Introduction
As defined in GOLD 2014 by Vestbo et al (2014), which is an update of GOLD 2001 by Pauwels et al (2001), chronic obstructive pulmonary disease (COPD) is a common preventable and treatable disease characterized by airflow limitation that is usually progressive and is also associated with an enhanced chronic inflammatory response in the airways and the lung to noxious particles or gases. According to the joint guidelines by Celli et al (2004) on behalf of the American Thoracic Society and the European Respiratory Society (ATS-ERS), COPD is characterized by airflow limitation that is not fully reversible. Indeed, according to the WHO (2012), it is one of the fastest growing diseases in the world, affecting the lives of 210 million people and contributing to 5% of deaths globally. Fletcher et al (1976) and Antó et al (2001) both reported the disease as often left undiagnosed for many years, particularly in its early stages. Its progression has been described by Mannino and Kiri (2006) as varying by phenotype- a concept that remains poorly understood. According to NICE (2010), evidence suggests an estimated three million people are affected by COPD in the UK with only about 900,000 having been diagnosed.
COPD exacerbation is a major cause of hospitalization. According to a report by LAIA: the Lung and Asthma Information Agency (2001), figures for the period 1995-2004 in the UK indicate a 50% increase in COPD exacerbations- responsible for many emergency hospital admissions over the period. The WHO (2004) reported the disease as accounting for over 108,000 emergency admissions in, for example, the financial year 2004/2005 and projected that it would rise to almost 160,000 admissions by 2028- costing an estimated £376 million annually. Indeed, the importance of COPD to the UK public health is highlighted by its inclusion among the nine target health conditions for which there have been since 2005, National Service Frameworks (NSFs) and strategies for qualitative care by the Department of Health (2005).
Although occupational exposure to dusts and chemicals as well as the genetic disorder known as alpha-1-antitrypsin deficiency are known to increase the risk of COPD, GOLD 2001 by Pauwels et al (2001) have identified cigarette smoking as by far the most important risk factor for the disease. According to the National Heart, Lung and Blood Institute (2012), there is also emerging evidence a patient can develop COPD if they live with a smoker or breathe in second-hand smoke routinely elsewhere. In general, according to reports by the American Thoracic Society (1995), Pauwels et al (2001) in GOLD 2001 and Vestbo et al (2014) in GOLD 2014, apart from the harm caused by exposure to tobacco smoke, such COPD patients will lose lung function more quickly than those who are not exposed as the smoke destroys the tiny hair-like cilia that normally repair and clean the airways. According to the WHO (2014), regular exposure to second-hand smoke can increase a person’s risk of heart disease and lung cancer by as much as a third as well as make it more likely to develop COPD. Indeed, studies by Dayal et al (1994), Leuenberger et al (1994), Berglund et al (1999) and Larsson et al (2003)- to list but four, suggest there is mounting evidence COPD might be independently associated with passive smoking. Other reports by the U.S. Department of Health and Human Services (2006), Eisner (2009) and Jordan et al (2011) also suggested second hand smoking might be associated with poorer health status and a greater risk of COPD exacerbation. According to NICE (2010), COPD exacerbation is a major driver of emergency admissions for COPD in the UK. Indeed, Jordan et al (2001) and Mannino and Buist (2007) have separately suggested passive smoking as strongly implicated in the etiology of COPD. A study by the UK Royal College of Physicians (2005) and another by Sims et al (2010) both reported smoke exposure levels as having been declining since the mid-1990s in England such that the levels among non-smoking adults living with non-smoking partners in 2003 were about half the levels in 1993.
Since July 2007, there has been smoking ban in England at enclosed places of work as well as enclosed places which are open to the public, such as where goods and services can be obtained, including private clubs and certain other designated places as described in chapter one of the Health Act of 2006, the details of which can be found in the National Archives (2006). The term “smoking ban” was used interchangeably with smoke-free legislation in this study.The ban in England followed from similar bans introduced earlier in Scotland (March 2006), Wales and Northern Ireland (April 2007) and amidst evidence about the benefits of such bans to the health of the population, especially with regard to the risk of myocardial infarction (MI) as reported by Bartecchi et al (2006) and Khuder et al (2007). However, to date the benefits of the smoking ban legislation specifically for COPD have not been investigated yet. It is reasonable to expect the smoking legislation to offer similar benefits to COPD patients in terms of reductions in emergency admissions.
