Close anatomical and embryological relations between the parathyroid glands and the thymus can lead to the appearance of rare but various associations between hyperparathyroidism producing lesions with benign or malignant thymoma Therefore outside primary hyperparathyroidism, ectopic secretion of PTH or PTH related protein and MEN type 1, our case is one of the few observations of glandular hyperplasia in CKD-MBD coexisting with thymoma described by Palmer and Sawyer (1978), Byrne et al(1989), Suzuki T et al (1997), Suzuki K et al (1998), De Toma et al (20010 and Palin et al (2009).
The routinely excision of the upper retrosternal tissue during surgery of RHp recommended by Rizzoli et al (1994), Welch et al (2012) and Maria et al (2013) can reveal outside of ectopic or supernumerary glands the presence of cellular nests or even constituted thymic tumors.
The clinical aspects of this concurrent pathology are mixed, the long standing evolution on hemodialysis and annoying combined features of ESRD and parathyroid hy-perfunction prevailing the discrete presence of a benign noninvasive thymoma or even the symptomatic course more or less rapid of a malignant tumor. Therefore the progressive osteoarthicular pains, neuromuscular and even psychiatric complaints, ectopic calcifications and calciphylaxy or intense pruritus dominate and masks the asymptomatic evolution or nonspecific manifestations of an incipient or even malignant thymoma: fever, sweating, weight loss or belated appearing dyspnea, cough, compressive signs etc.
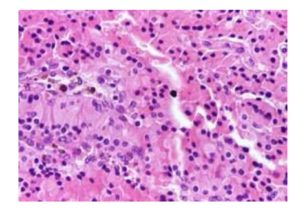
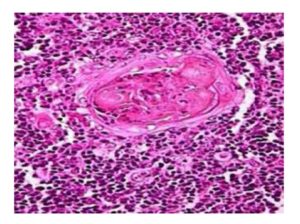
Laboratory usual tests revealed normal calcemia but raised iPTH and of course ure-mia and hypercreatinemia of renal HP. Selected investigations can be used only to look for detecting associated problems or tumor spread in thymoma: full blood count electrophoresis and anti-acetylcholine-receptors ( indicative for malignancy) Imaging resort to ultrasound and sestamibi scan in RHp and to chest X-ray, high un- hanced contrast CT scan and MR scan for thymoma as Mari et al (1999) and Ceriani et al (2008) and the lesion may be sampled with a CT guided needle biopsy. A third of these tumors are discovered serendipitous due to chest radiography or CT for imaging of other conditions, for screening purpose or, as in our case, intraoperatively at surgery for any cervical or thoracic lesions. However the final diagnosis in thymoma is the histopathological examina-tion of the surgical specimen.
Despite various advances in medical therapy, parathyroidectomy is a pragmatic symptomatic therapy in cases of RHp appearing in patients under maintenance dialysis but the optimal technique must be individualized in each case and still to be debated. For us, the best solution for aggressive, refractory forms of RHp is total para-thyroidectomy without auto-transplantation. Even if our patient had no clinical signs and symptoms for myasthenia gravis complete exeresis of the thymic tumor occurred as the most favorable curative alternative.
Conclusion
Coexistence of the main types of hyperparathyroidism and thymoma is probably coincidentally and in the lack of myasthenic features the diagnosis can be established only by chance, imaging methods or surgery on a neighboring organ. Although rare the operating surgeon must be aware of possible presence of such pathology. Concomitant exeresis of all hyperplastic parathyroids together with the thymic tumor will achieve cure of both lesions.
The authors declare that they have no competing interest All authors read and approved the final manuscrip Author’s contribution: DMR- conceived the study and performed surgery, GM- performed surgery, G — expertise in pathology, DS – drafted the paper, corresponding author
References
1.Palmer FJ, Sawyers TM: Hyperparathyroidism, chemodectoma , thymoma and myasthenia gravis (1978). Archives of Internal Medicine , 138(9) :1402-3
Publisher
2.Byrne AJ, Gunn A, Davidson DLW, Paterson CR (1989): Parathyroid hyperplasia associated with thymoma. Postgraduated Medical Journal 65(763): 310-1
Published
3.Suzuki T, Suzuki S, Kitami A, Hori G, Inoue T, Suzuki S (1997): A thymoma associated with hyperparathyroidism. Thorac Cardiovasc Surg (), 45(4): 211-2
Publisher
4.Suzuki K, Tanaka K, Shibusa S, Shibuya Y, Inuzuka M, Fujishima T et al (1998): Parathyroid- hormone-related-protein-producing thymic carcinoma presenting as a giant extrathoracic mass. Respiration, 65(1): 83-5
Publisher
5.De Toma G, Placco M, Nicolati V, Brozzetti S, Letizia C, Cavallaro A (2001): Type B1 thymoma thymoma in multiple endocrine neoplasia (MEN-1) syndrome. Tumori , 87(4): 266-8
6.Palin SL, Singh B (2009): Primary hyperparathyroidism due to a parathyroid adenoma with subsequent miasthenia gravis. Quarterly Journal of Medicine, 93(8): 560-1
Publisher – Google Scholar
7.Rizzoli R, Pache JC, Didierjean L, Burger A, Bonjour JP (1994): A thymoma as a cause of true ecto-pic hyperparathyroidism. The Journal of Clinical Endocrinology & Metabolism, 79(3): 912-5
8.Welch K, McHenry CR (2012): The role of transcervical thymectomy in patients with hyperparathyroidism. AmericanJournal of Surgery, 203(3): 292-5
Publisher
9.Maria V, Saad M, Ioannis F (2013): Parathyroid adenoma associated thymoma in a female adult with primary hyperparathyroidism. International Journal of Surgery Case Reports, 4(1): 105-7
Publisher – Google Scholar
10.Mari C, Leon J, Farrerons J, Matis-Guiu X, Tembl A, Martin JC et al (1999): Thymic carcinoid and parathyroid hyperplasia detection with 99mTc-MIBI men type. Journal of Endocrinological Investigation, 22(10): 803-7
11.Ceriani L, Giovanella L (2008): Simultaneous imaging of pericardic thymoma and parathyroid adenoma by sestamibi scan. Clinical Nuclear Medicine, 33(8): 542-4
Publisher
12.L, Giovanella L: Simultaneous imaging of pericardic thymoma and parathyroid ade-noma by sestamibi scan (2008). Clinical Nuclear Medicine 33(8): 542-4