Introduction
Historically, the energy of impact leading to these injuries was not taken into consideration,; the diagnosis and evaluation of malar fractures was considered by radiographic films sufficiently. And traditionally, Knight and North (1961), Larsen and Thomsen (1978), Kristensen and Tveterås (1986) and Zingg et al. (1992) classified the zygomatic fractures based on examination of plain radiographic films or intraoperative findings. However, regardless of the group of the classifications, Rohrich et al. (1992) and Convington et al. (1994) mentioned that 3-point fixation with steel wire is performed in almost all cases of zygomatic fractures.
Recently, plate fixation has increased in popularity for the treatment of zygomatic fractures. Rohrich and Watumull (1995) and Zachariades et al. (1998) mentioned that fixation with mini or micro plates provides better rigidity and stability than wiring of fragments. Furthermore, advances in radiological techniques have led to the increased use of high-resolution computed tomography (CT) and 3-dimentional (3D) CT, which can be used to diagnose even a tiny fracture or slight gap. Furthermore, improved safety procedures had led to a reduction in the number of accidents leading to these severe deformities. However, patients demand esthetic improvement, even when they have only a slight gap, and an increasing number of cases of zygomatic fracture are being repaired surgically.
The researchers consider the previous classification system should be improved. In this study, the researchers describe a new means of classifying zygomatic fractures based on 3D-CT and the type of trauma inflicted, which could be used to inform surgical strategy.
Materials and Methods
Patients treated for isolated zygomatic fractures at the Keio Univeristy Hospital between 2004 and 2011 were recruited for this study. Any patient who did not undergo a preoperative CT scan with 0.625 mm was excluded from this study. Patients with only zygomatic arch fracture or multiple complex fractures were also excluded.
This study was approved by the Institutional Review Board of Keio University School of Medicine, and the medical protocol and ethical guidelines followed the tenets of the Declaration of Helsinki.
The zygoma is supported by the following 4 regions: the zygomaticofrontal suture (ZF), inferior orbital rim (IO), zygomaticomaxillary buttress and zygomaticotemporal suture. When the zygoma undergoes an impact, the location of the resulting fracture depends on which of these supporting regions collapse. The collapse of these regions is dependent on the direction of the impact, but in general, the most structurally impaired of these regions will collapse first. The most stabile region of the zygoma is the ZF. In fact, the ZF comprises thickened cortical bone, and is triangular in shape. Collapse of the ZF requires a strong external force. Therefore, the researchers analyzed and classified the external forces based on the deviation of the zygoma featuring ZF.
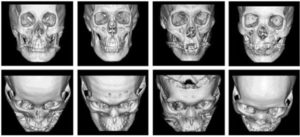
The researchers focused on the classification of the ZF and IO based on preoperative 3D-CT. The ZF was divided into 2 types: “shear type” which indicates the presence of a gap or deviation of the ZF, whereas the “greenstick type” indicates the absence of a gap or deviation of the ZF. Analysis of the IO is performed according to whether the zygoma is rotated on the maxilla, or below the maxilla, and is classified as “lateral type” and “medial type”, respectively (Figure 1).
Figure 1. The Type of the Malar Fracture Based on ZF and IO.

Results
In total, the researchers performed 176 operations for facial fracture. After applying the exclusion criteria, this study population included 113 patients aged 16 to 82 years (mean (SD) age = 39.8 (17.0) years), including 74 men and 39 women.
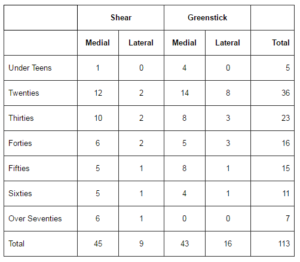
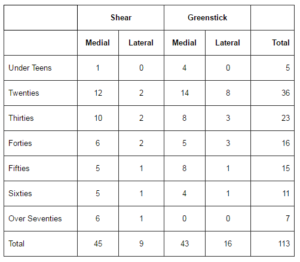
The total numbers of patients in each group and age range are shown in Table 1. Overall, 54 patients had shear type and 59 patients had greenstick type ZF. In the shear type and greenstick type groups, the incidence of medial type was significantly greater than that of lateral type (p < 0.001). The researchers classified patient ages as follows: 50. The ratio of shear type was 0.36, 0.56 and 0.54, respectively (p < 0.05).