In terms of risks associated with exposure to passive smoking, the impact on COPD (especially its exacerbation) is widely recognized and according to Eisner (2009) , Mannino and Buist (2007) and Eisner et al (2009), COPD patients are likely to benefit the most from declining exposure to passive as well as active smoking than those without COPD. Two recent UK studies by Sims et al (2010) and Mackay et al (2010)- both of which are based on routinely collected hospital admission data have reported benefits of the ban in the form of reductions in emergency admission rates for MI in England and asthma in Scotland respectively. It was thus reasonable to assess whether similar benefits could be found for COPD using the same database. We know from Holguin et al (2005), Anecchino et al (2007) and Boutin-Forzano et al (2007) that the overwhelming majority of COPD patients also suffer from other diseases as comorbidities are associated with a number of the poorer outcomes experienced by these patients. Actually, the most common of these comorbidities include hypertension, heart failure and coronary artery disease- all of which are known to be strongly associated with the risk of MI. Indeed, with about 40% of COPD patients having heart disease as reported by Anecchino et al (2007) and between 17%-42% of them also living with high blood pressure as reported by Boutin-Forzano et al (2007).
The aim of this study was to assess whether there was any significant change in the annual number of emergency admissions for COPD among persons aged 40 and older following the implementation of the smoke-free legislation in England.
Methods
Data
The National Health Service (NHS) in England routinely collects information in the form of Hospital Episode Statistics (HES) on all patients who receive care in its hospitals. The HES data are freely available online from the website of the Health and Social Care Information Centre, UK (2013; http://www.hscic.gov.uk/) and the annual national aggregated data for COPD (classified in HES as ICD-10 J43-J44) for the financial years 2002/03 to 2011/2012 were used. In accordance with the suggestion by Zwar et al (2011), persons younger than 40 years were excluded to minimize the possible impact of misdiagnosis of the disease. Only data on all emergency admissions are freely available with age and sex breakdown.Therefore, for each year and sex, the age distribution of finished consultant episodes for COPD were used as weights on the corresponding age distribution of all emergency admissions to derive modified weights to apply on the corresponding data for the total emergency admissions for COPD to obtain the study data.
Corresponding mid-year population estimates were obtained from the Office for National Statistics (ONS), UK (2012). The chosen period represented the last five years prior to implementation of the smoking ban legislation (i.e. 2002/03 to 2006/07 as 2002-2006) and afterwards (i.e. 2007/08 to 2011/12 as 2007-2011). The annual data on cigarette smoking prevalence for the UK were similarly obtained from the ONS and were used to adjust for the direct effect of smoking in the trend analyses. To estimate the annual admission rates, the mid-year population estimates were considered as the corresponding patients at risk of emergency admission for COPD- a common practice for the analysis of aggregated data as described by Esteve et al (1994).
Statistical Analysis
Poisson regression model was used to test the hypothesis that there was no change in the annual number of emergency admissions for COPD between the five-year periods before and after the ban. The annual number of admissions for COPD was thus assumed to come from a Poisson distribution with each admission considered as having occurred independently at random and at a constant rate as described by McCullagh and Nelder (1989) and as illustrated by Agresti (2002). The impact of the smoking ban was assessed in terms of percentage change in emergency admission rates for COPD between the two periods- calculated as the exponent of the estimated incident reporting ratio (IRR) with the corresponding 95% confidence interval (CI). Thus, in common with Sims et al (2010), the model included the introduction of the smoking ban as a binary predictor variable (= 1 for the ban period 2007-2011 and =0 for the period 2002-2006), sex, age and the annual smoking prevalence. To avoid any assumption on the form of relationship between annual smoking prevalence and the outcome, the variable was log-transformed in preference over categorization. The annual mid-year population estimate for England was used as an offset variable so as to facilitate a one-to-one relationship between the population size and the number of admissions. Stratified analyses by sex were also conducted to assess the impact of the legislation in men and women separately.
In common with most ecological analyses, over-dispersion was anticipated as a likely problem and was assessed by testing for the significance of the deviance goodness of fit of the model, and the estimated standard errors were adjusted for its effect as described and illustrated by Cook and Weisberg (1982). The deviance (likelihood ratio) test statistic G² was used to assess the goodness-of-fit of the model.
All analyses were done using the statistical software package StatsDirect version 2.8.040.
Sensitivity Analysis
To assess whether emergency admission rates for COPD had been declining over time independently of the smoking ban, sensitivity analysis was conducted by refitting the final model separately with assumed false starting year of 2004 (i.e. three years prior to the actual) in one analysis and 2009 (i.e. two years after) in another.
