In 2008 the WHO indicated that 1.6 billion adults worldwide were overweight or obese, and that at least 300 million women were obese. Furthermore, over 40 million children under the age of five were overweight and approximately 50% of those will become childbearing women who may also become obese. Determinants of being overweight or obese were the same for all countries examined and included biological, psychological as well as sociological factors; making a multidisciplinary approach essential for a global strategy. The global increase in body weight is reflected in the UK population and in many other European countries. Currently a quarter of all women in Britain are obese (PHE, 2013). Unsurprisingly this demographic is reflected in the pregnant population (Heslehurst et al, 2007) and with increased body weight comes greater risks to health as well as a poorer long term prognosis of the offspring (Schack-Nielsen et al, 2010).
Pregnant women with a higher BMI are significantly more likely to experience adverse pregnancy outcomes (Arrowsmith et al, 2011, Denison et al, 2008, Dennison et al 2010). Obesity during pregnancy is directly associated with increased health risks for women such as gestational diabetes, hypertension, and birth complications (Scott-Pillai et al, 2013); with a subsequent need for enhanced maternity care and increased costs of care (Dennison et al 2010, Wuntakal and Hollingworth, 2009). Shorter term complications include difficulty in monitoring the fetus (Paladini, 2009) and risk of stillbirth (Scott-Pillai et al, 2013). Maternal obesity also poses increased health risks to the infant with the development of an obese phenotype (Desai and Ross, 2011), poorer newborn vascular health (Begg et al 2013) and newborns that require hospital admission (Scott-Pillai et al, 2013). Furthermore there is evidence to suggest a relationship between obesity and maternal death; the Centre for Maternal and Child Enquiries and Royal College of Obstetricians and Gynaecologists in the UK identified a higher percentage of obesity in mothers who died compared with the general maternity population.
In 2004, the WHO adopted the ‘Global Strategy on Diet, Physical Activity and Health’ to substantially reduce deaths and non-communicable disease through diet and physical activity. A key principle of the Global Strategy was to take a ‘life-course perspective’ starting with maternal health and prenatal nutrition. The WHO suggested that research evaluating policies and interventions should be promoted; and that the increased presence of behavioural science in the field should contribute to the development of both local and national expertise.
Guidelines and policies: Where are we now?
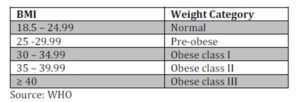
The Quality Standard for Antenatal Care in the UK (NICE 2012) states that women with a BMI ≥ 30 kg/m2, at first visit, should receive personalised healthy eating and physical activity advice from a trained professional. This advice may be delivered by dietitians for women who are class I and II obese, and further support may be provided by midwives and obstetric staff. NICE states that healthcare professionals should offer women this personalised support themselves at the first antenatal visit, unless they are insufficiently trained to do so, in which case they should refer the woman on to an appropriately trained professional.
Similarly the CMACE/RCOG (2010) report ‘Management of Women with Obesity in Pregnancy’ recommends that all obese pregnant women should be given appropriate information about the risks of obesity in pregnancy. The risks should be reduced by offering dietary and lifestyle advice. A recommendation is also made on specialist education and training for healthcare professionals in relation to managing maternal obesity and the nutrition of pregnant women. Both the NICE and CMACE/RCOG guidance highlight the vital nature of pre-pregnancy, pre-natal and post-natal dietary and lifestyle advice; both on the short and long term health of the mother as well as her child. The guidelines are targeted at providing information and advice to women, as well as healthcare professionals caring for pregnant women.
These guidelines have now been in place for over four years and there is a need to evaluate how effective the guidelines are in assisting healthcare professionals to advise obese women. It is worthwhile investigating if healthcare professionals who encounter women at their first visit are, or perceive that they are, sufficiently knowledgeable and educated to discuss these issues. Macleod et al (2013) in a survey of midwives from a range of hospital and midwifery settings, found that less than half of their respondents regularly gave advice about the risks of obesity in pregnancy and the benefit of weight management during pregnancy, yet the majority (77%) thought that such advice would be appropriate. The calculation and recording of BMI, in order to identify women who are obese at the start of their pregnancy, was found to be missed or incomplete in almost 10% of 486 maternity notes; due perhaps to a lack of facilities available to midwives at the point of booking (Rees et al 2012). Furthermore, in the UK, policy and guidance indicate that obese women should be offered referral to a dietitian. However, with such a significant proportion of the UK population with a BMI ≥ 30 kg/m2 , it is seen to be unrealistic to refer all obese, pregnant women to a dietitian.
