Introduction
Anterior Cruciate Ligament (ACL) reconstruction is an established and widely practiced surgical procedure with proven efficacy and a low morbidity profile (Gillquist & Odensten 1988; Paulos et al. 1991; Haug et al. 2000; Ruiz et al. 2002; McCulloch et al. 2007). Over recent years there have been many evolving trends in ACL reconstruction practice (Ruiz et al. 2002; McCulloch et al. 2007). Open reconstruction has moved towards all arthroscopic surgery (Gillquist & Odensten 1988; Ruiz et al. 2002; McCulloch et al. 2007). The predominance of patella bone tendon bone (BTB) graft has been replaced by hamstring (HS) graft (Kartus et al. 2001; Taylor et al. 2009; Samuelsson et al. 2009). Operative technique now favours trans-medial portal femoral drilling over trans-tibial femoral drilling (Araujo et al. 2011; Iriuchishima et al. 2011). The last of these has facilitated more anatomical femoral tunnel placement, and in recent years the possibility of developing a multiple bundle reconstructive technique as well as an anatomic single bundle reconstruction (Shafizadeh et al. 2011; Zelle et al. 2006; Tanaka et al. 2012; Karlsson et al. 2011).
Another significant trend that developed over the 1990’s was that of rapid rehabilitation and day surgery ACL reconstruction (Decarlo et al. 1992; Shelbourne & Dersam 2003; Cappellino et al. 2012; Ardern et al. 2011; Coşkunsu et al. 2010; Kruse et al. 2012). Anecdotally, there has been a move back towards a more conservative course of rehabilitation. The risks of early graft failure, secondary to either rupture or late laxity, are cited as potential risks of aggressive rapid rehabilitation regimens (Heijne & Werner 2007; Andersson et al. 2009; Zhu et al. 2013).
Several studies have examined the effect that graft choice has on rehabilitation considerations (Samuelsson et al. 2009; Shelbourne & Dersam 2003; Coşkunsu et al. 2010; Andersson et al. 2009), or the evidence for individual aspects of rehabilitation (Heijne & Werner 2007; van Grinsven et al. 2010; Wright & Fetzer 2007; Shelbourne & Nitz 1990). There is no published research that examines the different practices in ACL rehabilitation. Although rehabilitation regimens are constructed in conjunction with operating surgeons, to a large extent, it is physiotherapists who monitor patient progression and decided how quickly they advanced to further milestones based on limb proprioception, muscle strength discrepancies, range of movement, pain and patient confidence.
With the aim of better understanding variations in current practices of ACL rehabilitation in the UK, we conducted a survey of all the physiotherapy departments that provide rehabilitation for patients undergoing isolated ACL reconstruction in the Greater London area within the NHS (National Health Service- State healthcare).
Materials and Methods
Ethical approval was sought from our local research and ethics committee. Formal endorsement was deemed unnecessary due to the intrinsic nature of the study and lack of patient involvement, or the use of any patient level data.
All hospital orthopaedic departments within the M25 (Greater London ring road) were identified with the aid of the NHS Direct website (NHS Direct 2011). Each hospital physiotherapy department was contacted by telephone, and a physiotherapist was surveyed. This process frequently required multiple attempts for an appropriate and available physiotherapist to be identified. Departments were deemed non-respondents after an appropriate physiotherapist could not be contacted following a minimum of 5 attempts via telephone on five separate days, two attempts by e-mail, and a personal visit by a researcher.
On contacting a physiotherapy department, we ascertained if they were routinely involved with rehabilitating ACL reconstruction patients. If this were the case, we specifically asked to speak to a senior physiotherapist who was regularly involved in the rehabilitation of such patients. The purpose of the study was verbally outlined, including the information required (i.e. their guidelines only and no patient details etc.) and verbal consent was obtained.
The physiotherapists were asked how many surgeons performed ACL reconstruction at their institution, if their unit practised predominantly in-patient or day-surgery ACL reconstruction, if bracing was commonly used, and if there was a written post ACL reconstruction rehabilitation protocol in their department. We also enquired specifically about the time-line for rehabilitation milestones: Full weight bearing, removal of brace (If used), cycling, straight line running, running with cutting/pivoting and the expected return to contact sport or high risk activity such as skiing
Result
54 physiotherapy departments were identified form the NHS direct website. From this result, 39 departments were identified within the greater London area as providing rehabilitation for patients undergoing ACL Reconstruction. Of these, 38 (97.4%) were included in our study, and 1 (2.6%) failed to respond.
