Introduction
Distraction Osteogenesis (DO) involves gradual, controlled displacement of surgically created fractures (subperiosteal osteotomy) by incremental traction (Ilizarov, 1988), resulting in simultaneous expansion of soft tissue and bone volume due to mechanical stretching through the osteotomy site (Ilizarov, 1989). This ability to reconstruct combined deficiencies in bone and soft tissue makes the process unique and invaluable to all types of reconstructive surgeons. The procedure is now widely used by maxillofacial surgeons for the correction of craniofacial deformities. Initially external devices were used for distraction. Lately devices for intraoral usage are being engineered thereby increasing its potential applications in dentistry. The essence of orthodontic treatment is the movement of teeth through alveolar bone to obtain an esthetically ideal occlusion. Many advances have occurred in orthodontics over the past century, but relatively little has been done to enhance the rate at which tooth movement occurs and for successful management of complications such as ankylosed teeth. The current applications of DO in orthodontics focuses on addressing these concerns.
History of the Procedure
The history of DO begins with the old techniques of repositioning and stabilization of bone fractures used by Hippocrates, as noted in the book by Samchukov, Cherkashin, and Cope (1999). In early 20th century Alessandro Codivilla (1905) introduced a crude method of DO for lengthening of the lower limbs. Later, Abbott (1927) improved the Codivilla method by incorporating pins instead of casts; and Rosenthal (1930) first performed this technique in the maxillofacial region; who was followed by Kazanjian (1941) and Crawford (1948). Subsequently, Allan (1948) incorporated a screw device to control the rate of distraction. However, DO did not gain immediate acceptance until the breakthrough in 1951 when Gavril Ilizarov (1969), developed a technique for repairing complex fractures or nonunion of the long bones. Ilizarov’s procedure was based on the biology of bone and the ability of the surrounding soft-tissues to regenerate under tension. He was able to reduce the frequency and severity of the complications and made the surgery safer. Over the ensuing years, the technique was perfected, stimulating interest in DO.
The first reports of craniofacial DO maybe attributed to the rapid expansion of the palate that was carried out in growing patients in the 1960s (Haas, 1961). This practice, however, involved the distraction of a naturally occurring physis since it incorporates controlled soft-tissue and hard tissue expansion through a suture. Finally, Snyder et al. (1973) first described the Ilizarov technique to lengthen a surgical osteotomy of the canine mandible by 15mm. By the early 1990s, experimental investigation intensified following reports from New York University (Karp, Thorne, McCarthy & Sissons, 1990) and from Constantino et al. (1993), where DO was successfully used to augment and to close canine segmental lower jaw defects.
The first clinical results of craniofacial DO were reported by McCarthy et al. (1992) in patients with congenital deformities who successfully underwent gradual distraction of the mandible. Subsequently Polley and Figueroa (1997) made use of the procedure in the treatment of severe maxillary deficiency in children and adolescents with cleft problems. Presently craniofacial DO is implemented in the lower face (mandible), mid face (maxilla, orbits), upper face (fronto-orbital, cranial vault), and in congenital and acquired anomalies. Craniofacial anomalies account for most applications of distraction.
Evolution in Orthodontics
Modern research and development in the field of DO has led to the implementation of numerous innovative and revolutionary distraction systems. A wide variety of intraoral internal distractors now available are engineered to be small and compact with increased patient comfort and acceptance. This paved way to further investigating the technique for applications in influencing the rate and vector of tooth movement.
Liou and Huang (1998) first applied this concept to orthodontic tooth movement and performed rapid canine retraction through distraction, which they aptly termed as ‘Dental Distraction’. Later investigations validated that this rapid movement is a form of DO of the periodontal ligament which acts a ‘suture’ between alveolar bone and tooth with similar osteogenic potential (Liou, Figueroa & Polley, 2000). In a more recent study, Sayin et al. (2004) investigated the clinical validation of this technique and substantiated that this procedure reduced the net orthodontic treatment time. Soon after this concept was introduced, İşeri et al. (2001) and Kişnişci et al. (2002) used a different technique called ‘Dentoalveolar Distraction’ (DAD) for rapid canine distalization by performing osteotomies around the canines and achieved accelerated movement. This surgical technique does not rely on the stretching and widening of the periodontal ligament, thus prevents overloading and stress accumulation in the periodontal tissues (Gürgan, İşeri, & Kişnişçi, 2005). The technique was later substantiated with follow-up (Kurt, İşeri, & Kişnişci, 2010) and a large number of cases have since been treated successfully (Kişnişçi & Iseri, 2011).
In the same year Isaacson et al. (2001) successfully attempted to move an ankylosed central incisor using orthodontics, surgery and DO. Later, Kodof et al. (2005) demonstrated the effectiveness of treating ankylosed tooth and the surrounding alveolar ridge defect by a simple DO apparatus. More recent case reports have emphasized the evolutionary role of DO in attaining orthodontic correction of ankylosed anterior teeth (Dolanmaz, Karaman, Pampu & Topkara, 2010; Kim, Park, Son, Kim, Kim & Mah, 2010).
Distraction Device Classification
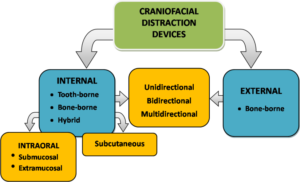
Distraction devices used for craniofacial osteodistraction are classified into two basic types: external and internal devices (Figure 1). Depending on the direction of action, they are further categorized as unidirectional, bidirectional, or multidirectional devices (Andrade, Gandhewar & Kalra, 2011). External devices are attached to the bone with percutaneous pins and fixation clamps, connected by a distraction rod. The internal devices can be placed subcutaneously, or placed intraorally as extramucosal or submucosal. Devices can be attached to the bone (bone-borne); to the teeth (tooth borne) or attached to both (hybrid type).
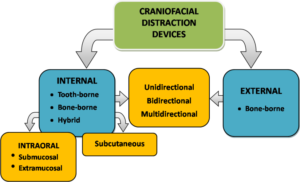
Figure 1: Classification of Craniofacial Distraction Devices
Influencing Rate of Tooth Movement
To date, several innovative modalities have been reported to accelerate orthodontic tooth movement, including low-level laser therapy, pulsed electromagnetic fields, electrical currents, corticotomy, distraction osteogenesis, and mechanical vibration. Recently Long et al. (2013) conducted a critical systematic review of randomized controlled trials to assess the effectiveness of these interventions where in they concluded that both corticotomy and distraction were effective and safe to accelerate orthodontic tooth movement. Kharkhar et al. (2010) in their quasi-randomized controlled trial to evaluate the best approach to reduce the overall orthodontic treatment time by means of distraction osteogenesis inferred that dentoalveolar distraction was superior to periodontal distraction in all areas of assessment. The details of major studies related to applications of distraction in rapid tooth movement and their methodological variations are presented in Table 1.
