The patient was followed with periodic ultrasounds and there is no evidence of tumor in bladder or in upper urinary tract after 5 years of follow-up.
Discussion
Bladder transitional-cell carcinoma is extremely rare in the first two decades of life. The estimated frequency in patients under 40 is less than 1% in all cases (Khaisidy et al., 1990).
Previous history of exposure to carcinogenic agents; such as smoking, chemotherapy or radiation are well-known risk factors for bladder cancer in adults (Perez Niño el al. 2009). However, the prior exposure to toxic substances is not normally found in young patients. (Hoening et al. 1996; Khaisidy et al. 1990; Perez Niño et al. 2009; Ruiz et al. 2009, Paner et al. 2011; Giedl el al. 2006)
A significant association was found between urothelial tumors and a mutation in the p53 gene. In adults, this mutation is observed in highly differentiated and aggressive tumors, whereas in young people it is also present in low-grade tumors. A study by Linn et al. (1991), from 73 tumors in patients younger than 30 years, found 81% of them to be low-grade pTa tumors. Alterations in the p53 gene can be found in the majority of tumors, suggesting that the modification of this gene may not correlate with poor prognosis tumors.
The most commonly reported symptoms are in order of frequency: gross hematuria (80%), irritative urinary symptoms or recurrent urinary tract infections (15%) and microscopic hematuria (5%). (Khaisidy et al., 1990)
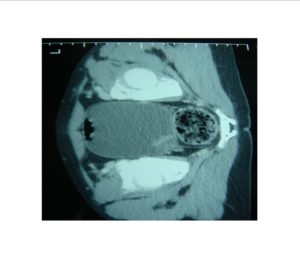
The diagnosis is usually done with ultrasound and cystoscopy (Hoenig et al. 1996; Dennery et al. 2002). The urine cytology has a low sensitivity in detecting these tumors. (Hoenig et al.1996; Lerena et al. 2010). This is probably because the majority of bladder tumors in these patients are low grade. In our case, the urinary cytology was negative; and although CT scan was performed to complete the study, it is usually not necessary.
The standard treatment is transurethral resection. It has not been described the use of immunotherapy or adjuvant chemotherapy in pediatric patients, due to the low aggressive nature of these tumors (Paner et al. 2011). These tumors appear normally as solitary lesions and are usually located in bladder trigone or in perimeatal area (Paner et al. 2011; Giedl et al. 2006)
A 97% of bladder cancer cases in children and adolescents are non-muscle-invasive tumors (Hoening et al. 1996; Khaisidy et al. 1990; Perez Niño et al. 2009; Ruiz et al. 2009, Paner et al. 2011; Giedl et al. 2006) this percentage being significantly higher than in adults. They are usually low-grade lesions (Giedl el al. 2006) and the recurrence rate is very low (2-5%) in contrast to what occurs in adults, where recurrence rate ranges between 60 and 70% (Perez Niño et al. 2009)
As a result of the low incidence of these tumors in childhood, there is no consensus on their follow-up. Many published series suggest a follow-up based on ultrasonography. Cystoscopy should only be performed in those cases where there is a high suspicion of recurrence; as in children and adolescents, these tumors have a very low recurrence rate, and this procedure requires general anesthesia in most cases (Hoening et al. 1996; Khaisidy et al. 1990; Perez Niño et al. 2009; Ruiz et al. 2009, Paner et al. 2011; Giedl et al. 2006; Lerena et al. 2010). Our patient was followed with periodic ultrasounds; however, a cystoscopy was performed at 3 years of follow-up for episode of gross hematuria with negative ultrasound.
In conclusion, the urothelial bladder tumors in childhood are rare. They are usually solitary tumors, non-muscle-invasive and low grade of malignancy, with an excellent prognosis. Transurethral resection is a definitive treatment, with a very low recurrence rate. The follow-up should be done with urinalysis, cytology and ultrasound. The cystoscopy should be reserved for selected necessary cases.
References
1. Dennery ,MP, Rushton, HG, Belman, AB. (2002) “Sonography for the detection and follow-up of primary nonsarcomatous bladder tumors in children,” Urology ,1,59
Google Scholar
2. Gakis G., Efstathiou J., Lerner SP. et al. (2013) “ICUD-EAU International Consultation on Bladder Cancer 2012: Radical Cystectomy and Bladder Preservation for Muscle-Invasive Urothelial Carcinoma of the Bladder” European Urology 63,45-57
Publisher – Google Scholar
3. Gied,l J. Wild, PJ. Stoehr, R. et al. (2006) “Urothelial neoplasms in individuals younger than 20 years show very few genetic alterations and have a favorable clinical outcome,”Verh Dtsch Ges Pathol, 90,253-63.
4. Hoenig, DM. McRae, S. Chen, SC. et al. (1996) “Transitional cell carcinoma of the bladder in the pediatric patient,”J Urol, 156,203—205.
Publisher – Google Scholar
5. Khaisidy, L. Khasu, B. Mallett, E. et al. (1990) “Transitional cell carcinoma of bladder in children,” Urology ,35,142-144.
Publisher – Google Scholar
6. Lerena, J., Krauel, L., García-Aparicio, L., et al. ( 2010) “Transitional cell carcinoma of the bladder in children and adolescents: Six-case series and review of the literature,” Journal of pediatric, 6, 481-485.
Google Scholar
7. Linn, J. F., Sesterhenn, I. Mostofi, F. K., Schoenberg, M. (1998)“The molecular characteristics of bladder cancer in young patients,” J Urol, 159, 1493.
Publisher – Google Scholar
8. Paner, GP. Zehnder, P. Amin, AM. Husain, AN. Desai, MM. (2011) “Urothelial neoplasms of the urinary bladder occurring in young adult and pediatric patients: a comprehensive review of literature with implications for patient management,” Adv Anat Pathol ,18 (1) 79-89.
Publisher – Google Scholar
9. Perez Niño, JF. Malo Rodríguez, G. Llinás Lemus, E. el al. (2009) “Comportamiento de las neoplasias uroteliales de vejiga en adolescentes,” Urol.colomb, 2,63-68.
Google Scholar
10. Ruiz, E. Alarcón Caba, M. Toselli, L. Moldes, J. Ormaechea, M. de Badiola, F,. Christiansen, S. (2009) “Transitional cell carcinoma of the bladder in adolescents: a diagnosis to bear in mind,” Arch Argent Pediatr, 107(1) 49-52.
Google Scholar