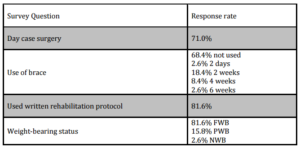
Table 1 summarises the results of surgery type, written protocol use, brace use and weight bearing status immediately post op. Day surgery ACL reconstruction was performed routinely at 27 (71.0%) units, with 11 (28.9%) units performing all ACL reconstructions as in-patient procedures. 31 (81.6%) of the departments that responded had written rehabilitation guidelines, with 7 (18.4%) performing rehabilitation without any written guidelines.
Table 1: Summary of immediate post-operative rehabilitation
The majority of departments, 31 (81.6%), adopted immediate post-operative full weight bearing, 6 (15.8%) allowed partial weight bearing, and 1 (2.6%) managed their patients as non-weight bearing. Of the 7 departments that did not allow immediate full weight bearing, it was permitted at 2 weeks following surgery.
Braces were only used in 12 (31.6%) departments. Where braces were used, they were worn for 2 days at 1 department, 2 weeks at 7 departments, 4 weeks at 3 departments, and 6 weeks at 1 department.
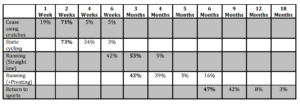
Table 2: Anticipated achievement of rehabilitation milestones
The expected achievement of rehabilitation milestones in the 38 physiotherapy departments included in the study. The most common result for a milestone is highlighted in bold.
Table 2 illustrates anticipated achievement of rehabilitation milestones. Specific results are as follows:
- Free of crutches at 1 week: 7 (18.4%), 2 weeks: 27 (71.0%), 4 weeks: 2 (5.3%), and 6 weeks: 2 (5.3%).
- Allowed to cycle at 2 weeks: 28 (73.7%), 4 weeks: 9 (23.7%), and 6 weeks: 1 (2.6%).
- Allowed to return to straight line running at 6 weeks: 16 (42.1%), 12 weeks: 20 (52.6%), and 16 weeks: 2 (5.3%).
- Allowed to return to running with cutting and twisting at 3 months: 16 (42.1%), 4 months: 15 (39.5%), 5 months:
1 (2.6%), and 6 months: 6 (15.8%).
- Allowed to return to contact and high-risk sports at 6 months: 18 (47.4%), 9 months: 16 (42.1%), 12 months: 3 (7.9%) and 18 months: 1 (2.6%).
Discussion
The purpose of this study was to investigate the contemporary practices of physiotherapy departments in London, with regards to rehabilitation following ACL reconstruction. Through our efforts we achieved a response rate of 97.4% of all relevant physiotherapy departments. Our survey demonstrates a significant trend towards day case ACL reconstruction, with immediate full weight bearing. Within the departments surveyed, there was a significant trend towards rapid rehabilitations, with both early cycling, and return to contact and high-risk sports at 6 months.
There are few studies that have investigated the topic of our research. Lobb et al (2012) recently reviewed systematic reviews on ACL reconstruction rehabilitation, looking at the strength of evidence behind individual components of regimens. They concluded that many RCTs lacked detail on the use of different treatments at different time points, what the comparative ‘standard treatment’ was, or the amount of physiotherapy input. They also found that all but one of the reviews included in their work had higher risks of bias when graded by the PRISMA quality checklist. As a result they found limited evidence to support any particular rehabilitation therapy (Lobb et al. 2012). Poor methodology with lack of standardisation, and increased risk of bias, does not appear to be an isolated finding among reviews of rehabilitation protocols (Johnson & Beynnon 2012).
Francis et al (2001) conducted a postal survey aimed at British surgeons who performed ACL reconstruction. They specifically sought details on graft choice, operative timing, bracing post operatively, rehabilitation and outcome measures. Regarding post operative bracing, they found a mixed response, with 30% of surgeons using braces, comparable to the 31.6% we found. There were a variety of restrictions on the range of movement within the brace, and the longest period of use was 3 months. With regards to rehabilitation, only half of the participants gave details regarding their own protocols. 36% aimed to have their patients running at 4 months and 59% aimed to have a return to sport by 6 months. This study did not present their results regarding rehabilitation in great detail, preventing any useful analysis or comparison to our findings.