Table 1: Studiesa Related to Rapid Orthodontic Tooth Movement with Distraction Osteogenesis in Human Subjects

Both Dental Distraction and Dentoalveolar Distraction involve precision surgical procedure which is best suited to be done under nasotracheal general anaesthesia. But surgery can as well be performed on an outpatient basis, with the patient under local anaesthesia, sometimes supplemented with sedation. Since the procedures are invasive an antibiotic and non steroidal anti-inflammatory regimen is advised post surgically, along with strict oral hygiene maintenance instructions.
Methodology: Periodontal Ligament (Dental) Distraction
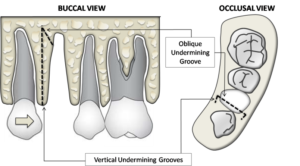
The anatomic position of the roots and the sites of interdental and horizontal osteotomies are assessed radiographically. After first premolar extraction, vertical osteotomies (undermining grooves) are carried out at the buccal and lingual sites of the interseptal bone adjacent to the canine tooth (Figure 2). The vertical osteotomies are now connected with an oblique osteotomy extending toward the base of the interseptal bone to weaken the resistance. The interseptal bone is not cut through mesiodistally toward the canine (Sayin, Bengi, Gürton & Ortakoğlu, 2004). The depth of the osteotomy is dependent on the thickness of the interseptal bone, as revealed radiographically. The distractors are cemented in place after the surgery.
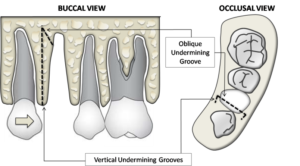
Figure 2: Surgical Technique Involving Vertical and Oblique Undermining Grooves (Osteotomies) to Eliminate Interseptal Bone Resistance Distal to Canine. No Cuts are Performed on Buccal and Lingual Plates
Methodology: Dentoalveolar Distraction (DAD)
This more commonly used surgical procedure involves peripheral osteotomies in relation to the canine tooth and can be done precisely with the aid of CT scan (Figure 3). Periapical and panoramic radiographs supplemented with CT scan imaging are taken at the start and end of the distraction and consolidation. The osteotomy sites, root structures, individual length of the canine teeth, proximity of the maxillary sinus and the mental foramen can be accurately determined.

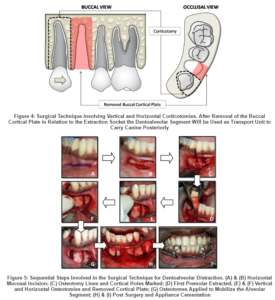
The surgical procedure is as described previously by Kişnişci et al. (2002). A horizontal mucosal incision is made parallel to the gingival margin of the canine and premolar beyond the depth of the vestibule and the surgical area is well exposed. The first premolar is extracted and a vertical osteotomy is made on the anterior aspect of the canine tooth by connecting multiple cortical holes made on the alveolar bone. The osteotomy was continued, passing 3 to 5 mm above the canine apex. A similar osteotomy was made along the posterior aspect between the first premolar buccal root and canine. Fine osteotomes are introduced and advanced in the coronal direction. The first premolar buccal cortical bone is removed, and any bony interference smoothed between the canine and the second premolar, preserving palatal or lingual cortical shelves. Larger osteotomes are used to fully mobilize the alveolar segment that includes the canine by fracturing the surrounding spongious bone around its root and off an intact lingual or palatal cortex and neighbouring teeth (Figures 4 & 5). In maxilla the apical bone near the sinus wall is removed, leaving the sinus membrane intact to avoid interferences during the distraction process. Finally, the ‘transport dentoalveolar segment’ includes the buccal cortex and underlying spongy bone that envelopes the canine root (Iseri, Kisnisci, Bzizi & Tuz, 2005). The distractor is now tried onto the canine and the first molar. To ensure that the transport segment is fully mobilized, the device is activated by several millimetres and set back to its original position. The incision is closed with sutures. Surgical procedure lasts approximately 30 minutes for each canine.
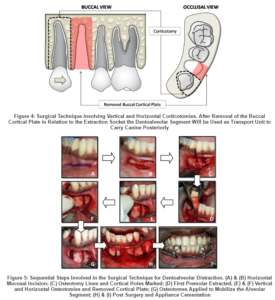
Appliance Construction
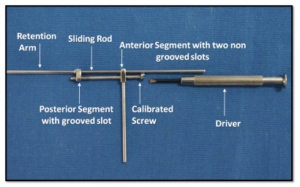
Majority of the individual canine distractors currently used are custom made, intraoral, tooth-borne device (Table 1). The distraction device (Figure 6) is fabricated from stainless steel and typically consists of:
- An anterior segment: adapted onto the canine.
- A posterior segment: includes a retention arm adapted onto the molar, and a grooved screw slot.
- A screw: of standardized diameter and a pitch.
- Sliding rod: acts as a guidance bar through which the anterior segment slides, and
- Screw wrench or driver: to advance the screw.
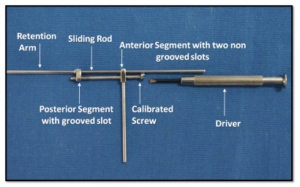
Figure 6: Custom Made Distractor Device
After the bands are fabricated and adapted for the canines and first molar, an impression is taken with irreversible hydrocolloid; the bands are transferred onto the impression and working models are made. The length of the screw can be arranged according to the distance between the distal point of the canine and the mesial point of the first molar. The distractor is then soldered to the bands with consideration of the biomechanical principles of tooth movement and the centre of rotation of the canine (Figure 7).

