Anantharam, B., Chahal, N., Stephens, N. & Senior, R. (2010). “Temporo-mandibular Joint Dislocation: An Unusual Complication of Transoesophageal Echocardiography,” European Journal of Echocardiography, 11 (2), 190-1.
Publisher – Google Scholar
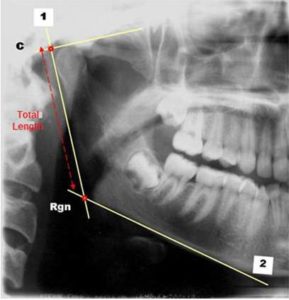
Bezuur, J. N., Habets, L. L. M. H. & Hansson, T. L. (1988). “The Recognition of Craniomandibular Disorders- A Comparison between Clinical, Tomographical, and Dental Panoramic Radiographical Findings in Thirty- One Subjects,”Journal of Oral Rehabilitation, 15 (6), 549-54.
Publisher – Google Scholar
Bezuur, J. N., Habets, L. L. M. H. & Hansson, T. L. (1989). “The Recognition of Craniomandibular Disorders; Condylar Symmetry in Relation to Myogenous and Arthrogenous Origin or Pain,” Journal of Oral Rehabilitation, 16 (3), 257-60.
Publisher – Google Scholar
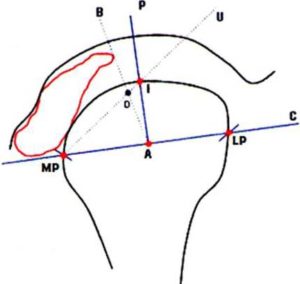
Giambartolomei, L. A. (2003). “Anatomía del Complejo Articular Cráneomandibular — ATM,” Ed: Publicaciones Universidad Nacional de Córdoba; ISBN: 950 — 33 — 0410 — 5.
Publisher
Habets, L. L. M. H., Bezuur, J. N., Naeiji, M. & Hansson, T. L. (1988). “The Orthopantomogram, an Aid in Diagnosis of Temporomandibular Joint Problems. ll. The Vertical Symmetry,” Journal of Oral Rehabilitation, 15 (5), 465-71.
Publisher – Google Scholar
Hutchinson, S. Y. (2005). “Cone Beam Computed Tomography Panoramic Images vs. Traditional Panoramic Radiographs,” American Journal of Orthodontics & Dentofacial Orthopedics, 128 (4), 550-550.
Publisher – Google Scholar
Isberg, A. (2003). ‘Disfunción de la Articulación Temporomandibular,’ Ed. Artes Médicas Latinoamérica, 91, 173 – 180.
Google Scholar
Kopp, S. & Rockler, B. (1979). “Relationship between Clinical and Radiographic Findings in Patients with Mandibular Pain or Dysfunction,” Acta Radiologica: Diagnosis, 20, 456.
Publisher – Google Scholar
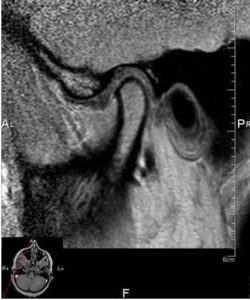
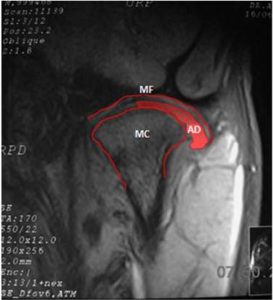
Larheim, T. A. (2005). “Role of Magnetic Resonance Imaging in the Clinical Diagnosis of the Temporomandibular Joint,”Cells Tissues Organs 180 (1), 6-21.
Publisher – Google Scholar
López López, J., Chimenos Küstner, E., Blanco Carrión, A., Reselló Llabrés, X. & Jané Salas, E. (2005). “Diagnóstico Por la Imagen de los Trastornos de la Articulación Craneomandibular,” Avances en Odontoestomatología, 21 (2), 71-88.
Publisher – Google Scholar
Okeson, J. P. (1999). ‘Anatomía Funcional y Biomecánica del Sistema Masticatorio. En: Tratamiento de Oclusión y Afecciones Temporomandibulares,’ Ed. Mosby, 7-17.
Paesani, D., Westesson, P.- L., Hatala, M. P., Tallents, R. H. & Broods, S. L. (1992). “Accuracy of Clinical Diagnosis for TMJ Internal Derangement and Arthrosis,” Oral Surgery, Oral Medicine, Oral Pathology, 73 (3), 360-3.
Publisher – Google Scholar
Panmekiate, S., Petersson. A., Rohlin, M., Akerman, S. & Isberg, P.- E. (1995). “Corrected Sagittal Tomography of the Temporomandibular Joint. Influence of Errors in Film and Patient Positioning on Linear and Angular Measurements,” Acta Odontologica Scandinavica 53 (4), 264-9.
Publisher – Google Scholar
Park, J. W., Song, H. H., Roh, H. S., Kim, Y. K. & Lee, J. Y. (2012). “Correlation between Clinical Diagnosis Based on RDC/TMD and MRI Findings of TMJ Internal Derangement,” International Journal of Oral & Maxillofacial Surgery 41(1), 103-8.
Publisher – Google Scholar
Pasquet, G. & Cavezian, R. (2009). “Diagnostic Means Using oral and Maxillofacial Cone Beam Computed Tomography: Results,” Journal de Radiologie 90 (5 Pt 2), 618-23.
Publisher – Google Scholar
Reyez Tellez Girón, J. & Nuñez Tovar, C. (1998). ‘Nomenclatura Anatómica Internacional,’ Ed. Médica Panamericana, 19, 59, 44-45.
Google Scholar
Rezende Barbosa, G. L., Nascimento, M. D. C. C. & Ladeira, D. B. S., Bomtorim, V. V., da Cruz, A. D. & Almeida, S. M. (2013). “Accuracy of Digital Panoramic Radiography in the Diagnosis of Temporal Bone Pneumatization: A Study in Vivo Using Cone-Beam-Computed Tomography,” Journal of Cranio-Maxillofacial Surgery. Jul 11. pii: S1010-5182(13)00178-9.
Publisher – Google Scholar
Winocur, E., Reiter, S., Krichmer, M. & Kaffe, I. (2010). “Classifying Degenerative Joint Disease by the RDC/TMD and by Panoramic Imaging: A Retrospective Analysis,” Journal of Oral Rehabilitation, 37(3):171-7.
Publisher – Google Scholar