Table 1. Classification of Each Groups and Generations
Discussion
The most widely used approach for classifying fractures is the Knight and North classification system. Knight and North (1961) classified fractures into 6 groups and 4 subdivisions based on plain radiographic films. The system allows for easy evaluation and is clinically useful, but cannot be used to evaluate bone displacement in 3-dimensions. This is particularly a problem for isolated zygomatic fractures since it is thought that the displacement of zygomatic bone might be a consequence of axial rotation around a vertical.
More recently, Zingg et al. (1992) have used CT scans to aid classification, which allow for detailed 3D evaluation. However, this increases the number of groups and subdivisions to be classified, making clinical use more complicated. Therefore, the researchers sought to establish a simple, usable classification system for different types of zygomatic fractures based on the findings of 3D-CT scans. Today, high-resolution CT can be performed easily and quickly with low exposure times. 3D-CT can be reconstructed easily from the data. However, there are few reports that have used 3D-CT to classify zygomatic fractures.
Previously, Manson et al. (1990) classified zygomatic fractures into fractures caused by low-energy, medium-energy and high-energy injuries. Low-energy fractures were found to result in minimal or no displacement, and had a continuous ZF. Medium or high-energy injuries resulted in fractures of all buttresses, including the ZF. In such case, the researchers used the condition of the ZF to inform this paper’s classification system and report that greenstick or shear type fractures are based on the energy of injury.
Rohrich and Watumull (1995) and Rinehart et al. (1989) reported that rigid miniplate fixation provides consistently better zygomatic and global symmetry than interosseous wires, and deforming forces of this magnitude require at least 2 miniplates. Therefore, many surgeons use 3 areas of internal fixation to provide rigidity and satisfactory zygomatic contour and eminence. However, dissection of the periosteum for plate fixation impairs the blood supply to the zygoma. This in turn leads to long-term complications such as bone absorption or infection. Given these complications, Nagasao et al. (2007) mentioned that the provision of adequate stability with minimal handling is preferable.
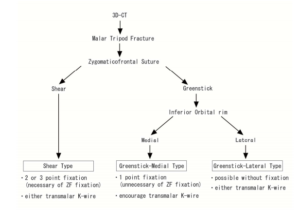
Dal Santo et al. (1992), Ellis and Kittindumkerng (1996), Manson et al. (1990), Nagasao et al. (2009) and Tarabichi (1994) mentioned that the potential risk of postoperative setbacks increases when the ZF is sheared regardless of medial or lateral rotation, and proper fixation of the miniplate is particularly important in these instances. Medial and lateral rotation is based on the direction of energy associated with the injury. However, when the ZF is not sheared, but only made greenstick, medial rotation carries a higher risk of postoperative setback than the lateral. Therefore, insertion of a plate at the ZM or IO is required. If stability is a concern, a transzygomatic Kirschner wire (K-wire) can be added. Treatment of lateral rotation simply requires rotation with or without transzygomatic Kirschner wire.
Based on the findings of 3D-CT, energy of injury and treatment method, the researchers classified zygomatic fractures into 3 types. First, they classified the ZF status into either shear or greenstick types. The shear type is a high-energy injury, regardless of medial or lateral rotation at the IO, and requires at least 2-point fixation involving the ZF. For the greenstick type, further analysis is performed at the IO and this type is further divided into medial and lateral types (Figure 2). The greenstick-medial type has a risk of postoperative setback, so 1 plate at ZM or IO is required. And the greenstick-lateral type is usually performed only reduction without plating.
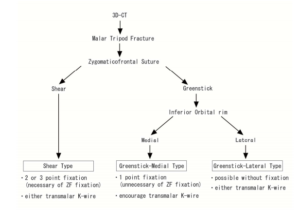
Figure 2. The Study’s Classification Protocol and Guideline for Treatment
In this study, the researchers did not consider other postoperative setbacks other than bone displacement. In clinical practice, it is necessary to consider every possible factor, such as postoperative setback, gender, age, duration between injury and operation, extent of scar associated with soft tissue and blood supply available during the dissection of the periosteum. However, the researchers believe that in the majority of cases treated according to the present classification system, there can be achieved sufficient stability for the fractured zygoma to be maintained at the correct position following repositioning.
Conclusions
The researchers’ classification system based on 3D-CT featuring ZF is a great improvement to the current classification system based on the mechanism of facial injury. The system may be used to inform clinicians about the ideal fixation strategy conducive to biomechanical stability. This classification system is a very useful and easy tool for the classification of zygomatic fractures and may serve to improve surgical outcomes in patients.