Midwives: The forefront of maternity care
Maternal obesity has placed increasing demands on NHS maternity services, with the numbers of obese, pregnant women more than doubling since 1989 (Heslehurst et al 2007). Midwives and healthcare professionals suggest that pregnancy may be a good opportunity to enhance women’s engagement with health services, with their pregnancy providing an opportunity to address obesity (Heslehurst et al, 2013). However, healthcare professionals voiced anxieties about using maternity care as a platform for raising obesity issues, with the risk of offending or disengaging women from health services. Phelan (2010) suggested that pregnancy was a “teachable moment” because women may attach an increased value to their health, since it concerned both mother and baby. Maternity healthcare professionals also identified that further training would be required to enable them to broach and support issues of body weight and weight gain during pregnancy (Heslehurst et al 2011, 2013 ].
Midwives felt that in other health-related behaviours, training and education had an impact on confidence and motivation to raise then manage sensitive issues in their practice (Heslehurst et al, 2013). Midwives are at the forefront of maternity care in the UK, and in the vast majority of cases, are the healthcare professional that has the most frequent contact with a pregnant woman throughout her pregnancy. It could be suggested, therefore, that midwives are in an optimum position to communicate with pregnant women about body weight and weight gain during pregnancy, as well as post-birth. Midwives have expressed concern about the potential of affecting the unique relationship of trust that they had with women, and the potential to disengage women from maternity services if communication about weight and weight management was not sensitively managed (Schmied et al 2011). Singleton and Furber (2014) reported that midwives experienced a sense of helplessness about their own care provision for obese, pregnant women. Nyman et al (2011) suggested that healthcare professionals, including midwives, needed to examine their own attitudes and beliefs about obesity in order to optimise their care of obese pregnant women and offer practical and well informed guidance. In a quantitative analysis of the experiences of over 600 Australian women who gave birth during 2009, there was a relationship between women with a raised BMI and self-reported poorer treatment during pregnancy and post-natally. Furthermore, final year medical and midwifery students held less positive views of patient self-care and more negative attitudes towards pregnant women who were overweight and obese rather than healthy weight, pregnant women (Mulherin et al, 2013). Whilst it is difficult to justifiably expand the perceptions of medical students and midwifery students to the population of practicing doctors and midwives, the perception of weight stigma in maternity care expressed by pregnant women with raised BMI suggests that there is the opportunity to improve the way in which weight management in obese, pregnant women is approached.
Pregnancy can be seen as an opportunistic time to address the issue of gestational weight gain in obese, pregnant women. At this time women are given information related to other aspects of healthy lifestyle such as smoking cessation and reducing alcohol consumption and the issue of nutrition, exercise and healthy weight gain has the potential to be incorporated within the first initial consultation with the midwife. Pregnancy is often seen as a time when women will listen to and act upon the advice given by the midwife.
Dietary and physical activity interventions in a pregnant population
In 2010 a comprehensive systematic review of dietary and/or physical activity interventions for controlling weight gain in pregnancy was produced by the ScHARR Public Health Collaborating Centre (Campbell et al, 2010). Key to the development of public health guidance for promoting weight management in pregnancy; this extensive review of the literature found few studies that appraised the effectiveness of dietary and/or physical exercise intervention on gestational weight management. The studies that were included indicated inconsistent and inconclusive findings about the efficacy of dietary and/or physical activity interventions for controlling weight gain in pregnancy. An update to the review in 2011 found that there remained no significant effect of intervention on weight gain during pregnancy. Contradictory information about healthy weight management was frequently reported by women. Some interventions sought to address the issue of inconsistent information for women, nevertheless, there was no significant effect found on controlling gestational weight gain.
Evidence for the efficacy of dietary and lifestyle intervention on controlling excessive gestational weight gain was found in a randomised control trial that utilised group exercise sessions, home diet, and exercise counselling in the intervention group however obese, pregnant women were not examined as an independent subset of the intervention group. The lifestyle intervention significantly reduced the occurrences of excessive gestational weight gain (35% in the intervention group gained excessive gestational weight compared to 55% in the control group). The intervention group also reported increased daily activity, and improved diet (Hui et al, 2012). These findings suggest that utilising a lifestyle intervention of this type may contribute to managing gestational weight gain. However obese, pregnant women were not examined as an independent sub-set of the intervention group. Consequently, there is scope for examining the effect of a dietary and lifestyle intervention on an obese, pregnant population.
