Introduction
The process of respiration is crucial for the functioning of living organisms. In the case of multicellular organisms, such as humans, respiration is primarily associated with gas exchange, where oxygen is taken in from the environment and carbon dioxide is removed from the body. The process of respiration can be divided into two types, namely external respiration and internal respiration. External respiration refers to the exchange of gases between the organism and the environment. It begins in the upper respiratory tract, where air is inhaled through the nostrils or mouth and passes through the nasal passages or throat. It then proceeds to the larynx, where it passes through the vocal cords, which help control the airflow. From the larynx, air reaches the trachea, which branches into two bronchi leading to the lungs. The bronchi are divided into smaller structures called bronchioles, which ultimately reach the pulmonary alveoli. The pulmonary alveoli are tiny sacs surrounded by a network of blood vessels, where actual gas exchange occurs. During respiration, oxygen diffuses from the pulmonary alveoli into blood vessels, a process known as diffusion. Oxygen binds to hemoglobin in red blood cells and is transported to all tissues of the body. At the same time, carbon dioxide, which is a by-product of metabolic processes, moves from the blood to the pulmonary alveoli and is exhaled. Internal respiration can be defined as the gas exchange between the blood and all cells in the body. After oxygen is taken up by the pulmonary alveoli, it is transported by the blood to the cells of the body, where it is utilized in cellular respiration, generating the necessary energy for the organism to function. The process of respiration is controlled by the respiratory center located in the brainstem, specifically in the area known as the NTS (Nucleus Tractus Solitarius) (AbuAlrob and Tadi, 2019). It is part of the peripheral nervous system, which receives information from receptors located in the arteries and efferent nerve fibers associated with the respiratory system. The respiratory center generates rhythmic nerve signals that lead to the contraction of the respiratory muscles. The rhythm and depth of the respiratory signals generated depend on the concentration of carbon dioxide and the pH of the blood. During inhalation, the intercostal muscles and diaphragm expand, increasing the volume of the chest cavity and causing a decrease in pressure within the lungs. Air is drawn into the lungs. Exhalation is the reverse process of inhalation, where the respiratory muscles contract, reducing the volume of the chest cavity and simultaneously pushing air out of the lungs (Feldman and Del Negro, 2006; Smith et al., 2013; Guyenet and Bayliss, 2015).
Taking into consideration the complicated and important nature of the respiratory process in sustaining life, a simulator has been devised to instruct medical students in identifying abnormalities that may arise during artificial respiration. The primary objective of this endeavor is to create a web application accessible to all individuals, enabling them to acquire proficiency in operating a mechanical ventilator. Employing mathematical models, the functions of the respiratory system and the ventilator have been intricately mapped, facilitating the accurate simulation of authentic challenges that can manifest during the process of patient ventilation.
Lungs and their functions
The lungs are a respiratory organ that performs several important functions in the human body in addition to gas exchange:
- breathing – the lungs allow gas exchange, which involves taking in oxygen from the air and removing carbon dioxide from the body. Gas exchange occurs in the lung alveoli, where oxygen from inhaled air enters the blood, and carbon dioxide exits the blood into exhaled air. This process depends on the concentration of gases in the blood and air, the partial pressures of carbon dioxide (CO2) and oxygen (O2), and the efficiency of gas diffusion (Weibel, Cournand and Richards, 1963; Paiva, 1973)
- air filtration – the lungs cleanse the air of dust, bacteria, viruses, and other harmful substances. The lungs use cells such as cilia, macrophages, and mucus production for this purpose (Yeh and Schum, 1980; Asgharian and Price, 2006; Kuek and Lee, 2020)
- blood pH regulation – the lungs influence the body’s acid-base homeostasis by regulating the concentration of hydrogen ions (H+) and bicarbonate ions (HCO3-) in the blood. When the concentration of CO2 in the blood increases, the lungs are stimulated to increase respiratory rate to remove excess CO2 and increase blood pH (Severinghaus, 1979; Ng, Bidani and Heming, 2004; Bohrn, 2006)
- protection against infections: The lungs have defense mechanisms, such as immune system cells, that protect against infections and diseases (Fels and Cohn, 1986; Linden et al., 2008)
- blood filtration – removal of toxic substances, excess water, and electrolytes from the blood (Scharfetter and Hutten, 1994)
- surfactant production: The lungs produce surfactant, which reduces the surface tension of lung alveoli and prevents their collapse (Goerke, 1974)
Respiratory failure is a condition characterized by the inability to maintain normal partial pressures of gases in arterial blood. Within respiratory failure, the mechanisms responsible are ventilatory failure (a decrease in alveolar ventilation) and shunt (resulting from intrapulmonary shunting) as well as mismatching of perfusion and ventilation (Bredenberg et al., 1969; Mendez and Hubmayr, 2005; Morales-Quinteros et al., 2019)
Ventilatory failure is defined as a decrease in alveolar ventilation below the level necessary to maintain normal alveolar gas partial pressure. Two types of ventilatory failure can be distinguished within this pathology. Pure ventilatory failure and respiratory diseases.