References
Covington, D. S., Wainwright, D. J., Teichgraeber, J. F. & Parks, D. H. (1994). “Changing Patterns in the Epidemiology and Treatment of Zygoma Fractures: 10-Year Review,” J Trauma, 37 (2) 243-248.
Publisher – Google Scholar – British Library Direct
Dal Santo, F., Ellis, E. & Throckmorton, G. S. (1992). “The Effects of Zygomatic Complex Fracture on Masseteric Force,” J Oral Maxillofac Surg, 50 (8) 791-799.
Publisher – Google Scholar
Ellis, E. & Kittidumkerng, W. (1996). “Analysis of Treatment for Isolated Zygomaticomaxillary Complex Fractures,” J Oral Maxillofac Surg, 54 (4) 386-400.
Publisher – Google Scholar – British Library Direct
Knight, J. S. & North, J. F. (1961). “The Classification of Malar Fracture: An Analysis of Displacement as a Guide to Treatment,” Br J Plast Surg, 13 325-339.
Publisher – Google Scholar
Kristensen, S. & Tveterås, K. (1986). “Zygomatic Fractures: Classification and Complications,” Clin Otolaryngol Allied Sci, 11 (3)123-129.
Publisher – Google Scholar
Larsen, O. D. & Thomsen, M. (1978). “Zygomatic Fracture: A Simplified Classification for Practical Use,” Scand J Plast Reconstr Surg, 12 (1) 55-58.
Publisher – Google Scholar
Manson, P. N., Markowitz, B., Mirvis, S., Dunham, M. & Yaremchuk, M. (1990). “Toward CT-Based Facial Fracture Treatment,” Plast Reconstr Surg, 85 (2) 202-212.
Publisher – Google Scholar
Nagasao, M., Nagasao, T., Imanishi, Y., Tomita, T., Tamaki, T. & Ogawa, K. (2009). “Experimental Evaluation of Relapse-Risks in Operated Zygoma Fractures,” Auris Nasus Larynx, 36 (2) 168-175.
Publisher – Google Scholar
Nagasao, T., Tamada, I., Miyamoto, J., Ogata, H., Kaneko, T., Nagasao, M. & Nakajima, T. (2007). “Effectiveness of Additional Transmalar Kirschner Wire Fixation for a Zygoma Fracture,” Plast Reconstr Surg 119 (3) 1010-1019.
Publisher – Google Scholar – British Library Direct
Rinehart, G. C., Marsh, J. L., Hemmer, K. M. & Bresina, S. (1989). “Internal Fixation of Malar Fractures: An Experimental Biophysical Study,” Plast Reconstr Surg, 84 (1) 21-25.
Publisher – Google Scholar
Rohrich, R. J., Hollier, L. H. & Watumull, D. (1992). “Optimizing the Management of Orbitozygomatic Fractures,” Clin Plast Surg, 19 (1) 149-165.
Publisher – Google Scholar
Rohrich, R. J. & Watumull, D. (1995). “Comparison of Rigid Plate Versus Wire Fixation in the Management of Zygoma Fractures: A Long-Term Follow-Up Clinical Study,” Plast Reconstr Surg, 96 (3) 570-575.
Publisher – Google Scholar – British Library Direct
Rowe, N. L. & Killey, H. C. (1968). ‘Fractures of the Facial Skeleton, 2nd ed.,’ E&S. Livingstone, Edinburgh and London
Google Scholar
Tarabichi, M. (1994). “Transsinus Reduction and One-Point Fixation of Malar Fractures,” Arch Otolarngol Head Neck Surg, 120 (6) 620-625.
Publisher – Google Scholar – British Library Direct
Zachariades, N., Mezitis, M. & Anagnostopoulos, D. (1998). “Changing Trends in the Treatment of Zygomaticomaxillary Complex Fractures: A 12-Year Evaluation of Methods Used,” J Oral Maxillofac Surg, 56 (10)1152-1156.
Publisher – Google Scholar – British Library Direct
Zingg, M., Laedrach, K., Chen, J., Chowdhury, K., Vuillemin, T., Sutter, F. & Raveh, J. (1992). “Classification and Treatment of Zygomatic Fractures: A Review of 1,025 Cases,” J Oral Maxillofac Surg, 50 (8) 778-790.
Publisher – Google Scholar