Introduction
Dermographism is a chronic form of physical urticaria in which the skin becomes raised and inflamed when stroked, scratched, rubbed, and sometimes even slapped.9 It has been reported that dermographism has an unpredictable course and is exacerbated by stress, nervousness and exhaustion.6,7 To the authors’ knowledge, in the dental literature there is only one publication which described the cases of dermographism developed after dental procedure.5 Prosthesis used for the rehabilitation of missing teeth and surrounding oral tissues may cause complications like hypersensitivity, ulceration, pain etc. Allergic reactions caused by prosthesis materials are infrequently reported, however, and in particular acrylic hypersensitivity reactions have been described.1
Allergic reactions is usually manifested by the release of several chemical constituents from the material e.g. methyl methacrylate. Allergic reactions due to the incorporated coloring agents were also reported1.
Case Description and Results
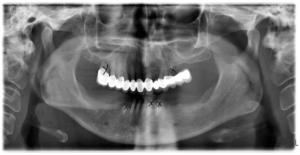
A 50-year-old female presented to our clinic for prosthodontic rehabilitation. There was a fixed partial bridge on her upper jaw. Her lower jaw had been restorated with fixed partial bridge and removable partial denture (Fig 1), but she could never use the removable denture. After the clinical examination, patient was informed about the need for extraction and replacement of some of the teeth. 3 weeks after the extractions, she was treated with tooth-retained overdenture in the upper jaw (Fig 2) and implant-retained overdenture in her lower jaw (Fig 3). Chrome-cobalt framework and precision attachments with conventional methyl methacrylate denture base material was used for restoring the upper denture. Lower denture containing chrome, cobalt and methyl methacrylate was also made. However she presented with erythema mucosal hyperplasia on the hard palate associated with burning sensation and bleeding following the dental treatment (Fig 4). It was decided to provide replacement of denture base material with a clear heat-cure acrylic resin (Orthocryl EQ, Dentaurum, Inspringen, Germany). She uncounted some symptoms following this, oral discomfort, erytheme in mucosa and itch. Currently, there are ranges of alternatives to the PMMA-based heat-polymerized denture base materials available. One of the alternatives to the denture with classic PMMA resins for patients who are allergic to MMA monomer is injection molded polyamide denture.
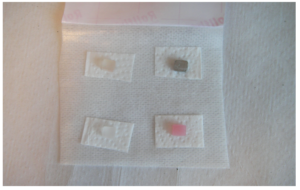
Patient was referred to the Dermatology Department before the new prosthetic rehabilitation with a polyamide material. Patient was allergy tested by means of patch test on the upper back according to the ICDRG criteria. All patch test materials and detailed instructions were sent to the dermatologists prior to testing.
Patch test materials prepared by cutting with dimensions of 1.0 ± 0.2 mm, 1.0 ± 0.2 mm, and 1.0 ± 0.2 mm, are as follows (Fig 5):
– Cr- Co (BEGO Medical, Bremen, Germany)
– PMMA-based heat-polymerized denture base material (Meliodent, Heraeus Kulzer Ltd, Hanau, Germany)
– PMMA-based heat-polymerized denture base material, clear (Orthocryl EQ, Dentaurum, Inspringen, Germany)
– Polyamide-based injected molded base material (Deflex, Buenos Aires, Argentina)
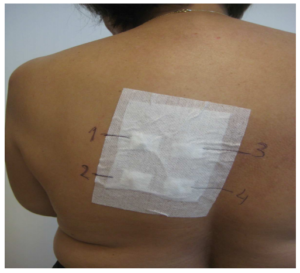
The test area was marked, so that allergens may be identified at reaction sites. The test area was kept dry, initially, to ensure adequate contact of allergen with the skin, but ultimately to ensure that the identification markings were preserved. The samples were placed on the upper back, the best site for reproducibility and also, for convenience, being a large flat surface. (Fig 6 and 7)
The reading was performed on days 2 and 4 and was classified according to the strength of reaction. No irritant reaction was observed on testing sites. However, red dermographic line of contact developed with small islands of edema. (Fig 8). She was then tested at the clinic for pressure urticaria with scratching. People with this form of chronic urticaria are sensitive to touch and pressure, as well as scratching2. The scratching lines were sustained for the 45 minutes of the consultation. (Fig 9)
Diagnosis is confirmed by means of a dermographometer (HTZ Limited, Vulcan Way, New Addington, Croydon, Surrey, CRO 9UG, UK), which is designed to apply a rubbing stimulus to the subject’s skin using predefined and reproducible pressures. It has spring-loaded smooth steel, which is 0.9 mm in diameter. The pressure on the tip was set to 100 g/mm2 by turning a screw at the top of the instrument. Device was applied perpendicularly for 70 seconds on the upper back during testing. Test sites showed a delayed red palpable swelling therefore the test was considered positive. Test sites inspected and test responses assessed approximately 6 hours after the end of provocation testing by physician, that is when the edema is usually at its most intensity.
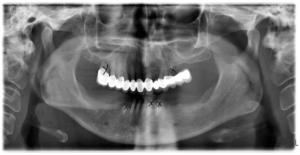
Figure 1: Panoramic view before treatment