Figure 7: Canine Distraction Appliances
Distraction Protocol
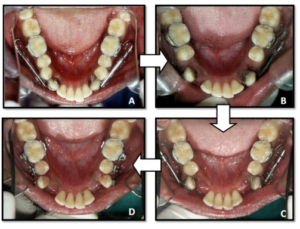
The distractor is activated twice per day, each consisting of one complete turn of 3600, for a total amount of about 0.8 mm per day. The distraction consists of gradual movement of the vascularized bony segment containing the canine tooth or ‘transport disc’. It takes less than 2 weeks for the canine to come into contact with the second premolar (Figure 8). The distractor is then removed and fixed orthodontic appliance treatment is immediately initiated concurrent to consolidation. Ligatures are placed under the archwire between the canine and the first molar and are kept at least 3 months for consolidation (Iseri, Kişnişci, Bzizi & Tuz, 2005; Kurt, İşeri & Kişnişci, 2010).
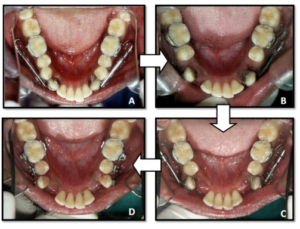
Figure 8: (A) Pre Distraction; (B) during Distraction Phase (6days); (C) & (D) Post Distraction (14 Days)
Treatment Progress
After the DAD is completed, the leveling and aligning phase is immediately initiated by round nickel-titanium arch wires in the upper and lower dental arches, followed by en masse anterior retraction. By the third month of orthodontic treatment, retraction of the anterior teeth is almost completed and the overjet reduced. Later, rectangular stainless steel arch wires are applied to maintain adequate torque in the anterior teeth. Overall active orthodontic treatment time in a bimaxillary dental protrusion case is as less as 6 months (Kurt, İşeri & Kişnişci, 2010).
Management of Ankylosed Tooth
Tooth ankylosis is the fusion of mineralized root surface to the surrounding alveolar bone with obliteration of the periodontal ligament (Biederman, 1956 & 1962). This is a common complication associated with trauma to maxillary incisors. According to the American Association of Orthodontics guideline (Excerpts from AAO Clinical Practice Guidelines for Orthodontics and Dentofacial Orthopedics, 1996), the treatment modalities for ankylosed teeth are: extraction, surgical luxation, surgical repositioning, fixed or removable appliances, and retention with or without coronal modifications. In the past, an ankylosed permanent anterior tooth was often surgically removed resulting in a significant vertical alveolar defect and a compromised aesthetic outcome. The surgical luxation concept though valid, is followed by a repair process that usually results in a recurrence of the ankylosis. Extraction and reimplantation occasionally results in external root resorption. Another surgical approach that has been reported involves corticotomies, where only the cortex of the bone is cut and orthodontic appliances are used to move the tooth over a period of a few weeks following the surgery (Phelan, Moss, Powell & Womble, 1990; Cheng, Zen & Su, 1997). This approach is very similar to, and could be considered the harbinger of, the DO procedure. When ankylosed, the gingival margin remains unaesthetically infrapositioned relative to neighbouring teeth. In the management of an ankylosed tooth with DO simultaneous expansion of soft tissues and alveolar bone is achieved without compromising blood supply to the tooth and the supporting bone resulting in an aesthetic outcome. The details of major studies related to applications of distraction in the management of ankylosis and their methodological variations are presented in Table 2.
Table 2: Studiesa Related to Orthodontic Tooth Movement of Ankylosed Teeth with Distraction Osteogenesis in Human Subjects

Methodology
The concept is based on alveolar bone distraction osteogenesis, used to augment the alveolar bone both vertically and horizontally (Smatt, Gibeili, Rahmi, Robin, Vanzo & Smatt, 1999; Urbani, Consolo, Lombardo & Bernini, 1999). The procedure can be carried out under local anaesthesia. A mucoperiosteal flap is reflected, and the bone exposed around the malpositioned tooth. Based on radiographic assessment, occlusally diverging vertical cuts are made from the mesial and distal interdental sides (interdental osteotomy) (Kofod, Würtz & Melsen, 2005; Alcan, 2006). Then, the two vertical cuts are combined by a third cut (subapical osteotomy), which is done horizontally two mm above the root apex (Figure 9). It is critical that the vertical osteotomies should be parallel or diverge occlusally. The alveolar segment is mobilized with the help of an osteotome taking care not to harm the palatal mucosa. The mucoperiosteal flap is then closed and sutured without repositioning the mobilized segment. A key aspect of the surgical procedure is to conserve as much attached gingiva as possible during the incision and suturing (Kim, Park, Son, Kim, Kim & Mah, 2010).
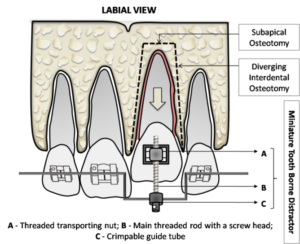
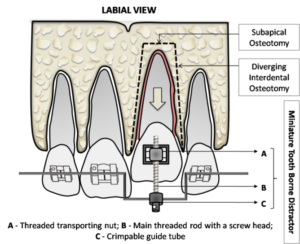
Figure 9: Surgical Technique Involving a Miniature Tooth Borne Distractor for Movement of Ankylosed Tooth
Appliance and Distraction Protocol
Custom made intraoral tooth borne distractors can be fabricated from conventional expansion screws (Kofod, Würtz & Melsen, 2005; Kim, Park, Son, Kim, Kim & Mah, 2010). Toros Alcan (2006) reported the effective use of a miniature tooth borne distractor in osteodistraction treatment of infrapositioned ankylosed teeth. This appliance is highly advantageous from the aspects of application, activation, buccolingual control, patient tolerance, and easy removal. The distraction device is composed mainly of three parts; threaded transporting nut designed to harness onto the bracket, main threaded rod with a screw head, and crimpable guide tube (Figure 9). The main threaded rod is at least 15 mm in length and 1.5 mm in diameter, performing a 0.25 mm distraction per turn.
The distractor is applied to the mobile tooth-bone segment using the archwire as the anchorage unit. Alveolar distraction typically carried out at a rate of 0.5 to 0.8 mm per day (Grayson & Santiago, 1999) would be appropriate for an ankylosed tooth. When the tooth reaches the level of its neighbour, activation is stopped; the distractor is removed and the tooth is included in the archwire for consolidation. If needed, tooth inclinations can also be corrected by applying torque and offset bends in the archwire, which changes the inclination of the distractor. Bone formation after distraction can be evaluated by both panoramic and periapical radiographs (Kinzinger, Jänicke, Riediger & Diedrich, 2003).