Within the first group, the following anatomical locations of dysfunction can be distinguished, leading to ventilatory failure:
- dysfunction of the respiratory neurons of the medulla oblongata, which are inhibited by hypoxia or high levels of PCO2,
- injury to upper motor neurons of the respiratory muscles,
- disease (including poliomyelitis) of the anterior horn cells of the spinal cord,
- injury to lower motor neurons of the respiratory muscles,
- impairment of neuromuscular junction function caused by botulism, muscle relaxants, organophosphorus compounds, nerve gases, and myasthenia gravis,
- loss of lung or chest wall elasticity,
- discontinuity of the chest wall,
- resistance in small airways,
- obstruction of the upper airways
The second group includes:
- asthma,
- chronic obstructive pulmonary disease,
- cystic fibrosis,
- pulmonary edema,
- pulmonary embolism,
- pulmonary hypertension,
- atelectasis,
- pulmonary fibrosis,
- lung cancer,
- pleural effusion,
- acute lung injury.
The respirator
A respirator is used when a patient has breathing difficulties and is unable to breathe independently (maintain adequate oxygen levels in the blood or remove carbon dioxide from the body). A respirator is used in the following situations (Dreyfuss and Saumon, 1998; Mascia et al., 2005; Wax, Kenny and Burns, 2006; Burns et al., 2011; Fan, Brodie and Slutsky, 2018):
- in the case of respiratory diseases (acute pneumonia, chronic obstructive pulmonary disease, asthma, and acute respiratory distress syndrome),
- in the case of non-respiratory diseases such as poisoning, Parkinson’s disease, and neurological diseases,
- after surgical procedures to provide the patient with adequate breathing support during recovery,
- in the case of injuries such as spinal cord or brain injuries that can affect the patient’s ability to breathe.
Mechanical lung ventilation – types
Spontaneous breathing – this is a mode of breathing that is not supported by any assistance.
With a ventilator:
- Invasive where the patient usually does not cooperate.
- Non-invasive where the patient always cooperates.
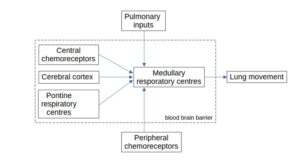
Control of spontaneous breathing is done through the analysis of partial pressures of PO2, PCO2, H+. Breathing movements are generated by central respiratory rhythm generators in various locations in the lower brainstem and then are output as motor activities. The controlling parameters are muscle strength, volume, and frequency of breathing (figure1).
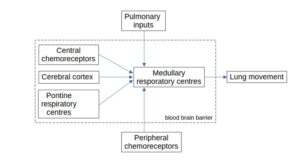 Fig 1. Spontaneous breath control system
Fig 1. Spontaneous breath control system
Invasive ventilation – it is conducted in patients using a ventilator and an endotracheal or tracheostomy tube. This method allows direct access to the airways. The patient usually does not cooperate.
In this medical method, respiratory parameters such as respiratory rate, tidal volume, and inspiratory pressure can be precisely controlled. It is used in cases where the patient has damaged airways, or their airways are characterized by a serious inflammatory condition – invasive ventilation protects the airways from further damage and allows for their regeneration. However, the use of this type of ventilation carries the risk of respiratory tract infections (including pneumonia), damage to respiratory tract tissues (both during intubation and during prolonged ventilation). Additionally, prolonged invasive ventilation can lead to complications such as barotrauma or hypotension.