Coşkunsu et al surveyed 55 surgeons in Turkey regarding surgical technique, pre-operative prerequisites and rehabilitation approaches in 2010. Although they specifically asked about rehabilitation regimens and milestones in an email survey, they focussed more on graft choice, differences in post-operative practice based on that choice and the evidence for specific post-operative adjuncts such as braces and continuous passive movement (CPM). A second article by the Australian group Feller et al in 2002 was quite similar. They also focussed more on the achievement of rehabilitation milestones in relation to graft type, finding no significant difference between the two. Both these studies contacted the surgeons performing the operations, and not the physiotherapists actually conducting the rehabilitation.
In our findings, the majority of units (71%) practice day-surgery ACL reconstruction, representing a significant change in practice over the last decade. This change has been made possible by the adoption of all arthroscopic techniques, reducing the pressures upon in-patient beds as well as resulting in a reduced cost profile for the procedure.
Bracing following ACL reconstruction acts to rest the surgical wounds and soft tissue envelope, and reduce early cycling of the graft, prior to graft incorporation. The majority of units no longer use bracing. When braces were adopted, they were predominantly used for between 2 and 4 weeks. In one instance, braces were used for only 2 days, this was found to be precautionary, so as to support weight bearing during loss of limb control secondary to regional anaesthesia such as a lumber plexus or femoral nerve block. The evidence for bracing has been extensively investigated, with no long-term benefit being identified from their use (Grant 2013; Lobb et al. 2012; van Grinsven et al. 2010; Wright & Fetzer 2007). It has been pointed out that systematic reviews on this topic have primarily examined patella tendon grafts, and that there is a lack of evidence regarding hamstring grafts (Coşkunsu et al. 2010). A previous survey of British surgeons in 2001 found that a similar number used braces compared to our results (Francis et al. 2001), showing little changes in attitudes to braces over the last decade in the UK, in spite of the evidence. Although we found that just under a third of patients are still braced, this level is much lower compared with other similar articles (Coşkunsu et al. 2010; Feller et al. 2002), implying that there may be international trends which also govern their use, not just clinical evidence.
7 (18.4%) of the departments surveyed, had no written guidelines for rehabilitation. Patients may frequently see multiple therapists throughout the course of their treatment in large physiotherapy departments. Written protocols allow the delivery of care to be delivered consistently. It is crucial that surgeons and their physiotherapy departments work closely to establish written agreed guidelines to act as a framework to guide rehabilitation.
The use of accelerated rehabilitation following ACL reconstruction was advocated in the early 1990s (Decarlo et al. 1992; Shelbourne & Nitz 1990; Fu et al. 1992), with authors advocating return to contact and high risk sports as early as 2 months following reconstruction (Shelbourne & Nitz 1990). Early rehabilitation has been implicated in delayed graft incorporation, tunnel widening and graft failure by means of both rupture and late laxity (Decarlo et al. 1992; Shelbourne & Dersam 2003; Ardern et al. 2011; Coşkunsu et al. 2010). However, the evidence is not so clear cut; more recent studies have found there is no difference between conventional and more aggressive, accelerated rehabilitation regimens (Grant 2012; Christensen et al. 2013). There are more recent investigations into specific neurocognitive and neuromuscular approaches to ACL reconstruction, with the evidence showing encouraging results (Cappellino et al. 2012; Grant 2013).
Ligament registries have recently been introduced in order to help identifying risk factors that lead to degenerative joint disease, graft failure, meniscal failure and failure to return to sports (Granan, Forssblad, et al. 2009; Granan et al. 2008; Ytterstad et al. 2011). The focus of registries has been upon surgical techniques, graft types, fixation types and implants. Ligament registries thus far have not collected data on rehabilitation regimens and corresponding milestones (Granan, Bahr, et al. 2009; Granan, Forssblad, et al. 2009; Granan et al. 2008; Engebretsen & Forssblad 2009). Over aggressive rehabilitation has been associated with ACL graft rupture and late laxity (Heijne & Werner 2007; Andersson et al. 2009). As rehabilitation can occur for many months after the operation, it seems obtuse that this factor is not considered when analysing the outcomes of ACL reconstruction. Due to this fact, ligament registries should consider collecting data on rehabilitation regimens, such that the impact of differing practices on the failure of grafts may be better understood.
Conclusion
There remains considerable variation in the post-operative practices and rehabilitation regimens after isolated ACL reconstruction, which has not been considered with regards to outcome. Currently, the majority of procedures are conducted as Day Case surgery, with immediate full weight bearing, without bracing and anticipating a return to all sports at 6 months. Physiotherapists closely monitor the progression of rehabilitation, and play a vital role in advancing patients to the next level of exercises at their appropriate time. National ligament registries should consider collecting data on post-operative rehabilitation as it plays a significant role in the success of the intervention.