Bone Regenerate Evaluation
Panjabi et al. (1985 & 1989) and Fischgrund et al. (1994) found that the correlation between plain film radiographic density and biomechanical properties of the newly formed bone is poor. Frequent superimposition of adjacent bony structures in the maxillofacial region is a further compromise. Tjernstrom et al. (1992) showed that axial CT scans demonstrated great variations in regenerate bone appearance even though similar distraction protocols were used.Clinical evaluation of regenerate bone by manually stressing and checking for bone segment mobility is limited as well. Therefore evaluation using Quantitative Computed Tomography (QCT), described previously by Roth et al. (1997) and Smith et al.(1999) would be characteristic of the final level of regenerate healing. With QCT the hounsfield units measurement can be used to indicate the qualitative and quantitative analysis of bone volume (Shapurian, Damoulis, Reiser, Griffin & Rand, 2006) using subjective specification for cortical thickness and alveolar bone density before and after distraction.
Discussion
The regular rate of osteogenesis in orthodontic tooth movement during canine retraction is about 1 mm per month (Reitan, 1960 & 1967). Therefore with conventional orthodontic treatment techniques the canine retraction phase usually lasts 6 to 8 months. Both Vig et al. (1990) and Mavreas et al. (2008) reviewed the factors affecting the duration of orthodontic treatment, indicating that extraction treatments take longer than the non-extraction cases, the duration increasing with the number of extracted teeth. Therefore, under normal circumstances, conventional treatment with fixed appliances is likely to last 20 to 24 months.
Past notable attempts to shorten orthodontic treatment time included Corticotomy Assisted Orthodontics (CAO) (Gantes, Rathbun & Anholm, 1990; Chung, Oh & Ko, 2001; Wilcko, Wilcko, Bouquot & Ferguson, 2001; Long, Pyakurel, Wang, Liao, Zhou & Lai, 2013) which is based on the principle of Regional Acceleratory Phenomenon, a term first coined by Frost (1981). Physiologically, this theory proposes that when the bone is decorticated, an exuberant bone remodelling phase occurs in which teeth can be rapidly moved through demineralized bone due to an enhancement in cell-mediated tooth movement. The surgical procedure in CAO is extensive which includes palatal and vestibular mucosal incisions and corticotomies (Gantes, Rathbun & Anholm, 1990; Chung, Oh & Ko, 2001). In DAD, mucosal incisions and osteotomies are made only on the vestibular side of the alveolar bone, and the gingival margin, palatal mucosa, and palatal bone remain untouched, thus maintaining adequate blood supply for the transport dentoalveolar segment. Because it relies on the principles of DO, DAD might be expected to hold greater potential for generating bone than periodontal distraction.
The biomechanical factors thought to affect the quality of the distraction regenerate include the latency, rate, rhythm, and consolidation period (Swennen, Schliephake, Dempf, Schierle & Malevez, 2001). Most craniofacial surgeons have empirically applied the conclusions from long bone studies and recommend waiting periods of 4 to 7 days following osteotomy, allowing the formation and organization of a hematoma. Waiting too long before distraction (beyond 10 to 14 days) substantially increases the risk of premature bone union. However, the use of a zero latency period has found to have no adverse effects on the outcome while substantially shortening the treatment procedure (Chin & Toth, 1997; Toth, Kim, Chin & Cedars, 1998). In regard to the rate and rhythm of distraction, if the widening of the osteotomy site occurs too rapidly (>2 mm per day), then a fibrous non-union will result, whereas if the rate is too slow (<0.5 mm per day), premature bony union prevents movement (Aronson, 1994; Hegab & Shuman, 2012). These findings in long bones have been practically applied to the craniofacial skeleton, and most studies have described a rate of up to 1.0 mm, when activated twice per day (Spencer, Campbell, Dechow, Ellis & Buschang, 2011). The general rule holds that the consolidation period should be at least twice the duration of the distraction phase (Ilizarov, 1988). In DAD a consolidation phase of up to 3 months is recommended as in craniofacial distraction.
Long term follow up in DAD indicates that molar teeth did not show significant vertical, sagittal, and angular changes, signifying the absence of anchorage loss.24 This can be attributed to the rapid tooth movement and lack of time required for the hyalinized tissue on the compression side to be undermined with indirect resorption. No clinical and radiographic evidence of root fracture, root resorption, ankylosis, soft tissue dehiscence, or loss of vitality was observed in canine teeth at the end of DAD and orthodontic treatment, as well at follo w-up. Although the distractor is designed to be placed as high as possible on the buccal aspect of the canine tooth, moderate tipping is to be expected which can be readily overcome. This can be attributed to the application of force occlusal to the centre of resistance of the canine tooth caused by anatomic limitations of the vestibular sulcus (Kurt, İşeri & Kişnişci, 2010).
In treating ankylosed teeth it is noteworthy that DO treats the lack of growth of the alveolar process caused by the ankylosis and not the ankylosis itself. Therefore, treatment regimens must be planned relative to the patient’s remaining growth potential to avoid reoccurrence of the vertical deficiency (Kofod, Würtz & Melsen, 2005). If a patient’s vertical growth has ceased, the risk of relapse is minimal, but a patient with remaining growth potential can be either overcorrected or often subjected to the procedure. When compared to other treatment modalities for management of an ankylosed tooth, the versatility of DO lies in carrying the clinical crown, incisal edge and gingival margin to their appropriate position.
The Future
Advancements in the applications of craniofacial DO in orthodontics lies in persistent clinical research. This has set the foundation for molecular analyses of gene expression during DO, which has already led to the application of novel recombinant proteins and gene modified distraction protocols as demonstrated in the studies by Raschke et al. (1999), Long et al. (2011) and Castro-Govea et al. (2012). However, many issues still remain unresolved in regard to understanding how cells perceive the tension-stress effect of force, interpret it, and transmit intracellular messages. Analyzing the molecular events leading to successful DO has important clinical implications, since this is a fundamental step toward the evolution of targeted therapeutic interventions designed to accelerate osseous regeneration during distraction. Current research that is focused on the development of minimally invasive approaches; stem cells; biodegradable multiplanar distraction devices (Cohen & Holmes, 2001; Yamauchi, Mitsugi & Takahashi, 2007; Zakaria, Kon & Kasugai, 2012), should aim at decreasing the distraction and consolidation times, reducing complications, and optimizing patient outcomes.