Non-invasive ventilation – it is conducted using a ventilator and a mask. The patient almost always cooperates. It is used in patients who are both life-threatening and in patients who require respiratory support during sleep. Usually, during non-invasive ventilation, sedative drugs are not administered to the patient, and the patient is conscious; the treatment requires cooperation with the patient. The process of assisting breathing is carried out through a tight-fitting mask placed on the patient’s face and the ventilator.
Non-invasive ventilation (NIV) is a method of assisting the patient’s breathing that allows the use of an endotracheal or tracheostomy tube. Non-invasive ventilation helps avoid the potential complications associated with invasive mechanical ventilation. It is used in patients with acute and chronic respiratory failure, as well as in the weaning process from the ventilator, and to prevent intubation.
The asynchrony
Respiratory synchronization is crucial to ensure that mechanical ventilation is effective and safe for the patient. Proper synchronization involves matching the timing, volume, and flow of the respirator with the patient’s breathing patterns. This synchronization is necessary to avoid overdistention or collapse of the lungs, which can lead to lung injury and impaired gas exchange.
Several factors can cause synchronization issues during mechanical ventilation. These include asynchrony between the patient’s ventilator, improper respirator settings, and changes in the patient’s respiratory mechanics. Patient-ventilator asynchrony occurs when the timing, volume, or flow of the respirator does not match the patient’s breathing patterns. This can result in increased respiratory effort, lung injury, and decreased oxygenation. Improper ventilation settings, such as inadequate tidal volumes or high respiratory rates, can also lead to synchronization problems. Changes in the patient’s respiratory mechanics, such as airway obstruction or changes in lung compliance, can also affect synchronization (Epstein, 2011; Holanda et al., 2018; Ohshimo, 2021).
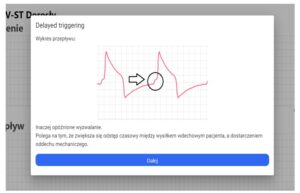
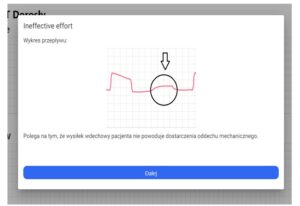
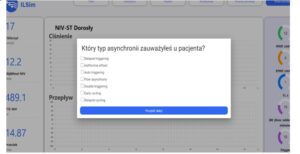
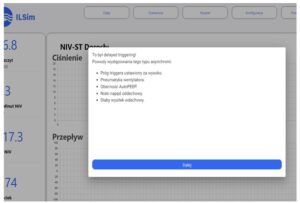
Asynchrony during the use of ventilators is a situation in which the patient’s breathing cycle is not synchronized with the ventilator’s breathing cycle. This leads to prolonged hospitalization and contributes to increased mortality. There are different types of asynchronies during the use of ventilators, and their precise identification is important in order to choose the appropriate ventilation mode and provide effective patient treatment. Here are some examples of types of asynchronies during the use of ventilators (De Wit et al., 2009; Blanch et al., 2015; De Haro et al., 2019):
- trigger asynchrony – the patient has difficulty initiating a breath, and the ventilator does not respond to the patient’s breathing attempts. As a result, the patient is exposed to breathing effort and may experience respiratory muscle fatigue.
- cycle asynchrony – the ventilatory volume delivered by the ventilator is not adjusted to the patient’s needs, which may lead to inappropriate breathing rate of the patient.
- volume asynchrony – the ventilator delivers a volume that is too small or too large compared to the patient’s needs. As a result, inadequate lung ventilation may occur.
- synchrony asynchrony – the patient’s breathing cycle and the ventilator’s cycle are unsynchronized, which may lead to inappropriate breathing rate of the patient.
- latency asynchrony – the patient initiates breathing, but the ventilator does not deliver ventilatory volume quickly enough, leading to delayed ventilator response.
To combat asynchrony, the following methods can be distinguished (Younes, 1992; Tobin, 2001; Sinderby and Beck, 2008; Mellott et al., 2009; Dres, Rittayamai and Brochard, 2016; Daniel and Ivan, 2017; Arnal and others, 2018):
- Assist Control Ventilation – this mode of ventilation allows the patient to independently initiate the breathing cycle, and, if necessary, the ventilator provides support in the form of selected ventilatory volume. This mode helps to avoid asynchrony between the patient and the ventilator.