References
1. Andersson, D., Samuelsson, K. & Karlsson, J., 2009. Treatment of anterior cruciate ligament injuries with special reference to surgical technique and rehabilitation: an assessment of randomized controlled trials. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association, 25(6), pp.653–85.
Google Scholar
2. Araujo, P.H. et al., 2011. Advances in the three-portal technique for anatomical single- or double-bundle ACL reconstruction. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA, 19(8), pp.1239–42.
3. Ardern, C.L. et al., 2011. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. The American journal of sports medicine, 39(3), pp.538–43.
Publisher – Google Scholar
4. Cappellino, F. et al., 2012. Neurocognitive rehabilitative approach effectiveness after anterior cruciate ligament reconstruction with patellar tendon. A randomized controlled trial. European journal of physical and rehabilitation medicine, 48(1), pp.17–30.
5. Christensen, J.C., Goldfine, L.R. & West, H.S., 2013. The effects of early aggressive rehabilitation on outcomes after anterior cruciate ligament reconstruction using autologous hamstring tendon: a randomized clinical trial. Journal of sport rehabilitation, 22(3), pp.191–201.
Google Scholar
6. Coşkunsu, D., Bayrakcı Tunay, V. & Akgün, I., 2010. Current trends in reconstruction surgery and rehabilitation of anterior cruciate ligament in Turkey. Acta orthopaedica et traumatologica turcica, 44(6), pp.458–63.
7. Decarlo, M.S. et al., 1992. Traditional versus Accelerated Rehabilitation following ACL Reconstruction: A One-Year Follow-Up. The Journal of orthopaedic and sports physical therapy, 15(6), pp.309–16.
Publisher – Google Scholar
8. Engebretsen, L. & Forssblad, M., 2009. Why knee ligament registries are important… Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA, 17(2), pp.115–6.
9. Feller, J.A., Cooper, R. & Webster, K.E., 2002. Current Australian trends in rehabilitation following anterior cruciate ligament reconstruction. The Knee, 9(2), pp.121–6.
Publisher – Google Scholar
10. Francis, A., Thomas, R.D. & McGregor, A., 2001. Anterior cruciate ligament rupture: reconstruction surgery and rehabilitation. A nation-wide survey of current practice. The Knee, 8(1), pp.13–8.
Publisher – Google Scholar
11. Fu, F.H., L-Y Woo, S. & Irrgang, J.J., 1992. Current Concepts for Rehabilitation following Anterior Cruciate Ligament Reconstruction. The Journal of orthopaedic and sports physical therapy, 15(6), pp.270–8.
Publisher – Google Scholar
12. Gillquist, J. & Odensten, M., 1988. Arthroscopic reconstruction of the anterior cruciate ligament. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association, 4(1), pp.5–9.
13. Granan, L.-P. et al., 2008. Development of a national cruciate ligament surgery registry: the Norwegian National Knee Ligament Registry. The American journal of sports medicine, 36(2), pp.308–15.
Publisher – Google Scholar
14. Granan, L.-P., Forssblad, M., et al., 2009. The Scandinavian ACL registries 2004-2007: baseline epidemiology. Acta orthopaedica, 80(5), pp.563–7.
Publisher – Google Scholar
15. Granan, L.-P., Bahr, R., et al., 2009. Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears: a cohort study based on the Norwegian National Knee Ligament Registry. The American journal of sports medicine, 37(5), pp.955–61.
Publisher – Google Scholar
16. Grant, J.A., 2012. Does accelerated rehabilitation affect knee joint laxity after ACL reconstruction? Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine, 22(6), pp.523–4.
17. Grant, J.A., 2013. Updating Recommendations for Rehabilitation after ACL Reconstruction: a Review. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine, 23(6), pp.501–2.
Google Scholar
18. Van Grinsven, S. et al., 2010. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA, 18(8), pp.1128–44.
Google Scholar
19. Haug, M., Sørensen, L. & Dichmann, O., 2000. Anterior cruciate ligament reconstruction as a day case with extended recovery. Ambulatory surgery, 8(4), pp.171–173.
Publisher – Google Scholar
20. Heijne, A. & Werner, S., 2007. Early versus late start of open kinetic chain quadriceps exercises after ACL reconstruction with patellar tendon or hamstring grafts: a prospective randomized outcome study. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA, 15(4), pp.402–14.