Two additional sensitivity analyses were conducted: (1) the Poisson regression methodology was applied to the HES data for myocardial infarction (MI) among persons aged 20 and older to replicate the findings of the earlier study by Sims et al (2010) which was based on a similar age group and (2) the association between the introduction of the smoking ban was investigated in relation to fractures of skull and facial bones among persons aged 40 and older which was a prioriassumed to have no direct causal link to the smoking ban.
Results
The age distribution of all emergency admissions in HES did not vary significantly from year to year according to the data for the financial years 2007/08 to 2011/12 as shown in Table 1- suggesting the assumption of a consistent age distribution over the ten-year study period was appropriate. The same was true for the age distribution of finished consultant episodes for COPD.
There were 1,026,782 emergency admissions for COPD between 2002 and 2011 which indicated a steady pattern of annual decline among men and women that started in 2005 and continued to the year of implementation of the smoking ban (Figure 1). Although the annual number of emergency admissions for COPD was consistently higher in men, the sex gap had been on the decline since the implementation of the smoking ban. In the five-year period prior to the ban, there were 256,340 emergency admissions for COPD among men compared with 244,257 and women. By contrast, the corresponding numbers in the ban period were 260,997 among men compared with 265188 among women- indicating more admissions occurred in women.
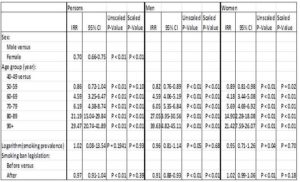
COPD emergency admissions were 2.5% lower in the ban period compared to the period before the ban although this was not statistically significant (P=0.39). Emergency admission levels were about 30% lower in women when compared with the level in men (P< 0.0001) (Table 1).
Table 1: Estimated Incident Reporting Ratio (IRR) for COPD Emergency Admissions
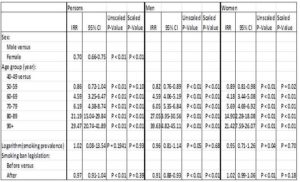
Stratified Analyses by Sex
Stratified analyses showed that in men the number of emergency admissions for COPD declined significantly by 9.4% (95% CI: 6.5% – 12.3%; P< 0.0001) during the period of the smoking-ban compared to the similar period prior to the ban. By contrast, in women emergency admissions were 2% higher in the ban period although this was not statistically significant (P< 0.1838). This implies that with respect to COPD emergency emissions, the introduction of the smoking ban has had a more pronounced effect in men than in women.
Sensitivity Analysis in COPD
In the sensitivity analysis involving 2004 as the starting year of the implementation of the smoking ban on the data for men, there was no evidence of a smoking-ban effect. Instead, there was a non-significant increase of 0.7% (P=0.85) in the number of emergency admissions for COPD in the ban period when compared with the period prior to 2004. When 2009 was assumed as the starting year of the smoking ban, the number of emergency admissions for COPD in the ban period having declined by 8.5% (95% CI: 5.8% – 11.1%; P< 0.0001) when compared with the period prior to 2009.
Sensitivity Analysis in Myocardial Infarction
There were 556,023 emergency admissions for myocardial infarction (MI) among persons aged 20 and older during the study period. There was evidence of decline in the number of emergency admissions for MI in the ban period when compared with the period prior to the ban by about 19.3% (95% CI: 13.8% – 24.5%; P< 0.0001).
Sensitivity Analysis in Fracture of Skull and facial Bones
There were 138,876 emergency admissions for fracture of skull and facial bones among persons aged 40 and older during the study period. Emergency admissions for fracture of skull and facial bones remained largely unchanged in the study period- the numbers in the ban period indicating a non-significant increase of 1.6% (P= 0.5342) when compared with the period prior to the ban.
Discussions
This study aimed to assess the impact of the smoke-free legislation since its introduction on emergency hospital admissions among patients with COPD in England as at the end of the financial year 2011/12. The Hospital Episodes Statistics (HES) data which were freely available were used to compare the emergency admission rates for COPDbetween the five-year periods before and after the ban- thus adopting a similar approach to the two earlier HES-based UK studies by Sims et al (2010) and Mackay et al (2010).