- Volume-Targeted Synchronized Intermittent Mandatory Ventilation – this method synchronizes the patient’s breathing with the ventilator. The ventilator delivers the selected ventilatory volume and, if the patient independently starts breathing, the ventilator synchronizes the breathing cycle with the patient. This method allows for avoiding asynchrony and increasing ventilation efficiency.
- Use of high-sensitivity ventilators – modern ventilators use airflow velocity sensors that can detect even small changes in ventilatory volume and adjust ventilatory volume to the patient’s needs. This method helps to avoid asynchrony and provides better control over the patient’s breathing.
Models of breathing
Model of spontaneous breathing mechanics
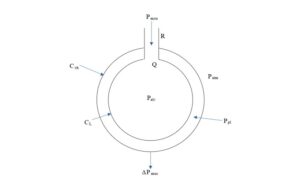
The breathing pattern for a single alveolus is shown in the diagram.
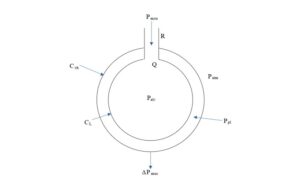
Fig 2. A single alveolus and parameters describing the process of gas exchange
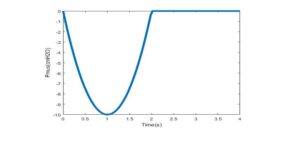
In the spontaneous breathing mode, we have the following parameter dependence:
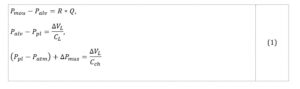
where:
Pmou is the pressure at the mouth of the airway;
Ppl is the pressure in the intrapleural space;
Patm is atmospheric pressure;
Palv is alveolar pressure;
Pmus is the difference in muscle pressure;
Q is the volumetric flow, which is positive during inspiration and negative during exhalation;
ΔVL is the change in lung volume;
R is the resistance of the respiratory system;
CL stands for lung compliance;
Cch is the compliance wall of the chest;
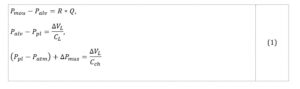
Muscle strength as a regulatory signal can be simulated, for example, in the form of a curve as shown in figure 3.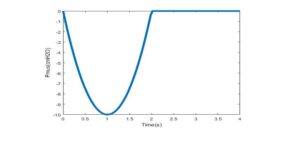
Fig 3. The typical shape of muscle pressure curve (respiratory muscular pressure used to drive the mechanical lung. Increase, hold and release are expressed as a fraction of Ttot.)
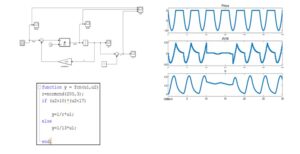
Using model (1), various respiratory system disorders can be simulated. To achieve this, special functions need to be established for variable parameters such as respiratory system resistance or lung compliance. The simulation scheme in the MATLAB/Simulink environment is shown in figure 4. Using the resistance change function (depicted in figure 4), the constant resistance can be altered to a programmed value corresponding to the specific disorder mode. Sample graphs for the case of airway constriction are also shown in figure 4.
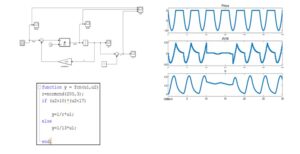
Fig 4. Example of resistance changes simulation
It should be noted that the control signal (Pmus) is generated based on the analysis of gas exchange. This topic will be the subject of a future article.
Model of mechanical ventilation
In this case, model (2) includes two possible sources of pressure control – muscular Pmus and ventilator Pvent.

where:
Pvent is the airway pressure applied by the ventilator;
Pmus is the pressure generated by the patient’s inspiratory muscles;
VT is the tidal volume;
CRS is the compliance of the respiratory system;
Raw is resistance in the respiratory tract;
dVi/dt is the inspiratory flow;
PEEP (positive end expiratory pressure) set on the ventilator;
PEEPi is self-peeling (auto-PEEP);
Resistance – a measure of the resistance to gas flow caused by the internal friction of the respiratory airflow, as well as the friction between the respiratory air and the airways. Unit: cmH2O/l/s
Compliance – a measure of lung elasticity, referring to the ability of the lungs to expand, defined as the change in lung volume (deltaV) per unit change in pressure (deltaP).