Google Scholar
21. Iriuchishima, T. et al., 2011. In vitro and in vivo AM and PL tunnel positioning in anatomical double bundle anterior cruciate ligament reconstruction. Archives of orthopaedic and trauma surgery, 131(8), pp.1085–90.
Publisher – Google Scholar
22. Johnson, R.J. & Beynnon, B.D., 2012. What do we really know about rehabilitation after ACL reconstruction?: commentary on an article by L.M. Kruse, MD, et al.: “rehabilitation after anterior cruciate ligament reconstruction. a systematic review”. The Journal of bone and joint surgery. American volume, 94(19), pp.e148(1–2).
23. Karlsson, J. et al., 2011. Anatomic single- and double-bundle anterior cruciate ligament reconstruction, part 2: clinical application of surgical technique. The American journal of sports medicine, 39(9), pp.2016–26.
Publisher – Google Scholar
24. Kartus, J., Movin, T. & Karlsson, J., 2001. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association, 17(9), pp.971–80.
25. Kruse, L.M., Gray, B. & Wright, R.W., 2012. Rehabilitation after anterior cruciate ligament reconstruction: a systematic review. The Journal of bone and joint surgery. American volume, 94(19), pp.1737–48.
26. Lobb, R., Tumilty, S. & Claydon, L.S., 2012. A review of systematic reviews on anterior cruciate ligament reconstruction rehabilitation. Physical therapy in sport : official journal of the Association of Chartered Physiotherapists in Sports Medicine, 13(4), pp.270–8.
Google Scholar
27. McCulloch, P.C. et al., 2007. An illustrated history of anterior cruciate ligament surgery. The journal of knee surgery, 20(2), pp.95–104.
Google Scholar
28. NHS Direct, 2011. http://www.nhs.uk/servicedirectories/Pages/ServiceSearch.aspx.
29. Paulos, L.E. et al., 1991. Anterior cruciate ligament reconstruction with autografts. Clinics in sports medicine, 10(3), pp.469–85.
Google Scholar
30. Ruiz, A.L., Kelly, M. & Nutton, R.W., 2002. Arthroscopic ACL reconstruction: a 5-9 year follow-up. The Knee, 9(3), pp.197–200.
Publisher – Google Scholar
31. Samuelsson, K., Andersson, D. & Karlsson, J., 2009. Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association, 25(10), pp.1139–74.
32. Shafizadeh, S. et al., 2011. Precision of tunnel positioning in navigated anterior cruciate ligament reconstruction. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association, 27(9), pp.1268–74.
33. Shelbourne, K. & Dersam, M., 2003. The evolution of rehabilitation for anterior cruciate ligament reconstruction. In R. Williams & D. Johnson, eds. Controversies in orthopaedic surgery: sports injuries to the knee. Oxford University Press, pp. 135–50.
34. Shelbourne, K.D. & Nitz, P., 1990. Accelerated rehabilitation after anterior cruciate ligament reconstruction. The American journal of sports medicine, 18(3), pp.292–9.
Publisher – Google Scholar
35. Tanaka, Y. et al., 2012. Triple-bundle ACL grafts evaluated by second-look arthroscopy. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA, 20(1), pp.95–101.
36. Taylor, D.C. et al., 2009. Patellar tendon versus hamstring tendon autografts for anterior cruciate ligament reconstruction: a randomized controlled trial using similar femoral and tibial fixation methods. The American journal of sports medicine, 37(10), pp.1946–57.
Publisher – Google Scholar
37. Wright, R.W. & Fetzer, G.B., 2007. Bracing after ACL reconstruction: a systematic review. Clinical orthopaedics and related research, 455, pp.162–8.
Publisher – Google Scholar
38. Ytterstad, K., Granan, L.-P. & Engebretsen, L., 2011. [The Norwegian Cruciate Ligament Registry has a high degree of completeness]. Tidsskrift for den Norske lægeforening : tidsskrift for praktisk medicin, ny række, 131(3), pp.248–50.
Google Scholar
39. Zelle, B.A. et al., 2006. Anatomical double-bundle anterior cruciate ligament reconstruction. Sports medicine (Auckland, N.Z.), 36(2), pp.99–108.
Publisher – Google Scholar
40. Zhu, W. et al., 2013. Anterior cruciate ligament (ACL) autograft reconstruction with hamstring tendons: clinical research among three rehabilitation procedures. European journal of orthopaedic surgery & traumatology : orthopédie traumatologie, 23(8), pp.939–43.
Google Scholar