Figure 2: Upper jaw overdenture prepared with chrom-cobalt framework conventional methymethacrylate denture base material

Figure 3: Two implant ball attachments placed for implant retained overdenture in her lower jaw
Figure 4: Reddened mucosal hyperplasia on the hard palate associated with burning sensation and bleeding following the dental treatment
Figure 5: Patch test materials prepared by cutting with dimensions of 1.0 ± 0.2 mm, 1.0 ± 0.2 mm,
and 1.0 ± 0.2 mm.
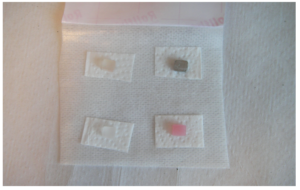
Figure 6: The samples just before placing on the upper back
Figure 7: Upper back of the patient with placed test samples
Figure 8: Red dermographic line of contact developed with small islands of edema after the patch test

Figure 9: Pressure dermographism from scratching after 45 minutes
Discussion
Symptomatic dermographism affects approximately 5% of the normal population and has an unpredictable course that may last from 5 to 7 years4. During the dental treatment; dentist should not only take care of one’s teeth and mouth but also take care of general health conditions.
This paper aimed at drawing attention to a possible complication of a minimally invasive treatment like mucosal reactions appearance in oral cavity following the conventional prosthetic therapy, outlining the complex etiology of systemic factors. Both finding out and eliminating the etiological factor before or during the treatment is essential for success.
The pressure dermographism represents one of the types of urticaria that is most difficult to control. The primary management is to orient patients to avoid situations that trigger the lesions. Medical therapy is generally unsatisfactory and includes antihistamines, non-steroidal anti-inflammatory drugs (NSAIDS), topical or systemic corticosteroids, sulphasalazine and dapsone.3
The main objective of the dental treatment plan was to find out how the edentulous alveolar ridge can be minimally loaded and how the load can be distributed on the abutment teeth. Implant and tooth retained full-mouth fixed partial denture can be the first choice of the treatment.
Secondly, removable partial dentures can be designed based on the selective tissue placement impression method. Szabó and Farkas8 mentioned that to maximally utilize the advantages of the mixed (dental and mucogingival) support, after the metal framework has been tried in, a second functional impression was taken. It is clear that in case of a known pressure urticaria, clinician should try to keep the occlusal load on edentulous mucosa in a tolerable level.
References
1. Barclay SC, Forsyth A, Felix DH, Watson IB. Case report–hypersensitivity to denture materials. Br Dent J. 1999 Oct 9; 187:350-2.
Publisher – Google Scholar
2. Barlow RJ, Warburton F, Watson K, Black AK, Greaves MW. Diagnosis and incidence of delayed pressure urticaria in patients with chronic urticaria. J Am Acad Dermatol. 1993 Dec; 29:954-8.
Publisher – Google Scholar
3. Dortas SD Jr, Valle SO, Pires AH, Guimarães PV, Jorge AS. [Delayed pressure urticaria with systemic manifestations: Case report]. An Bras Dermatol. 2009 Nov-Dec; 84:671-4.
Publisher – Google Scholar
4. Grattan CEH, Black AK. Urticaria and angioedema. In: Bolognia JL, Jorizzo JL, Rapini RP, et al, editors, Dermatology. Philadelphia (PA): Mosby; 2003.p.293.
5. Jauhar S, Staines K, McQueen M, Watson IB, Wray D, Felix DH. Dermographism and delayed pressure urticaria.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Jun; 103:774-9.
Publisher – Google Scholar
6. Juhlin L. Recurrent urticarial: clinical investigation of 330 patients. Br J Dermatol 1981; 104:369-81.
Publisher – Google Scholar
7. Michaelsson G. Chronic urticaria. A clical study with special reference to vascular reactions mediated by kallikreinkinin system. Acta Derm Venerol 1969; 49:404-16.
8. Szabó G, Farkas B. Prosthodontic treatment in delayed pressure urticaria. Fogorv Sz 2002;95(6):235-9.
9. Zuberbier T, Bindslev-Jensen C, Canonica W, Grattan CE, Henz BM, et al. EAACI/GA2LEN/EDF guideline: definition, classification and diagnosis of urticarial. Allergy 2006; 61:316-20.
Publisher – Google Scholar