The results indicate that the frequency of emergency hospital admissions for COPD had dropped significantly only in men in the five-year period 2007-2011 of the smoking ban legislation when compared with the corresponding five-year period 2002-2006 in England. In men, emergency hospital admissions for COPD declined by about 9% in the smoking ban period where as, levels increased by a non-significant 2% in women. These results indicate a narrowing of the sex gap. Indeed, whereas the total number of emergency admissions for COPD in the five-year period prior to the ban was higher in men (256,340 in men compared with 244,257 in women), the total for the succeeding five-year period was higher among women (260,997 in men compared with 265,188 in women), although the annual rates remained higher among men.
Evidence of similar sex difference in the impact of the smoking ban has been reported for myocardial infarction by Cesaroni et al (2008), Vasselli et al (2008) and Sims et al (2010). According to Wardle and Mindell (2008), the reduction in women might be more gradual because exposure to second-hand smoking had declined many years earlier than the legislation. Of course, it would be prudent to treat these findings with due caution.
Nonetheless, the sensitivity analyses support the finding that the introduction of the smoking ban, at least to some degree, will have contributed to the reduction in emergency hospital admissions in men. No effect was observed when 2004 was used instead of 2007 as the year of introduction and a reduced effect was found when 2009 was used. The reduced effect for 2009 could be because of the overlap between the two periods being compared as regards the actual smoking ban duration. Indeed, it might be reasonable to expect the impact of the ban to have started much earlier than the actual year of implementation of the legislation- particularly since Scotland had implemented the ban in 2006 which could have possibly resulted in increased awareness among their fellow UK citizens and especially as a number of clubs, public bars and workplaces also introduced some restrictions on smoking in advance of the ban in 2007. Indeed, there is good reason why the kick-in period of any benefit of the legislation to COPD patients and those at risk of the disease might be as short as few weeks of its implementation since most emergency admissions for COPD are due to the exacerbations of the disease. Eisner (2009) has suggested COPD exacerbations are often triggered by exposure to irritants of which cigarette smoke is one. Indeed, Leuenberger et al (1994), Larsson et al (2003) and Celli et al (2004) have also reported that persistent exposure to tobacco smoke is a major cause of complications in COPD- most of which usually result in hospital admissions and according to Apsley and Semple (2012), meaningful decrease in exposure levels to passive smoking over a period as short as a few weeks could result in fewer exacerbations among the population at risk of COPD and its complications. Although the current study also found evidence of smoking ban effect for emergency hospital admissions on myocardial infarction, the magnitude of effect over the 5-year smoking ban period was much larger than the 2.4% reduction reported in the earlier UK study by Sims et al (2010) which was based on a much shorter duration. However the current results are within the range of levels reported in the US-based studies reported by Sargent et al (2004), Bartecchi et al (2006) and Khuder et al (2007)- all of which similarly involved long smoking ban durations. Furthermore, the absence of smoking ban effect on emergency hospital admissions for fracture of skull and facial bones is in line with expectation for a condition generally recognized as unrelated to smoking. Together, these imply that the effects found are likely not artefacts of the data and methodology used, and the observed effects can, at least to some extent, be attributed to the introduction of the ban.
Although extensive literature review would suggest no other major nationwide public health policy was introduced in England during the period of the smoking legislation which could account for the effect found for the ban, there might be, however, several possible other reasons that could explain, or may contribute to these findings. It is reasonable to expect COPD patients and indeed persons who are susceptible to smoking induced COPD to also benefit from the reduced levels of emergency admissions for myocardial infarction widely reported as resulting from the smoking ban since the condition is a known major risk factor for COPD. It is also reasonable to expect improvements in the management of the disease, most notably changes in the use of more effective drugs against COPD exacerbations over the study period as reported by Soriano et al (2002 and 2003) and also by Kiri et al (2005a and 2005b) as also likely to account for the reduction in emergency admissions for COPD.
Limitations
The current analyses were based on the following assumptions: that (1) the sex distribution of emergency admissions for COPD was similar to the corresponding distribution for all finished consultant episodes for COPD, (2) the age distribution of emergency admissions for COPD was similar to the distribution for all emergency admissions and (3) the age distribution was stable over the 10-year study period in each sex. Thus, the validity of the study findings might depend on the validity of these assumptions. According to data from the Public Health Intelligence Team of NHS Hounslow (2012), the assumptions might be reasonable.
A major limitation of the study was the unavailability of patient-level data, rich enough to include information on the key risk factors of COPD. Although the previous UK studies by Sims et al (2010) and Mackay et al (2010) also used aggregated HES data at national level in their analyses, both were based on weekly admissions and hence involved more robust statistical models.