Another dietary and physical activity intervention reviewed normal weight and overweight/obese women in the “Fit for Delivery” study (Phelan et al 2011). This sought to control gestational weight gain so that the Institute of Medicine (IOM, 2009) guidelines were not exceeded. This was achieved in women of normal weight, but there was no significant effect on the overweight/obese women. These findings suggest that whilst the low intensity behavioural intervention was successful with normal weight women, it was deemed likely that a more intensive behavioural intervention involving a greater proportion of face-to-face contact may be necessary for overweight/obese women. Although these studies identified positive results in non-obese women, the findings cannot be generalizable to obese, pregnant women.
Psychological intervention in weight management: Raising some issues
In a systematic review exploring psychological intervention for overweight or obesity, Shaw et al (2005) examined the efficacy of behavioural and cognitive therapy strategies; both as weight loss strategies alone and in combination with diet/exercise strategies. The strategies examined included: behavioural therapies such as self-control and therapist controlled strategies, self-monitoring, problem-solving and goal-setting; cognitive behavioural therapy; psychotherapy; relaxation therapy and hypnotherapy. Shaw et al examined psychological intervention for weight loss in the general overweight and obese population. The greatest success was seen with the behavioural plus diet/exercise intervention. Such an approach including a psychological intervention could arguably apply to managing weight during pregnancy.
There are many interrelating factors that motivate eating behaviour; some tangible such as the cost and taste of foods, others less so concerning social climate, culture and the psychological determinants of food choice (European Food Information Council, 2005). Changing the dietary habits of obese, pregnant women to control gestational weight gain inevitably requires more than informational support and should include a sound psychological, theoretical framework in the design of any intervention to increase the likelihood of behavioural change. The behavioural intervention should improve clinical and psychological outcomes, but as yet research is sparse.
The ScHARR review sought to explore how contextual factors such as the beliefs of the individual or society influenced the efficacy of interventions (Campbell et al 2010). They found that dietary attitudes and behaviours before pregnancy were carried forward into pregnancy eating behaviours (Warriner 2000). Beliefs about the risks versus benefits to the fetus affected pregnancy eating behaviour (Fairburn, 1990, Wiles and Wiles, 1998). The beliefs of significant others, such as healthcare professionals, many also influence the amount of support offered to pregnant women (Heslehurst et al 2007). Whilst Campbell et al (2010) discussed evidence for contextual influence on intervention in terms of the views, attitudes and beliefs of pregnant woman and their significant others; these were not examined specifically as psychological constructs, but as descriptors of the type of influences seen in the research. Psychological outcomes of interventions are present as measures of maternal psychological wellbeing such as quality of life and self-esteem. These measurements feature as secondary maternal outcomes, yet the role of psychology in controlling gestational weight gain extends beyond just psychological wellbeing. Whilst a relationship between context and intervention success was identified the nature of how context influences outcome was not revealed.
Psychological aspects of gestational weight management are not only relevant for the design of controlled clinical trial interventions with women, but also for the design of educational interventions for midwives to facilitate the implementation of weight control advice and guidance into everyday practice. Empowering midwives in this way could potentially have paramount influence on weight management in pregnancy. There were three major barriers to the delivery of optimum support for overweight and obese pregnant women. These were the knowledge, attitudes and time constraints of healthcare professionals involved in their care (Cogswell et al, 2001). Therefore these issues need addressing directly with healthcare professionals. Since only a small number of obese, pregnant women may be referred to a dietitian or other specialist weight control intervention, changing midwives behaviour could have the greatest impact.
Strengthening intervention with psychological theory
Many of the barriers perceived by midwives to their delivery of effective support for obese pregnant women could be addressed by the development of theoretically grounded and robust controlled trial of a resource and accompanying training for midwives. There are early indications that the utilisation of psychological theory in the design and evaluation of interventions may increase the scope and quality of the research and improve clinical and psychological outcomes. Since results of interventions related to controlling gestational weight gain in obese, pregnant women so far have been inconsistent and inconclusive, future intervention should be tested in a controlled trial to strengthen and expand the evidence base. However the development of the intervention must also be grounded in a solid theoretical framework. A rigorous consultation with obese, pregnant women and healthcare professionals that are involved in their care should be conducted. This would gather the experiences of obese, pregnant women and healthcare professionals concerning controlling gestational weight gain to establish what facets an intervention should include; and identify the psychological aspects of gestational weight control such as personal perceptions, barriers, attitudes, beliefs. This would tailor the design and delivery of a resource and training package for midwives, concerning gestational weight control which is acceptable to midwives and women.