In the case of invasive ventilation, the main factor affecting lung function is the control by the ventilator. The patient typically does not cooperate with the ventilator and is sedated to reduce neural activity. Additionally, this mode of lung ventilation requires intubation, which involves inserting a plastic tube into the trachea.
Therefore, the challenge for the physician is to “replace” spontaneous breathing, which, as mentioned earlier, relies on gasometric parameters. From the perspective of respiratory mechanics, controlling the ventilator in invasive mode is relatively straightforward and involves maintaining appropriate pressure, flow, and volume settings for the delivered air. Additionally, the physician must make decisions regarding supplemental oxygenation based on gasometric results.
The most significant aspect of this mode is that the entire volume of air from the ventilator is delivered to the lungs during the inspiratory phase through the inspiratory pathway, and an appropriate amount of exhaled air exits through the expiratory pathway without any leakage. Since the patient does not “cooperate” with the ventilator, issues such as asynchrony are less likely to occur. However, lung parameters (resistance and compliance) can change during ventilation, and the physician must react to these changes as well.
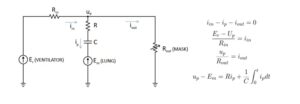
In the non-invasive ventilation mode, the model will have an additional component, Rout, which accounts for leakage. The schematic diagram and mathematical model of such a system are shown in figure 5.
The proposed model serves as a basis for simulating leaks and asynchrony.
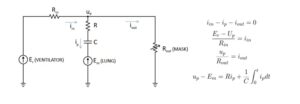 Fig 5. Breathing pattern with non-invasive ventilation
Fig 5. Breathing pattern with non-invasive ventilation
Leaks
Leaks are undesired phenomena during ventilation that impact treatment quality and the amount of delivered air. The causes of leaks can include:
- Inadequate sealing between the ventilator and the respiratory system.
- Variable resistance in the upper airways.
It is crucial to promptly recognize leaks and eliminate them immediately.
To model leaks, the parameter Rout is used. When using a mask, intentional leaks occur, which are determined by the mask parameters and depend on its type.
The leakage caused by mask imperfections on the face can be modeled as a variable Rout(t). Typically, this is a non-linear function. To simulate leaks, a simulation model was created with the ability to manually adjust the relevant parameters (figure 6).
Fig 6. Interface of breathing system simulation
The application
In modern times, one of the most crucial aspects of treating patients with various respiratory diseases is the use of medical ventilators. In the context of the COVID-19 pandemic, the utilization of these devices has become even more critical and widespread in ensuring proper patient monitoring worldwide. With the introduction of an increasing number of new types of ventilators to the market, along with the diversity of control methods and systems, there is a growing need to train new healthcare professionals in operating these devices.
As a result of these factors, there is an urgent need to develop a virtual system that enables the simulation of the real functioning of ventilators and facilitates rapid personnel training and research in the field of these devices. Such a system could significantly expedite the process of medical staff education, save costs on purchasing equipment for training purposes, and aid in the development of improved treatment protocols and enhanced effectiveness of respiratory therapies.
In light of these considerations, the development of virtual systems for simulating medical ventilators is one of the key challenges in the healthcare sector. Such systems can contribute to increased training efficiency and quality, as well as improve patient treatment outcomes. Therefore, future research and investments in this area are essential for further advancements in the field of medicine and providing better healthcare for patients.
Proposal for a solution using the described mathematical algorithms
A web-based application that allows for the control of a ventilator in volume and pressure modes has been developed for use through a web browser. This application ILSim was created as a diploma thesis in the Department of Informatics by Mr. Patryk Wawrzonkowski.
Within the application, models of various types of ventilators have been implemented, including invasive and non-invasive ventilators, enabling the adjustment of parameters such as PIP (Peak Inspiratory Pressure), PEEP (Positive End-Expiratory Pressure), Ti (Inspiratory Time), RR (Respiratory Rate), and Vt (Tidal Volume). The application also allows for the modification of respiratory system parameters such as resistance and airway resistance, as well as lung compliance.