Furthermore, although the estimated smoking ban effect was adjusted for changes in cigarette smoking prevalence, the reported level was still liable to bias from residual confounding. The likely impact would be that reductions in admissions due to decrease in active smoking levels might have been attributed to the ban. Another source of possible bias was the non-adjustment of the smoking ban effect by a number of important factors related to COPD, such as comorbidity, changes in the management of COPD and other known risk factors of COPD.
Indeed, an additional limitation of the study was the change in COPD diagnosis which occurred over the period of the study. While in 2001, according to GOLD 2001, chronic bronchitis was classified as stage 0 (i.e. at risk of COPD), this stage was deleted in 2006 when bronchitis chronic was classified as a different disease from COPD.
These are problems commonly associated with ecological studies and as such, the reported results require caution in their interpretation and any conclusions on possible causality.
Strengths
Ecological studies can provide evidence for identifying associations at the population level and as reported by Rose (1985), they are generally suitable for evaluating the effect of public health policy which would otherwise be very difficult to conduct. This study used freely available HES data to assess whether there was evidence of reductions in annual emergency admissions for COPD as a result of the implementation of the smoke-free legislation in England in 2007. It is the first study to assess the impact of the smoking ban on COPD.
Conclusions
The results of our study suggest emergency admissions for COPD declined significantly in men, but not in women, following the implementation of smoke-free legislation in England. This reduction of emergency admissions comes on top of those reported for other outcomes such as myocardial infarction and asthma, thereby further shifting its cost-benefit ratio further in favor of the implementation of the intervention. Because these trends were observed at an ecological level, the findings should be considered as indicative only and further investigation, using individual-level data, would be needed to more accurately estimate the impact of the introduction of the smoking ban in terms of the huge cost and quality of life implications of the thousands of emergency admission for COPD in the UK.
|
What is already known about this topic
Smoking is the most important cause of chronic obstructive pulmonary disease (COPD) and both active and secondhand smoke increase the risk of COPD exacerbations.
Although several studies have reported a reduction in emergency hospital admissions for important comorbid conditions of COPD such as asthma and myocardial infarction following the implementation of smoking ban legislations, there has been no such assessment of the impact on COPD.
What this study adds
There was significant reduction in emergency hospital admissions for COPD among men in the five years 2007-2011 of the smoking ban legislation in England.
There was no evidence of a change in emergency hospital admissions among women in the five years 2007-2011 of the smoking ban legislation in England.
These findings, if replicated, can help inform public health strategies for sustaining benefits resulting from current policies on COPD and also guide additional efforts aimed at further reducing the huge burden of the disease in England.
|
Acknowledgment
This work is dedicated to the memory of the late Dr George Visick, who until his death was a research colleague of VAK on the epidemiology of COPD.
Notes
Contributors: VAK developed the research proposal and is the principal investigator. VAK planned and undertook the analysis. FV contributed to the study design. Both VAK and FV drafted the paper.
Funding: This work was self-funded by VAK.
Competing interests: There was no conflict of interest. The authors declare that they had: (1) No financial support for the submitted work; (2) No financial relationships with commercial entities that might have an interest in the submitted work; (3) No spouses or partners who had relationships with commercial entities that might have an interest in the submitted work; (4) No non-financial interests that might be relevant to the submitted work.
Ethical approval: This study was based on anonymized records, and hence no ethical approval was required.
Data sharing: The study data are freely and publicly available.
