Discussion
Despite several flaps introduced for hand reconstruction, the reversed radial forearm flap is still largely preferred for hand reconstruction [9]. It is considered a workhorse flap in hand reconstruction [10]. It offers many merits such as adequately large, thin and pliable and colour matched tissues. It offers a simple and effective one-stage method of soft tissue reconstruction. Surgery is confined to a single site and limb permitting early mobilization and rehabilitation. Moreover, vascularized bone and tendon transfer, along with the flap, are possible. If the flap pedicle was designed with proper length, it could also cover the fingers [11-15].
On the other hand, the radial forearm flap that has many disadvantages has been reported such as poor donor sit skin graft take, noticeable donor scar, bulky volar skin compared to thin dorsal skin, , hand swelling, reduced joint movement and strength, reduced sensation, cold- intolerance, and radius fracture[16] [17]. Moreover, acute ischemia of the hand has been reported in spite of adequate circulation by preoperative Allen’s test [18]. In a review for the clinical trials to reduce donor site morbidity, Loeffelbein et al [19] concluded that, most publications failed to provide the solid evidence characteristic of high-quality research.
The reversed flow posterior interosseous artery flap (PIA) is a valuable option for reconstruction of hand defects. As it is based on the anterior-posterior interosseous artery system, it avoids sacrifice of either the radial or ulnar arteries as in case of the radial or ulnar forearm flaps. It is also possible to use this flap in circumstances where there has been damage to the palmer arch. In addition, the dorsal forearm skin is less bulky than the volar forearm skin; therefore, the PIA flap has better contour match. Furthermore, the donor site can often be closed primarily if the defect is small or by a skin graft, that will take well on the muscle bellies of the extensor carpi ulnaris and extensor digiti minimi [3]. Also in the event of flap failure, the PIA flap can be debrided and the defect skin grafted, while all other flap options remain available. This relative expendability of the PIA flap is one of its unique qualities [20]. Lastly, the flap can also be raised with a segment of the proximal third of the ulna as an osteocutaneous flap for bone defects, including thumb reconstruction [21].
In this study, 25 PIA flaps were harvested to close the ulnar side defects of the hand. The flap survival rates were comparable to other reported studies [22, 23] which supports its safety. Our results also showed a similar range of complications [23-28].
The flap can be considered as a smart and reliable option for coverage of the ulnar side of the hand, as it doesn’t sacrifice the main arteries of the forearm and hand. It is a single stage procedure with no need for 2nd stage division. It doesn’t need special equipments or special training like microsurgical transfer.
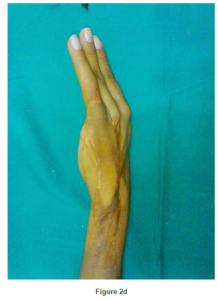
The flap was harvested with a skin bridge over the pedicle changing the island flap into a racquet shaped flap as described in a previous work [8]. The racquet shape modification of the flap avoids compression of the vascular pedicle which can develop in case of tunneling under skin or skin direct closure. In addition, it allows easy flap inset, enhances venous drainage as this skin bridge contains additional subcutaneous venous plexus. The skin strip can be also used for solving any additional local skin problems.
Although the radial forearm flap has higher success rates than PIA flap, and has been considered the workhorse flap for hand reconstruction; it seems less satisfactory compared to PIA flap especially for ulnar side hand defects. The PIA flap seems to be a reliable option for reconstructing the ulnar side of the hand. We feel that the PIA must be considered as one of the new preferred valuable flaps for hand reconstruction. This flap must be learned well to both senior and junior staff and should be considered as another option for hand coverage when the surgeon prefers not to use free tissue transfer or the radial artery flap. Gentle pedicle dissection and avoidance of pedicle compression using the racquet shape design reduce flap necrosis. During flap elevation, we could harvest a skin paddle up to only 3-4 cm below the lateral epicondyle of the humerus that enabled us to cover defects down to the middle phalanges. In addition, anastomotic vessel dissection as described by Bayon and Pho 4 also increases flap arc of rotation. In the last decade, the senior author (Ayman shaker) as well as the other authors used the posterior interosseous flap in more than 80 cases of hand and upper limb reconstruction and they believe that the PIAF can be used efficiently to solve many problematic defects.
