1. Deutsch, A. S. & Musikant, B. L. (2004). “Morphological Measurements of Anatomic Landmarks in Human Maxillary and Mandibular Molar Pulp Chambers,” Journal of Endodontics, 30 (6) 388-390.
Publisher – Google Scholar
2. Deutsch, A. S., Musikant, B. L., Gu, S. & Isidro, M. (2005). “Morphological Measurements of Anatomic Landmarks in Pulp Chambers of Human Maxillary Furcated Bicuspids,” Journal of Endodontics 31 (8) 570-573.
Publisher – Google Scholar
3. Belli, S., Cobankara, F. K., Eraslan, O., Eskitascioglu, G. & Karbhari, V. (2006). “The Effect of Fiber Insertion on Fracture Resistance of Endodontically Treated Molars with MOD Cavity and Reattached Fractured Lingual Cusps,”Journal of Biomedical Materials Research 79 (1) 35-41.
Publisher – Google Scholar
4. Bowen, R. L. & Rodriguez, M. S. (1962). “Tensile Strength and Modulus of Elasticity of Tooth Structure and Several Restorative Materials,” Journal of American Dental Associacion, 64 378-387.
Publisher – Google Scholar
5. Braga, R. R., Hilton, T. J. & Ferracane, J. L. (2003). “Contraction Stress of Flowable Composite Materials and Their Efficacy as Stress-Relieving Layers,” Journal of American Dental Associacion 134 721—728.
Publisher – Google Scholar
6. Brunthaler, A., Lucas, T., Sperr, W. & Schedle, A. (2002). ‘Longevity of Direct Resin Composite Restorations in Posterior Teeth,’ Received Published online: 27 May 2003.
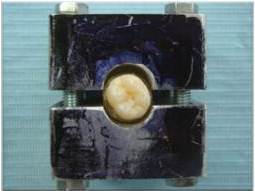
7. Ciocan, L.T., Iordache, B., Gălbinașu, B. & Pătrașcu, I. (2012). Invention Brevet no 122801 ‘Equipment for Testing the Cohesion of Mixed Dental Materials,’ State Office of Invention Nd Trademark, România.
8. Çötert, H. S., Sen, B. H. & Balkan, M. (2001). “In Vitro Comparison of Cuspal Fracture Resistances of Posterior Teeth Restored with Various Adhesive Restorations,” International Journal of Prosthodontics 14 374—378.
Publisher – Google Scholar
9. Craig, G. R. (2001). ‘Materiale Dentare Restauratoare,’ All Educațional, București, România.
10. Fennis, W. M. M., Kreulen, C. M., Tezvergil, A., Lassila, L. V. J., Vallittu, P. K. & Creugers, N. H. J. (2011). “In Vitro Repair of Fractured Fiber-Reinforced Cusp-Replacing Composite Restorations,” International Journal of Dentistry, article ID 165938.
Publisher – Google Scholar
11. Fusuyama, T. (1980). ‘New Concepts in Operative Dentistry: Differentiating Two Layers of Carious Dentin and Using an Adhesive Resin,’ Quintessence Publishing Co, Chicago, Il.
Google Scholar
12. Gatin, E., Matei, E., Pîrvu, D. A., Gălbinașu, B. M. & Iordache, S. (2012). “Comparative Survey of the Most Used Self Adhesive Dental Cements Based on Resin Composites,” Digest Journal of Nanomaterials and Biostructures, 7 (1) 207-214.
Publisher – Google Scholar
13. Gălbinașu, B. M., Miculescu, F., Pîrvu, D., Ciocan, L. T., Herschbach, D., Tonko, A., Pătrașcu, I. & Stoiciu, F. (2012). ‘Dental Tissue — Inlay Interface Structural Shift at Mechanical and Thermal Stresses,’ Optoelectronics and Advanced Materials 6 (3-4) 459-464.
Google Scholar
14. Hickel, R. & Manhart, J. (2001). “Longevity of Restorations in Posterior Teeth and Reasons for Failure,” The Journal of Adhesive Dentistry 3 (1) 45-64.
Publisher – Google Scholar
15. Cara, R. R., Fleming, G. J. P., Palin, W. M., Walmsley, A. D. & Burke, F. J. T. (2007). “Cuspal Deflection and Microleakage in Premolar Teeth Restored with Resin-Based Composites with and without an Intermediary Flowable Layer,” Journal of Dentistry 35(6) 482-4894.
Publisher – Google Scholar
16. Kuijs, R. H., Fennis, W. M. M., Kreulen, C. M., Roeters, F. J. M., Creugers, N. H. J. & Burgersdijk, R. C. W. (2006). “A Randomized Clinical Trial of Cusp-Replacing Resin Composite Restorations: Efficiency and Short-Term Effectiveness,” International Journal of Prosthodontics 19(4):349-54 PubMed PMID: 16900817.
Publisher – Google Scholar
17. Malhotra, N., Mala, M. & Acharya, S. (2001). “Resin-Based Composite as a Direct Esthetic Restorative Material,”Compendium of Continuing Education in Dentistry 32(5) 14-24.
Publisher – Google Scholar
18. Margeas, R. (2012). “Composite Resin: A Versatile, Multi-Purpose Restorative Material,” Compendium of Continuing Education in Dentistry 33(1) 25-27.
Publisher – Google Scholar
19. Ritter, A. V. (2001). “Posterior Resin-Based Composite Restorations – Clinical Recommendations for Optimal Success,” Journal of Esthetic and Restorative Dentistry, 13 88—99.
Publisher – Google Scholar
20. Ritter, A. V. (2008). “Posterior Composites Revisited,” Journal of Esthetic and Restorative Dentistry 20 (1) 57-67 PubMed PMID: 18237342.
Publisher – Google Scholar
21. Sarrett, D. C. (2005). “Clinical Challenges and the Relevance of Materials Testing for Posterior Composite Restorations,” Dental Materials 21(1) 9-20.
Publisher – Google Scholar
22. Technical Specifications ISO/T6 1405:2003 (E) ‘Dental Materials- Testing of Adhesion to Tooth Structure,’
23. Tezvergil, A., Fennis W. M. M., Kuijsc, R. H., Lassilab, L. V. J., Kreulen, C. M., Creugersa, N. H. J. & Vallittub P. K. (2004). “In Vitro Fracture Resistance of Fiber Reinforced Cusp-Replacing Composite Restorations,” Dental Materials 21 (5) 565-572.
24. Xu, H. H. K. et al. (2003). “Continuous-Fiber Preform Reinforcement of Dental Resin Composite Restorations,” Dental Materials, 19 (6) 523-530.
Publisher – Google Scholar