References
1.Agresti, A. (2002) “Categorical Data Analysis,” (2nd edition). Wiley, New York
Publisher – Google Scholar
2.American Thoracic Society. (1995). “Standards for the Diagnosis and Care Of Patients with Chronic Obstructive Pulmonary Disease,” Am J Respir Crit Care Med, 152 s77—s121
Publisher – Google Scholar
3.Anecchino, C., Rossi, E., Fanizza, C., De Rosa, M., Tognoni, G., Romero, M. & working group ARNO project. (2007). “Prevalence of Chronic Obstructive Pulmonary Disease and Pattern of Comorbidities in a General Population,”International Journal of Chronic Obstructive Pulmonary Disease, 2(4) 567-574
Publisher – Google Scholar
4.Antó, J. M., Vermeire, P., Vestbo, J. & Sunyer, J. (2001). “Epidemiology of Chronic Obstructive Pulmonary Disease,”European Respiratory Journal, 17 982—94
Publisher – Google Scholar
5.Apsley, A. & Semple, S. (2012). “Secondhand Smoke Levels In Scottish Bars 5 Years on from the Introduction of Smoke-Free Legislation,” Tob Control, 21 (5) 511-3. doi: 10.1136/tobaccocontrol-2011-050107
Publisher – Google Scholar
6.Bartecchi, C., Alsever, R. N., Nevin-Woods, C., Thomas, W. M., Estacio, R. O., Bartelson, B. B. & Krantz, M. J. (2006). “Reduction in the Incidence of Acute Myocardial Infarction Associated with a Citywide Smoking Ordinance,”Circulation, 114 1490-1496
Publisher – Google Scholar
7.Berglund, D. J., Abbey, D. E., Lebowitz, M. D., Knutsen, S. F. & McDonnell, W. F. (1999). “Respiratory Symptoms and Pulmonary Function in an Elderly Nonsmoking Population,” Chest, 115 49e59
Publisher – Google Scholar
8.Boutin-Forzano, S., Moreau, D., Kalaboka, S., Gay, E., Bonnefoy, X., Carrozzi, L., Viegi, G., Charpin, D. & Annesi-Maesano, I. (2007). “Reported Prevalence and Co-Morbidity of Asthma, Chronic Bronchitis and Emphysema: A Pan-European Estimation,” The International Journal of Tuberculosis and Lung Disease, 11 695-702
Publisher – Google Scholar
9.Celli, B. R., MacNee, W., Agusti, A., Anzueto, A., Berg, B., Buist, A. S., Calverley, P. M. A., Chavannes, N., Dillard, T., Fahy, B., Fein, A., Heffner, J., Lareau, S., Meek, P., Martinez, F., McNicholas, W., Muris, J., Austegard, E., Pauwels, R., Rennard, S., Rossi, A., Siafakas, N., Tiep, B., Vestbo, J., Wouters, E. & ZuWallack, R. (2004). “Standards for the Diagnosis and Treatment of Patients with COPD: A Summary of the ATS/ERS Position Paper,”European Respiratory Journal, 23 (6) 932-946. doi: 10.1183/09031936.04.00014304
Publisher – Google Scholar
10.Cesaroni, G., Forastiere, F., Agabiti, N., Valente, P., Zuccaro, P. & Perucci, C. A. (2008). “Effect of the Italian Smoking Ban on Population Rates of Acute Coronary Events,” Circulation; 117 1183-1188
Publisher – Google Scholar
11.Cook, R. D. & Weisberg, S. (1982). ‘Residuals and Influence in Regression,’ Chapman and Hall
Google Scholar
12.Dayal, H. H., Khuder, S., Sharrar, R. & Trieff, N. (1994.) “Passive Smoking in Obstructive Respiratory Diseases in an Industrialized Urban Population,” Environmental Research, 65 161e71
Publisher – Google Scholar
13.Department of Health (DOH). (2005). ‘National Service Frameworks and Strategies,’ http://www.nhs.uk/NHSEngland/NSF/Pages/ChronicObstructivePulmonaryDisease.aspx
14.Eisner, M. D. (2009). “Clinical Year in Review III: Chronic Obstructive Pulmonary Disease, Treatment of Tobacco Dependence, Lung Cancer, and Lung Transplantation,” Proceedings of the American Thoracic Society, 6 500—505
Publisher – Google Scholar
15.Eisner, M. D., Iribarren, C., Yelin, E. H, Sidney, S., Katz, P. P., Sanchez, G. & Blanc, P. D. (2009). “The Impact of SHS Exposure on Health Status and Exacerbations among Patients with COPD,” International Journal of Chronic Obstructive Pulmonary Disease, 4 169-176
Publisher – Google Scholar
16.Esteve, J., Benhamou, E. & Raymond, L. (1994). “Statistical Methods in Cancer Research,” vol. IV: Descriptive Epidemiology. International Agency for Research on Cancer Scientific Publications No. 128, Lyon
Publisher – Google Scholar