By utilizing the application, users can visualize key parameters related to the breathing process, such as airflow, lung pressure, and Vt (minute ventilation). Additionally, the application allows for monitoring other important aspects related to the breathing process, such as air leaks.
All these features make the web-based application for simulating ventilator control and patient simulation an invaluable training tool for medical personnel and facilitate research related to ventilators and the breathing process. Consequently, the development of such applications has tremendous potential in improving the quality of training and treatment for patients with respiratory diseases.
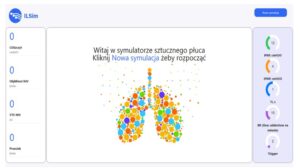
Fig 7. View of the start screen of the ventilator simulation application
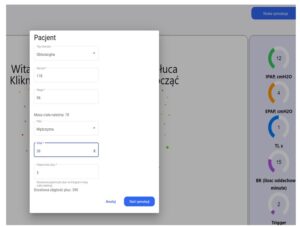
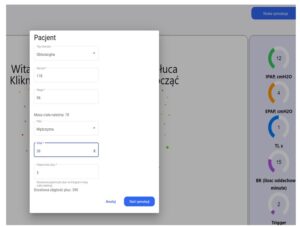
Fig 8. Set up patient parameters before starting the simulation Fig 9. Ventilator and patient simulation mode screen
Fig 9. Ventilator and patient simulation mode screen
Fig 10. Learning mode screen during simulation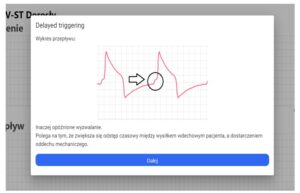
Fig 11. Screen demonstrations of learning mode steps – 1
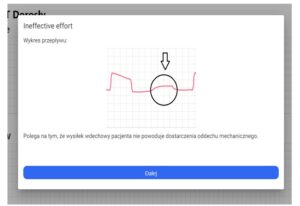
Fig 12. Demonstrations of successive steps in the training mode – 2
As part of the system that allows simulation of ventilator control and simulation of a patient connected to the ventilator, there is an option to simulate various emergency scenarios that may occur during normal device operation. These emergency scenarios are generated randomly, requiring appropriate actions from the trainer.
By doing so, the user can practically learn how to respond to different unforeseen situations that may arise while using the ventilator. During training, each decision made by the user is evaluated for correctness, allowing for progress monitoring in learning and detecting any potential errors.
Simulating various emergency scenarios during training also allows for the modification of ventilator configurations to adapt to specific requirements. This, in turn, increases the flexibility of the ventilator in case of unforeseen situations, which can greatly impact the quality of medical assistance provided.
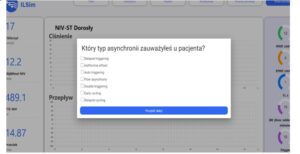
Fig 13. An example of a question screen with answer options to choose from after a random event during the simulation
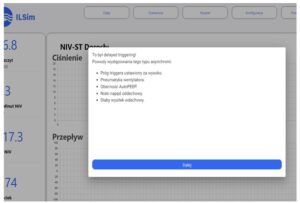
Fig 14. An example of a screen with the correct answer and additional information – 1
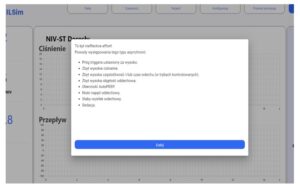
Fig 15. An example of a screen with the correct answer and additional information – 2
The system implementation process
In this article, we describe a computer system that is used for ventilator simulation. This system is accessed through a web browser, which means it does not require specialized hardware or software.
To begin the implementation, a selected group of students from a medical university is identified. These students are provided with dedicated user accounts, which are distributed via email. These accounts grant the students access to the ventilator simulation system, allowing them to log in and utilize its features.
Upon logging into the system, each student is equipped with a unique set of input data that describes the patient they will be examining during the simulation. These data contain crucial information about the patient, including their disease type, height, weight, gender, age, and lung capacity. The availability of these details facilitates a comprehensive and realistic simulation experience for the students.
