All subjects at pre-treatment stage of this study had orthognathic maxilla, retrognathic mandible, open configuration, proclination of upper and lower incisors and convex profile compared with Thai norms (Dechkunakorn et al., 1992). From patients’ interviews, approximately 50% of the subjects had taken off their retainers before the appropriate period. Retention period in males was 0.73 years, and in females 0.81 years (mean of both was 0.77 years). The possible reason may be attributed to unawareness of the importance of wearing retainers and the weakness of the follow-up system.
Twenty-nine patients had complete documents. The mean age of the subjects (13.84 years) was similar to the studies by Luppanapornlarp and Johnston, 1993, 12.88 years and Paquette et al., 1999, 12.53 years. Most orthodontic Class II patients were treated during the parapubertal growth spurt. The post-retention period in this study was 4.15 years, which was shorter compared with studies by Gardner and Chaconas, 1976 (5.3 years) and Harris et al., 1999 (5.5 years).
Skeletal Changes
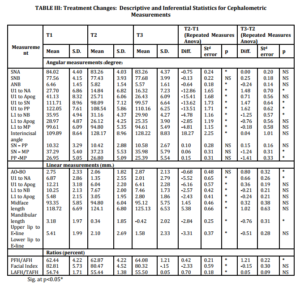
Most post-treatment changes (T2-T1, Table III) showed significant (p<0.05) differences in cephalometric variables, except SNB, SN-PP, SN-MP, PP-MP and Wits appraisal. SNB values were not significantly different from those reported by Harris et al.,1999 and Basciftci et al.,2003 . After treatment the antero-posterior position of maxilla relative to the cranial base decreased which may have occured as a result of the remodeling of A point or the anterior movement of N point. Therefore, the ANB correction was primarily due to the decrease of SNA (Merrifild and Cross,1970; Bennett et al.,1975).
In regard to the post-treatment changes in vertical direction, SN-PP, SN-MP and PP-MP did not change significantly. PFH/AFH, LAFH/TAFH increased significantly and UAFH/LAFH (Facial index) reduced significantly. This could have been because these patients showed the tendency to grow vertically quite equally in the anterior and posterior parts of the face during the treatment.
Mandibular length also showed significant (p<0.05) difference after treatment due to the growth of the mandible in late adolescence (Harris et al.,1999; Hellman,1927; Nanda, 1955) and the parapubertal growth spurt (Hellman,1927 ; Koen,1981).
After treatment, midface length increased significantly (p<0.05). Behrents, 1984 reported that the change of midface dimension might be attributed to an increase in the nasal airway from the increased physiologic demands brought on by age or due to the downward and forward growth of the maxilla during late adolescence.
In the post-retention period (T3-T2), no significant (p<0.05) changes were found in antero-posterior direction at SNA, SNB and ANB, which was similar to the studies by Luppanapornlarp and Johnston,1993 and Paquette et al.,1992 . These observations revealed a small amount of growth during the post-retention period. However, the Wits appraisal of this study increased significantly at post-retention which might be associated to relapse of the functional occlusal plane from orthodontic treatment.
Regarding the post-retention changes, the maxilla showed no difference in the PP plane (SN-PP changed with no significance), but the mandible showed a tendency to grow in an upward direction (SN-MP decreased significantly, PP-MP decreased significantly and PFH/AFH increased significantly). These results are similar to previous studies by Harris et al.,1999 and Erdinc et al.,2006 , which found that the increase in posterior facial height was more than that of the anterior facial height resulted in a decrease in the two angles of the occlusal planes (Downs’ and Functional) to the Frankfort Horizontal Plane. This growth pattern promotes upward and forward mandible rotation and stability of the class II correction from the end of treatment to post-retention period. Many studies have stated that the increase in the PFH/AFH ratio indicates a good prognosis for maintenance of the Class II correction because the consequence of an increasing ratio is an upward and forward (counterclockwise) rotation of the mandible and a flattening of the occlusal plane (Horn,1992; Subtelny et al.,1966; Bjork,1969; Isaacson et al.,1977; Woodside and Linder-Aronson,1979; Neilson,1991). Control of the vertical dimension during correction of a moderate to high angle Class II malocclusion could be the single most important factor influencing favorable mandibular change (Bjork,1969; Isaacson et al.,1977; Neilson,1991) . If vertical control is lost, the mandible can rotate downward and backward, decreasing the potential for a favorable mandibular change. Furthermore, Horn,1992 found that the PFH/AFH ratio is a good indicator of vertical control as active treatment progressed. He stated that an increase in the PFH/ AFH ratio indicates good control of the vertical dimension.