17.Fletcher, C. M, Tinker, C. M., Peto, R. & Speizer, F. E. (1976). “The Natural History of Chronic Bronchitis and Emphysema,” Oxford, Oxford University Press Health and Social Care Information Centre (HSCIC), UK. (2013) http://www.hscic.gov.uk/searchcatalogue?q=title%3A%22Hospital+Episode+Statistics%2C+Admitted+patient+care+-+
England%22&area=&size=10&sort=Relevance [Last accessed 18/02/2015]
18.Holguin, F., Folch, E., Redd, S. C. & Mannino DM. (2005). “Comorbidity and Mortality in COPD-Related Hospitalizations in the United States,” 1979 to 2001,” Chest Journal, 128 2005-2011
Publisher – Google Scholar
19.Jordan, R. E., Cheng, K. K., Miller, M. R. & Adab P. (2011). “Passive Smoking and Chronic Obstructive Pulmonary Disease: Cross-Sectional Analysis of Data from the Health Survey for England,” BMJ Open, 1:e000153 doi:10.1136/bmjopen-2011-000153
Publisher – Google Scholar
20.Khuder, S. A, Milz, S., Jordan, T., Price, J., Silvestri, K. & Butler, P. l. (2007). “The Impact of a Smoking Ban on Hospital Admissions for Coronary Heart Disease,” Preventive Medicine, 45 3-8
Publisher – Google Scholar
21.Kiri, V. A., Bettoncelli, G., Testi, R. & Viegi, G. (2005a). “Inhaled Corticosteroids Are More Effective in COPD Patients When Used with LABA than with SABA,” Respiratory Medicine, 99 1115-1124
Publisher – Google Scholar
22.Kiri, V.A., Pride, N. B., Soriano, J. B. & Vestbo, J. (2005b). “Inhaled Corticosteroids in COPD: Results from Two Observational Designs Free of Immortal-Time bias,” American Journal of Respiratory and Critical Care Medicine, 172 460-464
Publisher – Google Scholar
23.LAIA: the Lung & Asthma Information Agency. (2001). “Trends in Emergency Hospital Admissions for Lung Disease,”St. George’s Hospital Medical School. Factsheet 2001/4
Publisher – Google Scholar
24.Larsson, M. L., Loit, L. H., Meren, M., Põlluste, J., Magnusson, A., Larsson, K. and Lundbäck, B.l. (2003). “Passive Smoking and Respiratory Symptoms in the FinEsS Study,” European Respiratory Journal, 21 672e6
Publisher – Google Scholar
25.Leuenberger, P., Schwartz, J., Ackermann-Liebrich, U., Blaser, K., Bolognini, G., Bongard, J. P., Brandli, O., Braun, P., Bron, C. & Brutsche, M. (1994). “Passive Smoking Exposure in Adults and Chronic Respiratory Symptoms (SAPALDIA Study), Swiss Study on Air Pollution and Lung Diseases in Adults, SAPALDIA Team,” American Journal of Respiratory and Critical Care Medicine, 150 1222e8
Publisher – Google Scholar
26.Mackey, D., Haw, S., Ayres, J. G., Fischbacher, C. & Pell, J. P. (2010). “Smoke-free Legislation and Hospitalizations for Childhood Asthma,” The New England Journal of Medicine, 363 1139-1145
Publisher – Google Scholar
27.Mannino, D. & Buist, A. S. (2007). “Global Burden of COPD: Risk Factors, Prevalence, and Future Trends.” The Lancet, 370 765—773
Publisher – Google Scholar
28.Mannino, D. M. & Kiri, V. A. (2006). “Changing the Burden of COPD Mortality,” International Journal of Chronic Obstructive Pulmonary Disease 1 (3) 219-233
Publisher – Google Scholar
29.McCullagh, P. & Nelder, J. A. (1989). ‘Generalised Linear Models (2nd edition),’ Chapman and Hall
30.National Heart, Lung & Blood Institute. (2012). “What Causes COPD?,” National institutes of Health.http://www.nhlbi.nih.gov/health/health-topics/topics/copd/causes.html
Publisher
31.NICE. (2010). ‘Chronic Obstructive Pulmonary Disease,’ NICE Clinical Guideline (June)
32.Office for National Statistics (ONS), UK. (2012). ‘General Lifestyle Survey Overview: A Report on the 2010 General Lifestyle Survey,’
http://www.cancerresearchuk.org/cancer-info/cancerstats/types/lung/smoking/lung-cancer-and-smoking-statistics#age [Last accessed 18/02/2015]
Google Scholar
33.Pauwels, R. A., Buist, A. S., Calverley, P. M., Jenkins, C.R., Hurd, S. S. & the GOLD Scientific Committee. (2001). “Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease, NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop Summary,” American Journal of Respiratory and Critical Care Medicine, 163 1256—1276