Considering a psychological model: Theory of Planned Behaviour
The Theory of Planned Behaviour (TPB) is a psychological framework that provides a perspective from which to 1) design an intervention and 2) evaluate the effects of that intervention. The TPB considers aspects of cognition within a specific population (such as what someone may believe or the influences of significant others) about a specific issue (such as weight) and provides a structure on which to base the design of an intervention. A TPB-based intervention is entirely situation and population specific and is a different approach to using therapeutic practices such as Cognitive Behavioural Therapy (CBT). Therapeutic practices such as CBT have been used in many health related settings and whilst the inclusion of some psychological therapy has been seen to strengthen interventions beyond standalone therapy, findings are inconsistent and inconclusive (Shaw et al, 2009). Therapeutic practices are fundamentally different from TPB which is a psychological theory and they perform different functions in research and design.
The TPB seeks to understand the internal cognitive processes underlying behaviour performance (Ajzen, 1985). The TPB has been successfully applied to a wide range of social and health behaviours. Examples include: the intention to attend prostrate screening services (Hevey et al, 2009); physical exercise (Nigg et al 2009) and smoking cessation (Rise, 2008). The TPB hypothesizes that the behavioural outcome is best predicted by behavioural intention. The model proposed that behavioural intention is determined by attitude to the behaviour, subjective norm (that is, perceived social influence) and perceived behavioural control over the performance of the target behaviour. For example, every day when Katy, who is in the early stages of her pregnancy and takes her lunch break at work; she purchases convenience food from the work vending machine despite holding a generalised intention to eat more healthily. According to the TPB, this might be due to three main factors. First, a belief that the outcome of this behaviour would enable her to return to her desk more quickly than if she bought a healthy salad from the shop across the road (behavioural belief and attitude). Second, Katy may in part choose the work vending machine to purchase food quickly due to perceived pressure from her line manager and others to take as short a lunch break as possible (normative beliefs and subjective norm). Finally, although Katy recognises that she could achieve her goal of eating healthily and taking a shorter lunch break by bringing her own food to work, she was unable to go to her local shop the previous evening due to other commitments with her young family (control beliefs and perceived behavioural control).
Attitude to the behaviour is formed by behavioural beliefs regarding the expected outcome of the behaviour; subjective norm by beliefs about the expectations of others and motivations to comply with these expectations; whilst perceived behavioural control is determined by control beliefs concerning the power of factors that may influence whether the behaviour happens or not. The more positive the attitude and perceived social influence plus the greater the individual’s perception of control over the behaviour, the stronger that individual’s behavioural intention should be.
Considering the above, it would therefore seem reasonable to suggest that an intervention plan should seek to address all three facets of the TPB. Thus: 1) Attitude – Change midwives’ attitudes towards the behaviour of broaching discussion about gestational weight gain with obese women by changing beliefs about the likely outcome of the behaviour. For example, create a universal path of support for obese women that assure midwives that if they broach the subject of body weight and controlling gestational weight gain, the midwifery service will be able to provide some support for obese women with controlling their gestational weight gain. 2) Subjective Norm – Address the midwives beliefs about the perceived social pressure to perform (or to not perform) a behaviour. For example, create a consistently agreed midwifery service process and ‘script’ for all midwives to follow thereby removing the individual midwife’s pressure to make a personal decision to broach the subject and how to deliver the subject matter. 3) Control Belief – Develop an increased sense of control over the behaviour in the individual. For example, by equipping midwives with some instantly accessible support materials (such as an information pack that outlines optimal weight gain during pregnancy for each of the weight categories, the benefits of controlling weight gain and information about how to eat well for pregnancy) that they may share and discuss with obese women, thereby giving midwives control over their capacity to offer tangible support.
Improving the expectations of midwives about the outcomes of any discussion on controlling gestational weight gain with obese women; improving midwives’ beliefs about what their peers think about raising such a discussion, and furthermore increasing midwives’ sense of control about their capacity to offer support may significantly increase midwives’ intention to broach this discussion. Increasing intention may in turn increase the likelihood of midwives broaching a discussion about controlling gestational weight gain with obese, pregnant women.