In summary of skeletal changes, the subjects were successfully treated and the increase in posterior facial height also promoted the stability of Class II correction. The increase of posterior facial height may be a good control in the posterior dentoalveolar height, which may result from the forward movement of the molars into the extraction site.
Dental Changes
The cephalometric analysis (Table III, T2-T1) showed that all variable related to upper and lower incisors significant decreased (p<0.05) after treatment, except increase in the interincisal angle. These changes were observed because of the retraction of the upper incisors and slight retroclination of lower incisors to correct the dental overjet and overbite during the treatment (Basciftci and Usumez,2003).
Post-retention changes (Table III, T3-T2) showed a tendency of relapse of the proclined position of the upper incisors; four variables of the upper incisors increased significantly (U1 to NA, U1 to SN, U1 to PP and linear measurement of U1 to NA). Although the angulation and inclination of lower incisors decreased in all measurements, only L1 to NB decreased significantly.
The incisal angulation relapsed because of the changes in the overjet from the relapsed upper incisors and the retroclination of the lower incisors. This result contrasts with the studies by Luppanapornlarp and Johnston,1993 and Paquette et al.,1992 , who found that upper and lower incisors continued to retrocline at the post-treatment period. The difference can be attributed to the more uprighted upper incisor position in this study. Overly uprighted or tipped incisors have a tendency to return to their original position. As a result, the clinician should pay attention to the adequacy of lingual root torque of incisors before removing the fixed appliance.
Soft Tissue Profile
At post-treatment period (Table III, T2-T1); upper and lower lip to E line significantly decreased to a more esthetic lip profile because of the changes in the upper and lower incisors. The profiles tend to have straighter faces in extraction cases which are similar to reports by Bishara et al.,1997 and Basciftci and Usumez ,2003 .
For the post-retention changes (T3-T2), upper and lower lip to E line showed improved esthetic profile which decreased further 0.76 and 0.51 mm, respectively, but significant difference was seen only in upper lip to E line. The result is consistent with those of Luppanapornlarp and Johnston,1993 . This flattening of the facial profile was evident of maturational changes associated with continued mandibular growth, upward and forward mandibular rotation and growth of the nose and chin (Schudy,1974; Anderson,1973;Zierhut et ai.,2000.
Overall, the results of this study supported previous findings that only minor relapse is found after Class II correction (Uhde et al.,1983; Hellekant et al.,1989). Although the incisors changed significantly, the other smaller changes in the relationships may not be clinically significant.
Conclusion
The present study aimed to determine the long-term dental, skeletal and soft tissue profile changes in 29 Class II Division 1 with skeletal type II orthodontic patients (14 males and 15 females) treated in combination with the removal of the four premolars and fixed appliance. The results can be summarized as follows: 1) most of the skeletal parameters showed no significant difference between post-treatment and post-retention, except decrease in SN-MP and PP-MP and increase in PFH/AFH ratio, which are the primary factors in the maintenance of the corrected Class II malocclusion; 2) upper incisors tended to procline but lower incisors tended to retrocline after post-retention; 3) upper and lower lip to E-line continued to decrease during post-retention, and 4) the correction of Class II by extracting four premolars showed relatively stable results.
References
[1] Suchato, W. and Chaiwat, J. (1981), ‘Prevalence of malocclusion in young adult,’ Mahidol Dent J, 2,133-143.
[2] Kingsley, NW. (1880), ‘Oral Deformities,’ New York. D Appleton and Company, 136.
[3] Shapiro, PA. (1974), ‘Mandibular dental arch form and dimension. Treatment and posttratment changes,’ Am J Orthod, 66, 58-70.
Publisher
[4] Dechkunakorn, S. Sawaengkit, P., Anuwongnukroh, N. Sonthilawat, P. (1975), ‘Correspondence of antero-posterior jaw relation indicators,’ J Dent Assoc Thai, 42, 62-68.
[5] Little, RM.( 1975), ‘The Irregularity Index: A quantitative score of mandibular anterior alignment,’ Am J Orthod , 68, 554-563.
Publisher – Google Scholar
[6] Gardner, SD. and Chaconas, SJ. (1976), ‘Posttreatment and postretention changes following orthodontic therapy,’ Angle Orthod, 46(2), 151-161.