Once the input data are entered into the system, the student can start the simulation and choose a desired scenario. The system is designed to support multiple test-training sessions simultaneously, allowing all students within the selected group to use it concurrently. This feature of concurrent usage promotes collaboration and allows efficient utilization of the ventilator simulation system.
During the simulation, the system diligently records the test results achieved by each student. These results play a crucial role in the subsequent stages of the implementation process, as they are utilized to evaluate the accuracy of the student’s responses to anomalous situations encountered during the simulation. By assessing the correctness of the students’ actions, the system provides valuable feedback for continuous improvement.
The test results are recorded and utilized in subsequent stages to evaluate the correctness of the student’s response to anomalous situations during the simulation. As a result, the ventilator simulation system serves not only as a training tool but also enables continuous monitoring of the students’ progress.
The implementation of the ventilator simulation system involves the setup of user accounts for a selected group of students, provision of patient data, execution of simulations with concurrent usage, recording of test results, and continuous progress monitoring. By encompassing these steps, the system provides a valuable training tool for medical students while enabling educators to monitor and assess their progress effectively.
Conclusion
In conclusion, ensuring proper respiratory synchronization is crucial for effective and safe mechanical ventilation in patients who cannot breathe adequately on their own. Synchronization involves matching the timing, volume, and flow of the respirator with the patient’s breathing patterns to avoid negative consequences such as respiratory distress and lung injury. Common problems that can arise during mechanical ventilation include patient ventilator asynchrony, improper respirator settings, and changes in patient respiratory mechanics. Asynchrony between the patient and the ventilator can lead to increased respiratory effort, lung injury, and decreased oxygenation. Improper ventilation settings can also cause synchronization problems. Changes in the patient’s respiratory mechanics, such as airway obstruction, or changes in lung compliance can further affect synchronization. Addressing these challenges and improving synchronization is essential to reduce the risk of harm to patients while also optimizing the costs of training for medical personnel. The ongoing research focuses on developing methods and technologies to improve synchronization and optimize mechanical ventilation strategies for better patient outcomes.
References
- AbuAlrob, M.A. and Tadi, P. (2019) ‘Neuroanatomy, nucleus solitarius’.
- Arnal, J.-M. and others (2018) Monitoring mechanical ventilation using ventilator waveforms.
- Asgharian, B. and Price, O.T. (2006) ‘Airflow distribution in the human lung and its influence on particle deposition’, Inhalation Toxicology, 18(10), 795–801.
- Blanch, L. et al. (2015) ‘Asynchronies during mechanical ventilation are associated with mortality’, Intensive care medicine, 41, 633–641.
- Bohrn, M.A. (2006) ‘CAPNOGRAPHY: CLINICAL ASPECTS.: Edited by Joachim S. Gravenstein, Michael B. Jaffe, and David A. Paulus. Cambridge, United Kingdom: Cambridge University Press, 2004, 441 pages, 119.20 (hardcover).’, Academic Emergency Medicine, 13(7), e6.
- Bredenberg, C.E. et al. (1969) ‘Respiratory failure in shock.’, Annals of surgery, 169(3), 392.
- Burns, K.E.A. et al. (2011) ‘Pressure and volume limited ventilation for the ventilatory management of patients with acute lung injury: a systematic review and meta-analysis’, PLOS one, 6(1), e14623.
- Daniel, H. and Ivan, I. (2017) ‘Identifying patient-ventilator asynchrony using waveform analysis’, Palliat Med Care, 4(4), 1–6.
- Dres, M., Rittayamai, N. and Brochard, L. (2016) ‘Monitoring patient–ventilator asynchrony’, Current opinion in critical care, 22(3), 246–253.
- Dreyfuss, D. and Saumon, G. (1998) ‘From ventilator-induced lung injury to multiple organ dysfunction?’, Intensive care medicine, 24(2), 102.
- Epstein, S.K. (2011) ‘How often does patient-ventilator asynchrony occur and what are the consequences?’, Respiratory care, 56(1), 25–38.
- Fan, E., Brodie, D. and Slutsky, A.S. (2018) ‘Acute respiratory distress syndrome: advances in diagnosis and treatment’, Jama, 319(7), 698–710.
- Feldman, J.L. and Del Negro, C.A. (2006) ‘Looking for inspiration: new perspectives on respiratory rhythm’, Nature Reviews Neuroscience, 7(3), 232–241.