Conclusion
In the absence of any current, consistently efficacious intervention for controlling gestational weight gain in obese, pregnant women, a rationale is needed for developing and testing an intervention underpinned by a psychological framework. Community midwives operate at the forefront of maternity care, and are best placed to deliver advice and guidance regarding body weight during pregnancy to patients. Currently, midwives have significant reservations about how to broach discussion about, and offer support for, controlling gestational weight gain. Any intervention could be underpinned by TPB theory as applied to obesity during pregnancy, and should be developed for community midwives. To increase confidence in using the intervention, the protocol should be validated in a controlled trial. Behavioural intervention which would seek to enable community midwives to offer specific advice and support for obese, pregnant women may increase the likelihood of them offering support and advice about body weight and weight gain during pregnancy beyond their current midwifery practice.
References
1. Ajzen I. (1985) From intentions to actions: A theory of planned behaviour. In Action-Control: From Cognition to Behaviour (Kuhl J, Beckman J eds.), Springer, Heidelberg, 11-39.
2. Arrowsmith S, Wray S, Quenby S. (2011) Maternal obesity and labour complications following induction of labour in prolonged pregnancy. BJOG ; 118: 578-88.
3. Begg L, Palma-Dias R, Wang J, Chin-Dusting JFP, Skilton MR. (2013) Maternal adiposity and newborn vascular health. Arch Dis Child Fetal Neonatal Ed; 98: F279-80.
4. Campbell F, Messina J, Johnson M, Guillaume L, Madan J, Goyder E. (2010) Systematic Review of Dietary and/or Physical Activity Interventions for Weight Management in Pregnancy. Sheffield: SCHARR Public Health Collaborating Centre.
5. Centre for Maternal and Child Enquiries and Royal College of Obstetricians and Gynaecologists. (2010) CMACE/RJOG Joint Guideline: Management of Women with Obesity in Pregnancy. http://www.cmace.org.uk/getattachment/b46d45c8-330d-4b13-a408-9c630c38d152/Joint-CMACE-RCOG-Guidelines—
Management-of-Obesit.aspx
6. Cogswell ME, Perry GS, Schieve LA, Dietz WH. (2001) Obesity in women of childbearing age: Risks, prevention and treatment. Primary Care Update for Obstetricians and Gynecologists; 8: 89-105.
7. Denison FC, Price J, Graham C, Wild S, Liston WA. (2008) Maternal obesity, length of gestation, risk of postdates pregnancy and spontaneous onset of labour at term. BJOG; 115: 720—725.
8. Denison FC, Roberts KA, Barr SM, Norman JE. (2010) Obesity, pregnancy, inflammation and vascular function. Reproduction; 140: 373-385.
9. Desai M, Ross MG.(2011) Fetal programme of adipose: Effects of intrauterine growth restriction and maternal obesity/high fat diet. Semin Reprod Med; 29: 237-245.
10. European Food Information Council (2005). The Determinants of Food Choice. http://www.eufic.org/article/en/expid/review-food-choice/
11. Fairburn CG. (1990) The impact of pregnancy on eating habits and attitudes to shape and weight. Int J Eat Disord; 9: 160.
12. Heslehurst, N, Ells LJ, Simpson H, Batterham A, Wilkinson J, Summerbell CD. (2007)Trends in maternal obesity incidence rates, demographic predictors, and health inequalities in 36 821 women on a 15-year period. BJOG; 114: 187-194.
13. Heslehurst N, Moore H, Rankin J, Ells LJ, Wilkinson JR, Summberbell CD. (2011)How can maternity services be developed to effectively address maternal obesity? A qualitative study. Midwifery ; 27, e107-e177.
14. Heslehurst N, Russell S, McCormack S, Sedgewick G, Bell R, Rankin J. (2013) Midwives perspective of their training and education requirements in maternal obesity: A qualitative study. Midwifery; 29: 736-744.
15. Hevey D, Pertl M, Thomas K, Maher L, Chuinneagain SN, Craig A. (2009)The relationship between prostate cancer knowledge and beliefs and intentions to attend PSA screening among at-risk men. Patient Education and Counselling ; 74: 244-9.
16. Hui A, Back L, Ludwig S, Gardiner P, Sevenhusen G, Dean H, Sellers E, McGavock J, Morris M, Bruce S, Murray R, Shen GX. (2012) Lifestyle intervention on diet and exercise reduced excessive gestational weight gain in women under a randomised control trial. BJOG; 119: 70-77.