[7] Luppanapornlarp, S.and Johnston, LE. (1993), ‘The effects of premolar-extraction: A long-term comparison of outcomes in “clear-cut” extraction and nonextraction Class II patients,’ Angle Orthod, 63, 257-272.
[8] Paquette, DE., Beattie, JR. and Johnston, LE. (1992), ‘A long-tern comparison of non-extraction and premolar extraction edgewise therapy in “borderline” Class II Patients,’ Am J Orthod, 102(1), 1-14.
[9] Harris, EH., Gardner, RZ. and Vaden, JL. (1999), ‘A longitudinal cephalometric study of postorthodontic craniofacial changes,’ Am J Orthod,115,77-82.
[10] Basciftci, FA. and Usumez, S. (2003), ‘Effects of extraction and nonextraction treatment on Class I and Class II subjects,’ Angle Orthodontist, 73,36-42.
[11] Merrifield, LL. and Cross,J. (1970), ‘Directional forces,’ Am J Orthod, 57, 435-464.
Publisher
[12] Bennett, TH., Tullock, TFC., Vig, KWL. and Webb, WG. (1975), ‘Overjet stability after treatmentof Class II division1 malocclusion,’ Br J Orthod ,2,239-246.
[13] Hellman, M. (1927), ‘Changes in the human face brought on bydevelopment,’ Int J Orthod,13,475-516.
[14] Nanda, R. (1955), ‘The rats of growth of several facial components measured from serial cephalometric roentgenograms,’ Am J Orthod,41,658-673.
Publisher
[15] Koen, MC. (1989)Use of skeletal maturity indicators to enhance growth prediction during adolescence (Master’s Thesis) Memphis: University of Tennessee.
[16] Behrents, RG. (1984) A treatise on the continuum of growth in the aging craniofacial skeleton (PhD Dissertation). Ann Arbor: University of Michigan.
[17] Erdinc, A.E., Nanda, RS.and Isiksal, E. (2006), ‘Relapse of anterior crowding in patients treated with extraction and nonextraction of premolars,’ AJODO, 129,776-784.
[18] Horn, A. (1992), ‘Facial height index,’ Am J Orthod,102:180-186.
[19] Subtelny, Ill. and Sakuda, M. (1966), ‘Muscle, oral malformation, and growth changes,’ Am J Orthod, 52,495-517.
Publisher
[20] Bjork, A. (1969), ‘Prediction of mandibular growth rotation,’ Am J Orthod, 55, 585-599.
Publisher – Google Scholar
[21] Isaacson, RJ. Zapfel, RJ., Worms, FW. and Erdman, AG. (1977), ‘Effects of rotational jaw growth on the occlusion and profile,’ Am J Orthod, 72, 276-286.
Publisher
[22] Woodside, DG. and Linder-Aronson, S. (1979), ‘The channelization of upper and lower anterior face heights compared to population standards in males between ages 6-20 years,’ EurJ Orthod, 1, 214-240.
Publisher – Google Scholar
[23] Nielson, IL. (1991), ‘Vertical malocclusions: etiology, development, diagnosis and some aspects of treatment,’ Angle Orthod, 61, 247-260.
[24] Bishara, SE., Cummins, DM. and Zaher, AR. (1997), ‘Treatment and posttreatment changes in patients with ClassII, Division 1 malocclusion after extraction and nonextraction treatment,’ AJODO, 111,18-27.
[25] Schudy, FF. (1974), ‘Posttreatment craniofacial growth: its implications in orthodontic treatment,’ Am J Orthod, 65:,39-57.
Publisher – Google Scholar
[26] Anderson, JP., Joondeph, DR. and Turpin, DL. (1973), ‘A cephalometric study of profile changes in orthodontically treated cases ten years out of retention,’ Angle Orthod, 43, 324-336.
[27] Zierhut, EC., Joondeph, DR., Artun, J. and Little, RM. (2000), ‘Long-term profile changes associated with successfully treated extraction and nonextraction Class II Division 1 malocclusions,’ Angle Orthod,70,208-19.
[28] Uhde, MD., Sadowsky, C. and BeGole. EA. (1983), ‘Long-tenn stability of dental relationships after orthodontic treatment,’ Angle Orthod,53, 240-252.
[29] Hellekant, M., Lagerstrom, L. and Gleerup, A. (1989), ‘Overbite and overjet correction in a Class II Division 1 sample treated with edgewise therapy,’ Eur J Orthod,11,91-106