Publisher – Google Scholar
34.Public Health Intelligence Team – NHS Hounslow. (2012). “A fact sheet on Chronic Obstructive Pulmonary Disease (COPD) in the London Borough of Hounslow,” http://www.hounslow.gov.uk/jsna_2012_copd_datasheet.pdf [Last accessed 18/02/2015]
Publisher
35.Rose, G. (1985). “Sick Individuals and Sick Populations,” International Journal of Epidemiology, 14 32—38. doi: 10.1093/ije/14.1.32
Publisher – Google Scholar
36.Royal College of Physicians. (2005). ‘Going Smoke-Free: The Medical Case for Clean Air in the Home, At Work and in Public Places,’ A report by the Tobacco Advisory Group of the Royal College of Physicians. RCP
Google Scholar
37.Sargent, R. P., Shepard, R. M. & Glantz, S. A. (2004). “Reduced Incidence of Admissions for Myocardial Infarction Associated with Public Smoking Ban: Before and After Study,” BMJ, 328 977-980
Publisher – Google Scholar
38.Sims, M., Maxwell, R., Bauld, L. & Gilmore, A. (2010). “Short Term Impact of Smoke-Free Legislation in England: Retrospective Analysis of Hospital Admissions for Myocardial Infarction,” BMJ, 340 c2161. doi: http://dx.doi.org/10.1136/bmj.c2161
Publisher – Google Scholar
39.Soriano, J. B., Kiri, V. A., Pride, N. B. & Vestbo, J. (2003). “Inhaled Corticosteroids With/Without Long-Acting Beta Agonists Reduce the Risk of Re-Hospitalisation and Death in COPD Patients,” American Journal of Respiratory Medicine, 2 (1) 67-74
Publisher – Google Scholar
40.Soriano, J. B., Vestbo, J., Pride, N. B., Kiri, V., Maden, C. & Maier, W. C. (2002). “Survival in COPD Patients after Regular Use of Fluticasone Propionate and Salmeterol in General Practice,” European Respiratory Journal, 20 819-825
Publisher – Google Scholar
41.StatsDirect Ltd. StatsDirect Statistical Software. http://www.statsdirect.com. England: StatsDirect Ltd. 2013
42.The National Archives. (2006). “The Health Act 2006,” Chapter 1.http://www.legislation.gov.uk/ukpga/2006/28/contents [Last accessed 18/02/2015]
Publisher
43.U.S. Department of Health and Human Services. (2006). ‘The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General,’ Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Ofï¬ce on Smoking and Health
Google Scholar
44.Vasselli, S., Papini, P., Gaelone, D., Spizzichion, L., De Campora, E., Gnavi, R., Saitto, C., Binkin, N. & Laurendi G. (2008). “Reduction Incidence of Myocardial Infarction Associated with a National Legislative Ban on Smoking,” Minerva Cardioangiologica, 56 197-203
Publisher – Google Scholar
45.Vestbo. J., Agusti, A, Azuoento A., Fabbri, L., Jones, P., Martinez, F., Roche, N., Rodriquez-Roison, R., Sin, D., Stockley, R., Volgelmeier, C., Wedzicha, W. & the GOLD Scientific Committee. (2014). “Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease,” Chapter 1: Definition and overview. [Updated 2014]. www.goldcopd.org/uploads/users/files/GOLD_Report_2014_Jan23.pdf
46.Wardle, H. & Mindell, J. (2008). ‘Adult Cigarette Smoking and Exposure to Others’ Smoke,’ In: Craig R, Shelton N, eds. Health Survey for England 2007. Vol 1: Healthy lifestyles: knowledge, attitudes and behaviour. National Centre for Social Research and the Department of Epidemiology at University College Medical School London
47.WHO (2004). “The World Health Report 2004: Changing History,” Available at: www.who.int/whr/2004/en/. [Last accessed 18/02/2015]
Publisher
48.WHO (2012). “Programmes and Projects- Chronic Respiratory Diseases,”http://www.who.int/respiratory/copd/definition/en/index.html [Last accessed 18/02/2015]
Publisher
49.WHO (2014). “Tobacco Fact Sheet,” N°339. http://www.who.int/mediacentre/factsheets/fs339/en/ [Last accessed 18/02/2015]
Publisher
50.Zwar, N. A., Marks, G. B., Hermiz, O., Middleton, S., Comino, E. J., Hasan, I., Vagholkar, S. & Wilson, S. F. (2011). “Predictors of Accuracy of Diagnosis of Chronic Obstructive Pulmonary Disease in General Practice,” The Medical Journal of Australia, 195(4) 168-171
Publisher – Google Scholar