17. Institute of Medicine (2009). Weight Gain during Pregnancy: Re-examining the Guidelines. http://www.iom.edu/Reports/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines.aspx
18. Macleod M, Gregor A, Barnett C, Magee E, Thompson J, Anderson AS. (2013) Provision of weight management advice for obese women during pregnancy: A survey of current practice and midwives’ views on future approaches. Matern Child Nutr; 9: 467-472
19. Mulherin K, Miller KD, Barlow FK, Diedrichs PC, Thompson R. (2013) Weight stigma in maternity care: women’s experiences and care providers’ attitudes. BMC Pregnancy Childbirth, 13: 19.
20. National Institute for Health and Care Excellence (2012). NICE Quality Standard QS22: For antenatal care. http://www.nice.org.uk/guidance/index.jsp?action=byID&o=13898
21. Nigg CR, Lippke S, Maddock JE. (2009)Factorial invariance of the Theory of Planned Behaviour applied to physical activity across gender, age and ethnic group. Psychology of Sport and Exercise; 10: 219-25.
22. Nyman VMK, Prebensen AK, Flensner GEM (2011). Obese women’s experiences of encounters with midwives and physicians during pregnancy and childbirth. Midwifery; 26: 424-429.
23. Paladini D (2009). Sonography in obese and overweight pregnant women: Clinical, medicolegal and technical issues. Ultrasound Obstet Gynecol; 33: 720—729.
24. Phelan S (2010). Pregnancy: a “teachable moment” for weight control and obesity prevention. Am J Obstet Gynecol; 202: e1-8.
25. Phelan S, Phipps MG, Abrams B, Darroch F, Schaffner A, Wing RR (2011). Randomized trial of a behavioral intervention to prevent excessive gestational weight gain: the Fit for Delivery Study. Am J Clin Nutr ;93:772—9.
26. Public Health England (2013). Patterns and trends in adult obesity: Slide set. http://www.noo.org.uk/slide_sets (accessed 10/07/2013).
27. Rees GA, Porter J, Bennett S, Colleypriest O, Ellis L, Stenhouse E (2012). The validity and reliability of weight and height measurements and body mass index calculations in early pregnancy. J Hum Nutr Diet ; 25: 117-120.
28. Rise J, Kovac V, Kraft P, Moan IS (2008). Predicting the intention to quit smoking and quitting behaviour: Extending the Theory of Planned Behaviour. Br J Health Psychol; 13: 291-310.
29. Schack-Nielsen L, Michaelsen KF, Gamborg M, Mortensen EL, Sorensen TIA (2010). Gestational weight gain in relation to offspring body mass index and obesity from infancy through adulthood. Int J Obes (Lond) ; 34: 67-74.
30. Schmied VA, Duff M, Dahlen HG, Mills AE, Kolt GS (2011). Not waving but drowning: A study of the experiences and concerns of midwives and other healthcare professionals caring for obese, childbearing women. Midwifery ; 27: 424-430.
31. Scott-Pillai R, Spence D, Cardwell CR, Hunter A, Holmes VA (2013). The impact of body mass index on maternal and neonatal outcomes: a retrospective study in a UK obstetric population, 2004-2011. BJOG; 120: 932-939.
32. Shaw KA, O’Rourke P, Del Mar C, Kenardy J (2005). Psychological interventions for overweight or obesity. Cochrane Database of Systematic Reviews, issue 2. Art No.: CD003818. DOI: 10.1002/14651858.CD003818.pub2.
33. Singleton G, Furber C. (2014)The experiences of midwives when caring for obese women in labour, a qualitative study. Midwifery 30:103-111.
34. Warriner S (2000). Women’s views on being weighed during pregnancy. British Journal of Midwifery; 8: 620-623.
35. Wiles R, Wiles, R (1998). The views of women of above average weight about appropriate weight gain in pregnancy. Midwifery ; 14: 254-260.
36. World Health Organisation (2004). Global Strategy on Diet, Physical Activity and Health. www.who.int/dietphysicalactivity/strategy/…/strategy_english_web.pdf
37. World Health Organisation (2013). BMI Classification. Global Database on Body Mass Index. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html (accessed 26/06/2013).
38. Wuntakal R, Hollingworth T (2009). The implications of obesity on pregnancy. Obstetrics, Gynaecology and Reproductive Medicine; 19: 344-349.