DO is now entering a new era of the three-dimensional computer mediated preoperative planning and outcome assessment. The last few years have seen exciting advances in computer-assisted surgery (Gateno, Teichgraeber & Aguilar, 2000; Meehan, Morris, Maurer, Antony, Barbagli, Salisbury & Girod, 2006; Kanno, Mitsugi, Sukegawa, Hosoe & Furuki, 2008; Markiewicz & Bell, 2011). Computer-based three-dimensional scans will reconstruct the craniofacial skeleton and enable surgeons to virtually design, plan, and execute osteotomies. Cone beam CT scanners, which provide an excellent bony resolution at a fraction of the radiation, are now available for intraoperative CT imaging, bone regenerate evaluation, and postoperative follow-up. Ultimately, the application of virtual distractors together with fundamental biomolecular data will help guide the operator and patient expectations.
Conclusion
The human body possesses an enormous regenerative capacity. DO takes advantage of this potential to induce the regeneration of bone, nerve, blood vessels, and mucosa surrounding the tooth. The current applications of DO in orthodontics makes it a promising technique since it helps to overcome many of the present limitations, including reducing treatment duration not compromising the anchorage, and in the management of complexities; without any unfavourable long-term effects on periodontal tissues and surrounding structures. Older adolescents and adults are good candidates for distraction, whilst bimaxillary dental protrusion and Class II patients with severe overjet best perceive accelerated orthodontics with DAD.
It is very important to consider surgical and dental concerns during treatment planning. These concerns include, osteotomy design and location, selection of the distraction device, distraction vector orientation, duration of the latency period, the rate and rhythm of distraction, duration of the consolidation period, post-distraction orthodontics and functional loading of the regenerate bone. With technologic advancements, distraction devices have become smaller and more sophisticated than previous versions. Future may witness the use of the concepts of distraction to achieve better, faster & more efficient tooth movement with the refinement of distraction devices and protocols and modification of osteotomy techniques.
References
Abbott, J. S. (1927). Letters to the Editor, American Journal of Public Health (NY), 17 (12) 1256-1257.
Publisher
Alcan, T. (2006). “A Miniature Tooth-Borne Distractor for the Alignment of Ankylosed Teeth,” The Angle Orthodontis, 76 (1) 77-83.
Publisher – Google Scholar
Allan, F. G. (1948). “Bone Lengthening,” The Journal of Bone and Joint Surgery. British, 30B (3) 490-505.
Publisher – Google Scholar
American Association of Orthodontists (1997). Clinical Practice Guidelines for Orthodontics and Dentofacial Orthopedics 1996, 111 (6) 443-449.
Publisher
Andrade, N., Gandhewar, T. & Kalra, R. (2011). “Development and Evolution of Distraction Devices: Use of Indigenous Appliances for Distraction Osteogenesis-An Overview,” Annals of Maxillofacial Surgery, 1 (1) 58-65.
Publisher – Google Scholar
Aronson, J. (1994). “Experimental and Clinical Experience with Distraction Osteogenesis,” The Cleft Palate-Craniofacial Journal, 31 (6) 473-482.
Publisher – Google Scholar
Biederman, W. (1956). “The Incidence and Etiology of Tooth Ankylosis,” American Journal of Orthodontics, (42) 921-926.
Publisher – Google Scholar
Biederman, W. (1962). “Etiology and Treatment of Tooth Ankylosis,” American Journal of Orthodontics, 48 (9) 670-684.
Publisher – Google Scholar
Castro-Govea, Y., Cervantes-Kardasch, V. H., Borrego-Soto, G., Martínez-Rodríguez, H. G., Espinoza-Juarez, M., Romero-Díaz, V., Marino-Martínez, I. A., Robles-Zamora, A., Ãlvarez-Lozano, E., Padilla-Rivas, G. R., Ortiz-López, R., Lara-Arias, J., Vázquez-Juárez, J. & Rojas-Martínez A. (2012). “Human Bone Morphogenetic Protein 2-Transduced Mesenchymal Stem Cells Improve Bone Regeneration in a Model of Mandible Distraction Surgery,” Journal of Craniofacial Surgery, 23 (2) 392-396.
Publisher – Google Scholar
Chang, H. Y., Chang, Y. L. & Chen, H. L. (2010). “Treatment of a Severely Ankylosed Central Incisor and a Missing Lateral Incisor by Distraction Osteogenesis and Orthodontic Treatment,” American Journal of Orthodontics & Dentofacial Orthopedics, 138 (6) 829-838.
Publisher – Google Scholar
Cheng, C. Y., Zen, E. C. & Su, C. P. (1997). “Surgical-Orthodontic Treatment of Ankylosis,” Journal of Clinical Orthodontics, 31 (6) 375-377.
Publisher – Google Scholar
Chin, M. & Toth, B. A. (1997). “Le Fort III Advancement with Gradual Distraction Using Internal Devices,” Plastic and Reconstructive Surgery, 100 (4) 819- 832.
Publisher – Google Scholar
Chung, K. R., Oh, M. Y. & Ko, S. J. (2001). “Corticotomy-Assisted Orthodontics,” Journal of Clinical Orthodontics, 35 (5) 331-339.
Publisher – Google Scholar
Codivilla, A. (1905). “On the Means of Lengthening, in the Lower Limbs, the Muscles and Tissues which are Shortened through Deformity,” The Journal of Bone & Joint Surgery, S2-2 (4) 353-369.
Publisher – Google Scholar
Cohen, S. R. & Holmes, R. E. (2001). “Internal le Fort III Distraction with Biodegradable Devices,” Journal of Craniofacial Surgery, 12 (3) 264-272.
Publisher – Google Scholar
Costantino, P. D., Friedman, C. D., Shindo, M. L., Houston, G. & Sisson, G. A. Sr (1993). “Experimental Mandibular Regrowth by Distraction Osteogenesis. Long-Term Results,” Archives of Otolaryngology, Head & Neck Surgery, 119 (5) 511-516.
Publisher – Google Scholar
Crawford, M. J. (1948). “Selection of Appliances for Typical Facial Fractures,” Oral Surgery, Oral Medicine, Oral Pathology, 1 (5) 442-451.
Publisher – Google Scholar
Dolanmaz, D., Karaman, A. I., Pampu, A. A. & Topkara, A. (2010). “Orthodontic Treatment of an Ankylosed Maxillary Central Incisor through Osteogenic Distraction,” The Angle Orthodontist, 80 (2) 391-395.