- Fels, A.O. and Cohn, Z.A. (1986) ‘The alveolar macrophage’, Journal of applied physiology, 60(2), 353–369.
- Goerke, J. (1974) ‘Lung surfactant’, Biochimica et Biophysica Acta (BBA)-Reviews on Biomembranes, 344(3–4), 241–261.
- Guyenet, P.G. and Bayliss, D.A. (2015) ‘Neural control of breathing and CO2 homeostasis’, Neuron, 87(5), 946–961.
- De Haro, C. et al. (2019) ‘Patient-ventilator asynchronies during mechanical ventilation: current knowledge and research priorities’, Intensive care medicine experimental, 7, 1–14.
- Holanda, M.A. et al. (2018) ‘Patient-ventilator asynchrony’, Jornal Brasileiro de Pneumologia, 44, 321–333.
- Kuek, L.E. and Lee, R.J. (2020) ‘First contact: the role of respiratory cilia in host-pathogen interactions in the airways’, American Journal of Physiology-Lung Cellular and Molecular Physiology, 319(4), L603–L619.
- Linden, S.K. et al. (2008) ‘Mucins in the mucosal barrier to infection’, Mucosal immunology, 1(3), 183–197.
- Mascia, L. et al. (2005) ‘Cerebro-pulmonary interactions during the application of low levels of positive end-expiratory pressure’, Intensive care medicine, 31, 373–379.
- Mellott, K.G. et al. (2009) ‘Patient-ventilator dyssynchrony: clinical significance and implications for practice.’, Critical Care Nurse, 29(6), 41–55.
- Mendez, J.L. and Hubmayr, R.D. (2005) ‘New insights into the pathology of acute respiratory failure’, Current opinion in critical care, 11(1), 29–36.
- Morales-Quinteros, L. et al. (2019) ‘The role of hypercapnia in acute respiratory failure’, Intensive care medicine experimental, 7(1), 1–12.
- Ng, A.W., Bidani, A. and Heming, T.A. (2004) ‘Innate host defense of the lung: effects of lung-lining fluid pH’, Lung, 182, 297–317.
- Ohshimo, S. (2021) ‘Oxygen administration for patients with ARDS’, Journal of Intensive Care, 9(1), 1–14.
- Paiva, M. (1973) ‘Gas transport in the human lung’, Journal of Applied Physiology, 35(3), 401–410.
- Scharfetter, H. and Hutten, H. (1994) ‘Computer model for simulating control of the water and electrolyte state in the human body’, in System Modelling and Optimization: Proceedings of the 16th IFIP-TC7 Conference, Compiègne, France—July 5–9, 1993, 402–411.
- Severinghaus, J.W. (1979) ‘Simple, accurate equations for human blood O2 dissociation computations’, Journal of Applied Physiology, 46(3), 599–602.
- Sinderby, C. and Beck, J. (2008) ‘Proportional assist ventilation and neurally adjusted ventilatory assist—better approaches to patient ventilator synchrony?’, Clinics in chest medicine, 29(2), 329–342.
- Smith, J.C. et al. (2013) ‘Brainstem respiratory networks: building blocks and microcircuits’, Trends in neurosciences, 36(3), 152–162.
- Tobin, M.J. (2001) ‘Advances in mechanical ventilation’, New England Journal of Medicine, 344(26), 1986–1996.
- Wax, R.S., Kenny, L. and Burns, P. (2006) ‘Educating providers of mechanical ventilation: an update’, Current opinion in critical care, 12(1), 61–66.
- Weibel, E.R., Cournand, A.F. and Richards, D.W. (1963) Morphometry of the human lung. Springer.
- De Wit, M. et al. (2009) ‘Ineffective triggering predicts increased duration of mechanical ventilation’, Critical care medicine, 37(10), 2740–2745.
- Yeh, H.-C. and Schum, G.M. (1980) ‘Models of human lung airways and their application to inhaled particle deposition’, Bulletin of mathematical biology, 42(3), 461–480.
- Younes, M. (1992) ‘Proportional assist ventilation, a new approach to ventilatory support’, Am Rev Respir Dis, 145(1), 114–120.