Conclusion
The PIA flap seems a smart and reliable option for coverage of the ulnar side of the hand. Further evidence- base has shown that the PIA flap should be considered as a reliable choice in hand reconstruction especially ulnar side defects. The flap should be learned to senior and junior reconstructive surgeons as a classical flap for hand reconstruction. Familiarity with the flap anatomy lessens the operative time greatly and makes surgical dissection easier.
References
1. Lu, L. J., Wang, S. F., Yang, J. et al. (1986). ‘The Posterior Interosseus Flap: A Report of 6 Cases,’ The Second Symposium of the Chinese Association of Hand Surgery (Qing Dao city); 187e91.
Google Scholar
2. Penteado, C. V., Masquelet, A. C. & Chevrel, J. P. (1986). ‘The Anatomic Basis of the Fasciocutaneous Flap of the Posterior Interosseus Artery,’ Surg Radiol Anat; 8: 209e15.
3. Zancolli, E. A. & Angrigiani, C. (1988). “Posterior Interosseous Island Forearm Flap,” Journal of Hand Surgery: British & European Volume; 13-B: 130e5.
Publisher – Google Scholar
4. Bayon, P. & Pho, R. W. H. (1988). “Anatomical Basis of Forearm Flap Based on Posterior Interosseus Vessels,”Journal of Hand Surgery 13B: 435.
Publisher – Google Scholar
5. Giunta, R. E. & Lukas, B. (1998). “Impossible Harvest of the Posterior Interosseus Artery Flap: A Report of an Individualised Salvage Procedure,” British Journal of Plastic Surgery 51: 642-645.
Publisher – Google Scholar
6. Costa, H. & Soutar, D. S. (1988). “The Distally Based Island Posterior Interosseus Flap,” British Journal of Plastic Surgery 41: 221-217.
Publisher – Google Scholar
7- Brunelli, F., Giele, H. & Perrotta, R. (2000). “Reverse Posterior Interosseus Flap Based on an Exteriorized Pedicle to Cover Digital Skin Defects,” Journal of Hand Surgery British; 25: 296—9.
Publisher – Google Scholar
8. Nasser, S., Abdallah, Y. & Shaker, A. A. 2011). “Racquet-Shaped Modification of the Island Pedicle Flaps: A Simple Design to Increase its Versatility and to Decrease the Complication Rate, Egypt,” Egyptian Journal of Plastic and Reconstructive Surgery, Vol. 35, No. 1, January: 31-40.
Publisher – Google Scholar
9. Megerle, K., Sauerbier, M. & Germann, G. (2010). “The Evolution of the Pedicled Radial Forearm Flap,” Hand; 5(1): 37-42.
Publisher – Google Scholar
10. Friedrich, J. B. & Pederson, W. C., Bishop, A. T., Galaviz, P. & Chang, J. (2012). “New Workhorse Flaps in Hand Reconstruction,” Hand 7:45—54.
Publisher – Google Scholar
11. Soutar, D. S. & Tanner, N. S. B. (1984). “The Radial Forearm Flap in the Management of Soft Tissue Injuries of the Hand,” British Journal of Plastic Surgery, Volume 37, Issue 1, 18—26.
Publisher – Google Scholar
12. Jones, N. F., Jarrahy, R. & Kaufman, M. R. (2008). “Pedicled and Free Radial Forearm Flaps for Reconstruction of the Elbow, Wrist, and Hand,” Plastic & Reconstructive Surgery; 121(3): 887-98.
Publisher – Google Scholar
13. Taghinia, A. H., Carty, M. & Upton, J. (2010). “Fascial Flaps for Hand Reconstruction,” Journal of Hand Surgery; 35(8): 1351-5.