Publisher – Google Scholar
Fischgrund, J., Paley, D. & Suter, C. (1994). “Variables Affecting Time to Bone Healing during Limb Lengthening,”Clinical Orthopaedics & Related Research, (301) 31-37.
Publisher – Google Scholar
Frost, H. M. (1981). ‘The Regional Accelerated Phenomenon,’ Orthopedic Clinics of North America, (12) 725-726.
Gantes, B., Rathbun, E. & Anholm, M. (1990). “Effects on the Periodontium Following Corticotomy-Facilitated Orthodontics: Case Reports,” Journal of Periodontology, 61(4) 234-238.
Publisher – Google Scholar
Gateno, J., Teichgraeber, J. F. & Aguilar, E. (2000). “Computer Planning for Distraction Osteogenesis,” Plastic & Reconstructive Surgery, 105 (3) 873—882.
Publisher – Google Scholar
Grayson, B. H. & Santiago, P. E. (1999). “Treatment Planning and Biomechanics of Distraction Osteogenesis from an Orthodontic Perspective,” Seminars in Orthodontics, 5 (1) 9-24.
Publisher – Google Scholar
Gürgan, C. A., İşeri, H. & Kişnişçi, R. (2005). “Alterations in Gingival Dimensions Following Rapid Canine Retraction Using Dentoalveolar Distraction Osteogenesis,” European Journal of Orthodontics, 27 (4) 324—332.
Publisher – Google Scholar
Haas, A. J. (1961). “Rapid Palatal Expansion of the Maxillary Dental Apron and Nasal Cavity by Opening the Midpalatal Suture,” The Angle Orthodontist, (31) 73-79.
Publisher
Hegab, A. F. & Shuman, M. A. (2012). “Distraction Osteogenesis of the Maxillofacial Skeleton: Biomechanics and Clinical Implications,” 1:509. Doi: 10.4172/Scientific Reports. 509. [Retrieved Feb 15, 2013],http://www.omicsonline.org/scientific-reports/srep509.php#53.
Publisher
Ilizarov, G. A. (1988). “The Principles of the Ilizarov Method,” Bulletin of the Hospital for Joint Diseases Orthopaedic Institute, 48 (1) 1-11.
Publisher – Google Scholar
Ilizarov, G. A. (1989). “The Tension-Stress Effect on the Genesis and Growth of Tissues. Part I. The Influence of Stability of Fixation and Soft-Tissue Preservation,” Clinical Orthopaedics and Related Research, (238) 249-281.
Publisher – Google Scholar
Ilizarov, G. A. (1989). “The Tension-Stress Effect on the Genesis and Growth of Tissues: Part II. The Influence of the Rate and Frequency of Distraction,” Clinical Orthopaedics and Related Research, (239) 263-285.
Publisher – Google Scholar
Ilizarov, G. A. & Deviatov, A. A. (1969). “Surgical Lengthening of the Shin with Simultaneous Correction of Deformities,”Ortop Travmatol Protez, 30 (3) 32-37.
Publisher – Google Scholar
Im, J. J., Kye, M. K., Hwang, K. G. & Park, C. J. (2010). “Miniscrew-Anchored Alveolar Distraction for the Treatment of the Ankylosed Maxillary Central Incisor,” Dental Traumatology, 26 (3) 285-288.
Publisher – Google Scholar
Isaacson, R. J., Strauss, R. A., Bridges-Poquis, A., Peluso, A. R. & Lindauer, S. J. (2001). “Moving an Ankylosed Central Incisor Using Orthodontics, Surgery and Distraction Osteogenesis,” The Angle Orthodontist, 71 (5) 411-418.
Publisher – Google Scholar
İşeri, H., Bzeizi, N. & Kişnişci, R. (2001). ‘Rapid Canine Retraction Using Dentoalveolar Distraction Osteogenesis,’ [Abstract]. European Journal of Orthodontics, (23) 453.
Iseri, H., Kişnişci, R., Bzizi, N. & Tuz, H. (2005). “Rapid Canine Retraction and Orthodontic Treatment with Dentoalveolar Distraction Osteogenesis,” American Journal of Orthodontics & Dentofacial Orthopedics, 127 (5) 533-541.
Publisher – Google Scholar
Kanno, T., Mitsugi, M., Sukegawa, S., Hosoe, M. & Furuki, Y. (2008). “Computer-Simulated Bi-Directional Alveolar Distraction Osteogenesis,” Clinical Oral Implants Research, 19 (12) 1211-1218.
Publisher – Google Scholar
Karp, N. S., Thorne, C. H., Mccarthy, J. G. & Sissons, H. A. (1990). “Bone Lengthening in the Craniofacial Skeleton,”Annals of Plastic Surgery, 24 (3) 231-237.
Publisher – Google Scholar
Kazanjian, V. H. (1941). “The Interrelationship of Dentistry and Surgery in the Treatment of Deformities of the Face and Jaws,” American Journal of Orthodontics and Oral Surgery, (27) 10-19.
Publisher
Kharkar, V. R. & Kotrashetti, S. M. (2010). “Transport Dentoalveolar Distraction Osteogenesis-Assisted Rapid Orthodontic Canine Retraction,” Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 109 (5) 687-693.
Publisher – Google Scholar
Kharkar, V. R., Kotrashetti, S. M. & Kulkarni, P. (2010). “Comparative Evaluation of Dentoalveolar Distraction and Periodontal Distraction Assisted Rapid Retraction of the Maxillary Canine: A Pilot Study,” International Journal of Oral and Maxillofacial Surgery, 39 (11) 1074—1079.
Publisher – Google Scholar
Kim, Y. I., Park, S. B., Son, W. S., Kim, S. S., Kim, Y. D. & Mah, J. (2010). “Treatment of an Ankylosed Maxillary Incisor by Intraoral Alveolar Bone Distraction Osteogenesis,” American Journal of Orthodontics and Dentofacial Orthopedics, 138 (2) 215-220.
Publisher – Google Scholar
Kinzinger, G. S. M., Jänicke, S., Riediger, D. & Diedrich, P. R. (2003). “Orthodontic Fine Adjustment after Vertical Callus Distraction of an Ankylosed Incisor Using the Floating Bone Concept,” American Journal of Orthodontics and Dentofacial Orthopedics, 124 (5) 582-590.
