherence to treatment decrease as discussed above. Besides reaching the treatment target the physicians also do not follow the suggestions concerning the choice of the medication and are partly resistant to use combination treatment adequately according to a study by Sipilä et al (2011). Beta-blockers are still the most used antihypertensive drugs in Finland as stated by Varis et al (2009).
Conclusion
This study suggests that clinicians overestimate their adherence to hypertension guidelines as seen also in one earlier study. The blood pressure trigger values to increase medication were higher than suggested in current care guidelines in over half of the physicians. In most former studies the clinicians had only been asked for the adherence, not trigger values.
References
1. Alanen, S.I, Johannala-Kemppainen, R, Ijäs, J, Kaila, M, Klockars, M, Mäkelä, M. and Välimäki, M. (2007)“Evaluation of Current Care Effectiveness: A survey of hypertension guideline implementation in Finnish health centres,”Scandinavian Journal of Primary Health Care, 25(4) 232-236.
Publisher – Google Scholar
2. Alanen, S, Ijas, J, Kaila, M, Makela, M. and Valimaki, M. (2008) “Hypertension guideline implementation: experiences of Finnish primary care nurses.” Journal of Evaluation in Clinical Practice, 14(5) 830-835.
Publisher – Google Scholar
3. Chen, Q, Zhang, X, Gu, J, Wang, T, Zhang, Y. and Zhu, S. (2013) “General practitioners’´ hypertension knowledge and training needs: a survey in Xuhui district, Shanghai.” BMC Family Practice, 14(16) 1-10.
Google Scholar
4. Dechend, R, Kaiser, E, Derer, W, Deeg, E, Busjahn, A, Schmieder R.E. and Zeymer,U. (2012) “Guideline adherence in cardiovascular risk assessment and analysis in 15,000 hypertensive German patients in real life: results of the Prospective 3A Registry.” Journal of Clinical Hypertension (Greenwich), 14(8) 496-501.
Publisher – Google Scholar
5. J F Birrell. Aural Tuberculosis in Children. Proc. roy. Soc. Med. Volume 66 April 1973 .
6. Dickson R.C, Gaebel, K, Zizzo, A, Neimanis, I, Bridge, M, Corsini, J, Goebel, C, Levy R. and Woods, A. (2013)“Self-reported physician adherence to guidelines for measuring blood pressure.” Journal of the American Board of Family Medicine, 26(2) 215-217.
Publisher – Google Scholar
7. Flechtner-Mors, M, Wiegand, S, Gellhaus, I, Siefken-Kaletka, H, Widhalm, K, Reinehr, T, Roost, H.P, Leipold, G, Hoffmeister, U. and Holl, R.W. (2013) “Screening for co-morbidity in 65,397 obese pediatric patients from Germany, Austria and Switzerland: adherence to guidelines improved from the year 2000 to 2010.” Obesity Facts, 6(4) 360-368.
Publisher – Google Scholar
8. Fürthauer, J, Flamm, M. and Sönnichsen, A. (2013) “Patient and physician related factors of adherence to evidence based guidelines in diabetes mellitus type 2; cardiovascular disease and prevention: a cross sectional study.” BMC Family Practice, 14 (47) 1-8.
Google Scholar
9. Guidelines Committee (2003). “2003 European Society of Hypertension—European Society of Cardiology guidelines for the management of arterial hypertension.” Journal of Hypertension, 21 (6) 1011—1053.
10. Hagemeister, J, Schneider, C.A, Barabas, S, Schadt, R, Wassmer, G, Mager, G, Pfaff, H. and Höpp, H.W. (2001)“Hypertension guidelines and their limitations — the impact of physicians´ compliance as evaluated by guideline awareness.” Journal of Hypertension, 19(11) 2079-2086.
Publisher – Google Scholar
11. Petersen, L.A, Simpson, K, Pietz, K, Urech, T.H, Hysong, S.J, Profit, J, Conrad, D.A, Dudley R.A. and Woodard, L.D. (2013) “Effects of individual physician-level and practice-level financial incentives on hypertension care: a randomized trial.” JAMA, 310(10) 1042-1050.
Publisher – Google Scholar
12. Sipilä, R, Helin-Salmivaara, A, Korhonen, M.J. and Ketola E. (2011) “Change in antihypertensive drug prescribing after guideline implementation: a controlled before and after study.” BMC Family Practice, 12(87) 1-12.
Google Scholar
13. Steinman, M.A, Fischer, M.A, Shlipak, M.G, Bosworth, H.B, Oddone, E.Z, Hoffman, B.B. and Goldstein, M.K. (2004) “Clinician awareness of adherence to hypertension guidelines.” American Journal of Medicine 117(10) 747-754.
Publisher – Google Scholar
14 Theodorou, M, Stafylas, P, Kourlaba, G, Kaitelidou, D, Maniadakis, N. and Papademetriou, V. (2012)
“Physicians´ perceptions and adherence to guidelines for the management of hypertension: A national multicentre, prospective study.” International Journal of Hypertension, 503821 1-11.
Publisher – Google Scholar
15. Tyson, M.J. and McElduff, P. (2003) “Self blood pressure monitoring — a questionnaire study: response, requirement, training, support-group popularity and recommendations.” Journal of Human Hypertension, 17(1) 51-61.
Publisher – Google Scholar
16. Varis, J, Savola, H, Vesalainen, R. and Kantola, I. (2009) “Treatment of hypertension in Finnish general practice seems unsatisfactory despite evidence based guidelines.” Blood Pressure 18(1-2) 62-67.
Publisher – Google Scholar
17. Vartiainen, E, Laatikainen, T, Peltonen, M, Juolevi, A, Männistö, S. and Sundvall J. (2010) “Thirty-five-year trends in cardiovascular risk factors in Finland.” International Journal of Epidemiology, 39 504-518
Publisher – Google Scholar
18. Working group set up by the Finnish Society of Hypertension. (2002) “Hypertension. Current Care guideline.” Duodecim, 118(1) 110-126.
19. Working group set up by the Finnish Society of Hypertension, Käypä hoito. (2005) “Hypertension Current Care guideline.” Duodecim, 122(3) 339-340 (www.kaypahoito.fi).