Publisher – Google Scholar
14. Kim, K. S., Kim, E. S., Hwang, J. H. & Lee, S. Y. (2010). “Thumb Reconstruction Using the Radial Midpalmar (Perforator Based) Island Flap (Distal Thenar Perforator-Based Island Flap),” Plastic & Reconstructive Surgery; 125(2): 601-8.
Publisher – Google Scholar
15. El-Khatib, H. A. & Hammouda, A. H. (2005). “Reverse Osseofasciocutaneous Radial Forearm Flap for Thumb Reconstruction: A Flap Design and Case Series,” Journal of Hand Surgery; 30(6): 1298-304.
Publisher – Google Scholar
16. Page, R. & Chang, J. (2006). “Reconstruction of Hand Soft-Tissue Defects: Alternatives to the Radial Forearm Fasciocutaneous Flap,” Journal of Hand Surgery, 31(5): 847—56.
Publisher – Google Scholar
17. Timmons, M. J., Missotten, F. E. M., Poole, M. D. & Davies, D. M. (1986). “Complications of Radial Forearm Flap Donor Sites,” British Journal of Plastic Surgery, Volume 39, Issue 2: 176—178.
Publisher – Google Scholar
18. Jones, B. M. & O’Brien, C. J. (1985). “Acute Ischaemia of the Hand Resulting from Elevation of a Radial Forearm Flap,” British Journal of Plastic Surgery, Volume 38, Issue 3: 396—397.
Publisher – Google Scholar
19. Loeffelbein, D. J., Al-Benna, S. et al. (2012). “Reduction of Donor Site Morbidity of Free Radial Forearm Flaps: What Level of Evidence Is Available?,” Eplasty; 12: e9.
Publisher – Google Scholar
20. Costa, H., Pinto, A. & Zenha, H. (2007). ‘The Posterior Interosseus Flap e a Prime Technique in Hand Reconstruction,’ The Experience of 100 Anatomical Dissections and 102 Clinical Cases; PRS March.
21. Hsu, C. & Chang, J. (2003). “The Posterior Interosseus Artery Flap Revisited,” Operative Techniques in Plastic and Reconstructive Surgery, Vol 9, No 4: p 173-180.
Publisher
22. Fujiwara, M., Kawakatsu, M., Yoshida, Y. & Sumiya, A. (2003). “Modified Posterior Interosseus Flap in Hand Reconstruction,” Techniques in Hand and Upper Extremity Surgery, 7 (3): 102-109.
Publisher – Google Scholar
23. Balakrishnan, G., Kumar, B. S. & Hussein, S. A. (2003). “Reverse Flow Posterior Interosseus Artery Flap Revisited,”Plastic & Reconstructive Surgery, 111 (7): 2364-2369.
Publisher – Google Scholar
24. Shibata, M., Iwabuchi, Y., Kubota, S. et al. (1997). “Comparison of Free and Reversed Pedicled Posterior Interosseus Flap,” Plastic & Reconstructive Surgery, 99: 791-802.
Publisher – Google Scholar
25. Buchler, U. & Frey, H.- P. (1991). “Retrograde Posterior Interosseus Flap,” Journal of Hand Surgery [Am.], 16A: 283-292.
Publisher – Google Scholar
26. Dap, F., Dautel, G., Voche, P. et al. (1993). “The Posterior Interosseus Flap in Primary Repair of Hand Injuries,”Journal of Hand Surgery. (Br.), 18 (4): 437-45.
Publisher – Google Scholar
27. Brunelli, F., Valenti, P., Dumonitier, C. et al. (2001). “The Posterior Interosseus Reverse Flap: Experience with 113 Flaps,” Annals of Plastic Surgery, 47: 25-30.
Publisher – Google Scholar
28. Koch, H., Kursumovic, A., Hubmer, M. et al. (2003). “Defects on the Dorsum of the Hand – The Posterior Interosseus Flap and its Alternatives,” Journal of Hand Surgery, 8: 205-12.
Publisher – Google Scholar