Publisher – Google Scholar
Kişnişci, R. & Iseri, H. (2011). “Dentoalveolar Transport Osteodistraction and Canine Distalization,” Journal of Oral and Maxillofacial Surgery, 69 (3) 763-770.
Publisher – Google Scholar
Kişnişci, R., İşeri, H., Tüz, H. & Altuğ, A. (2002). “Dentoalveolar Distraction Osteogenesis for Rapid Orthodontic Canine Retraction,” Journal of Oral and Maxillofacial Surgery, 60 (4) 389-394.
Publisher – Google Scholar
Kofod, T., Würtz, V. & Melsen, B. (2005). “Treatment of an Ankylosed Central Incisor by Single Tooth Dento-Osseous Osteotomy and a Simple Distraction Device,” American Journal of Orthodontics and Dentofacial Orthopedics, 127 (1) 72-80.
Publisher – Google Scholar
Kumar, P. S., Saxena, R., Patil, S., Keluskar, K. M., Nagaraj, K. & Kotrashetti, S. M. (2009). “Clinical Investigation of Periodontal Ligament Distraction Osteogenesis for Rapid Orthodontic Canine Retraction,” Australian Orthodontic Journal,25 (2) 147-152.
Publisher – Google Scholar
Kurt, G., İşeri, H. & Kişnişci, R. (2010). “Rapid Tooth Movement and Orthodontic Treatment Using Dentoalveolar Distraction (DAD),” Angle Orthodontist, 80 (3) 597-606.
Publisher – Google Scholar
Liou, E. J. W. & Huang, C. S. (1998). “Rapid Canine Retraction through Distraction of the Periodontal Ligament,”American Journal of Orthodontics and Dentofacial Orthopedics, 114 (4) 372-382.
Publisher – Google Scholar
Liou, E. J. W., Figueroa, A. A. & Polley, J. W. (2000). “Rapid Orthodontic Tooth Movement Into Newly Distracted Bone after Mandibular Distraction Osteogenesis in a Canine Model,” American Journal of Orthodontics and Dentofacial Orthopedics, 117 (4) 391-398.
Publisher – Google Scholar
Long, H., Pyakurel, U., Wang, Y., Liao, L., Zhou, Y. & Lai, W. (2013). “Interventions for Accelerating Orthodontic Tooth Movement,” The Angle Orthodontist, 83 (1) 164-171.
Publisher – Google Scholar
Long, J., Li, P., Du, H. M., Liu, L., Zheng, X. H., Lin, Y. F., Wang, H., Jing, W., Tang, W., Chen, W. H. & Tian, W. D. (2011). “Effects of Bone Morphogenetic Protein 2 Gene Therapy on New Bone Formation during Mandibular Distraction Osteogenesis at Rapid Rate in Rabbits,” Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 112 (1) 50-57.
Publisher – Google Scholar
Markiewicz, M. R. & Bell, R. B. (2011). “Modern Concepts in Computer-Assisted Craniomaxillofacial Reconstruction,”Current Opinion in Otolaryngology & Head & Neck Surgery, 19 (4) 295-301.
Publisher – Google Scholar
Mavreas, D. & Athanasiou, A. E. (2008). “Factors Affecting the Duration of Orthodontic Treatment: A Systematic Review,” European Journal of Orthodontics, 30 (4) 386-395.
Publisher – Google Scholar
Mccarthy, J. G., Schreiber, J., Karp, N., Thorne, C. H. & Grayson, B. H. (1992). “Lengthening the Human Mandible by Gradual Distraction,” Plastic & Reconstructive Surgery, 89 (1) 1-8; Discussion 9-10.
Publisher – Google Scholar
Meehan, M., Morris, D., Maurer, C. R., Antony, A. K., Barbagli, F., Salisbury, K & Girod, S. (2006). “Virtual 3D Planning and Guidance of Mandibular Distraction Osteogenesis,” Computer Aided Surgery. 11 (2) 51-62.
Publisher – Google Scholar
Ohkubo, K., Susami, T., Mori, Y., Nagahama, K., Takahashi, N., Saijo, H. & Takato, T. (2011). “Treatment of Ankylosed Maxillary Central Incisors by Single-Tooth Dento-Osseous Osteotomy and Alveolar Bone Distraction,” Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 111 (5) 561-567.
Publisher – Google Scholar
Panjabi, M. M., Lindsey, R. W., Walter, S. D. & White, A. A. (1989). “The Clinician’s Ability to Evaluate the Strength of Healing Fractures from Plain Radiographs,” Journal of Orthopaedic Trauma, 3 (1) 29- 32.
Publisher – Google Scholar
Panjabi, M. M., Walter, S. D., Karuda, M., White, A. A. & Lawson, J. P. (1985). “Correlations of Radiographic Analysis of Healing Fractures with Strength: A Statistical Analysis of Experimental Osteotomies,” Journal of Orthopaedic Research, 3 (2) 212-218.
Publisher – Google Scholar
Phelan, M. K., Moss, R. B., Powell, R. S. & Womble, B. A. (1990). “Orthodontic Management of Ankylosed Teeth,”Journal of Clinical Orthodontics, 24 (6) 375-378.
Publisher – Google Scholar
Polley, J. W. & Figueroa, A. A. (1997). “Management of Severe Maxillary Deficiency in Children and Adolescence through Distraction Osteogenesis with an External, Adjustable, Rigid Distraction Device,” Journal of Craniofacial Surgery, 8 (3) 181-185.
Publisher – Google Scholar
Raschke, M. J., Bail, H., Windhagen, H. J., Kolbeck, S. F., Weiler, A., Raun, K., Kappelgard, A., Skiaerbaek, C. & Haas, N. P. (1999). “Recombinant Growth Hormone Accelerates Bone Regenerate Consolidation in Distraction Osteogenesis,” Bone 24 (2) 81—88.
Publisher – Google Scholar
Razdolsky, Y., El-Bialy, T. H., Dessner, S. & Buhler, J. E. Jr. (2004). “Movement of Ankylosed Permanent Teeth with a Distraction Device,” Journal of Clinical Orthodontics, 38 (11) 612-620.
Publisher – Google Scholar
Reitan, K. (1960). “Tissue Behaviour during Orthodontic Tooth Movement,” American Journal of Orthodontics, (46) 881-900.
Publisher – Google Scholar
Reitan, K. (1967). “Clinical and Histological Observations on Tooth Movement during and after Orthodontic Treatment,”American Journal of Orthodontics and Dentofacial Orthopedics, 53 (10) 721— 745.
Publisher
Rosenthal, W. (1930). ‘Therapie Der Mikrogenie,’ Sonntag E. and Rosenthal W., (Eds), Lehrbuch Der Mund- und Kieferchirurgie, Leipzig, Thieme.
Google Scholar
Roth, D. A., Gosain, A. K., Mccarthy, J. G., Stracher, M. A., Lefton, D. R. & Grayson, B. H. (1997). “A CT Scan Technique for Quantitative Volumetric Assessment of the Mandible after Distraction Osteogenesis,” Plastic & Reconstructive Surgery, 99 (5) 1237-1247; Discussion 1248-1250.
Publisher – Google Scholar
Samchukov, M. L., Cherkashin, A. M. & Cope, J. B. (1999). ‘Distraction Osteogenesis: History and Biologic Basis of New Bone Formation,’ Lynch, S.E., Genco, R.J. and Marx, R.E. (Eds), Tissue Engineering: Applications in Maxillofacial Surgery and Periodontics, Carol Stream, Quintessence.
Google Scholar
Sayin, S., Bengi, A. O., Gürton, A. U. & Ortakoğlu, K. (2004). “Rapid Canine Distalization Using Distraction of the Periodontal Ligament: A Preliminary Clinical Validation of the Original Technique,” The Angle Orthodontist, 74 (3) 304-315.
Publisher – Google Scholar
Shapurian, T., Damoulis, P. D., Reiser, G. M, Griffin, T. J. & Rand, W. M. (2006). “Quantitative Evaluation of Bone Density Using the Hounsfield Index,” Oral & Craniofacial Tissue Engineering, 21 (2) 290-297.
Publisher – Google Scholar
Smatt, V., Gibeili, Z., Rahmi, H., Robin, M., Vanzo, L. & Smatt, Y. (1999). ‘Alveolar Mandibular Reconstruction by Axial Vertical Distraction Osteogenesis and Oncology,’ Diner, P.A. and Vasquez, M.P., (Eds), Second International Congress on Cranial and Facial Bone Distraction Processes, Paris, France, June 17-19,1999; Bologna, Italy, Monduzzi Editore, 1999.
Google Scholar
Smith, S. W., Sachdeva, R. C. L. & Cope, J. B. (1999). “Evaluation of the Consolidation Period during Osteodistraction Using Computed Tomography,” American Journal of Orthodontics and Dentofacial Orthopedics, 116 (3) 254-263.
Publisher – Google Scholar
Snyder, C. C., Levine, G. A., Swanson, H. M. & Browne Jr, E. Z. (1973). “Mandibular Lengthening by Gradual Distraction: Preliminary Report,” Plastic & Reconstructive Surgery, 51 (5) 506-508.
Publisher – Google Scholar
Spencer, A. C., Campbell, P. M., Dechow, P., Ellis, M. L. & Buschang, P. H. (2011). “How Does the Rate of Dentoalveolar Distraction Affect the Bone Regenerate Produced?,” American Journal of Orthodontics and Dentofacial Orthopedics, 140 (5) E211-221.
Publisher – Google Scholar
Sukurica, Y., Karaman, A., Gürel, H. G. & Dolanmaz, D. (2007). “Rapid Canine Distalization through Segmental Alveolar Distraction Osteogenesis,” The Angle Orthodontist, 77 (2) 226-236.
Publisher – Google Scholar
Susami, T., Matsuzaki, M., Ogihara, Y., Sakiyama, M., Takato, T., Sugawara, Y. & Matsumoto, S. (2006). “Segmental Alveolar Distraction for the Correction of Unilateral Open-Bite Caused by Multiple Ankylosed Teeth: A Case Report,”European Journal of Orthodontics, 33 (3) 153-159.
Publisher – Google Scholar
Swennen, G., Schliephake, H., Dempf, R., Schierle, H. & Malevez, C. (2001). “Craniofacial Distraction Osteogenesis: A Review of the Literature,” International Journal of Oral and Maxillofacial Surgery, 30 (2) 89-103.
Publisher – Google Scholar
Tjernstrom, B., Thoumas, K. A. & Pech, P. (1992). “Bone Remodeling after Leg Lengthening: Evaluation with Plain Radiographs, Computed Tomography, and Magnetic Resonance Imaging Scans,” Journal of Pediatric Orthopaedics, 12 (6) 751-755.
Publisher – Google Scholar
Toth, B. A., Kim, J. W., Chin, M. & Cedars, M. (1998). “Distraction Osteogenesis and Its Application to the Midface and Bony Orbit in Craniosynostosis Syndromes,” Journal of Craniofacial Surgery, 9 (2) 100-113.
Publisher – Google Scholar
Urbani, G., Consolo, U., Lombardo, G. & Bernini, R. (1999). ‘Use of Miniaturized Intraoral Alveolar Distractors in Human Subjects,’ Diner, P.A. and Vasquez, M.P., (Eds), Second International Congress on Cranial and Facial Bone Distraction Processes, Paris, France, June 17-19, 1999; Bologna, Italy, Monduzzi Editore, 1999.
Google Scholar
Vig, P. S., Weintraub, J. A., Brown, C. & Kowalski, C. J. (1990). “The Duration of Orthodontic Treatment with and without Extractions: A Pilot Study of Five Selected Practices,” American Journal of Orthodontics and Dentofacial Orthopedics, 97(1) 45—51.
Publisher – Google Scholar
Wilcko, W. M., Wilcko, T., Bouquot, J. E. & Ferguson, D. J. (2001). “Rapid Orthodontics with Alveolar Reshaping: Two Case Reports of Decrowding” The International Journal of Periodontics and Restorative Dentistry, 21 (1) 9-19.
Publisher – Google Scholar
Yamauchi, K., Mitsugi, M. & Takahashi, T. (2007). “Biodegradable Screw Fixation in Maxillofacial Distraction Osteogenesis,” Journal of Oral and Maxillofacial Surgery, 65 (9) 1859-1861.
Publisher – Google Scholar
Zakaria, O., Kon, K. & Kasugai, S. (2012). “Evaluation of a Biodegradable Novel Periosteal Distractor,” Journal of Biomedical Materials Research Part B: Applied Biomaterials, 100 (3) 882-889.
Publisher – Google Scholar