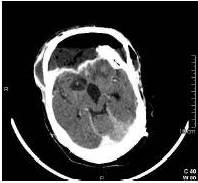
Emergency surgical intervention was performed and immediately after skin incision purulent exudate was visible. Cranioplasty was removed and a fetid collection was observed underneath, extending through subdural space and brain parenchyma. After meticulous debridement with saline with gentamicin and hydrogen peroxide, duroplasty and cranioplasty were replaced. Cultures from the abscess showed C. perfringens (susceptible to penicillin, amoxicillin, meropenem, clindamycin, metronidazole, ciprofloxacin) and Proteus mirabilis (susceptible to cephalosporins, aminoglucosydes, quinolones and carbapenems) with no fungal growth.
Broad spectrum antibiotics were administered in the post-operative period (meropenem 2gr/8h and clindamycin 600 mg/8h during 4 weeks). The patient recovered slowly and favourably, with normalization of laboratory tests and afebrile after stopping the antibiotics. At discharge, 6 weeks after the intervention, he was able to obey commands and sustain a simple conversation, without motor deficits (GOS 3).
Discussion
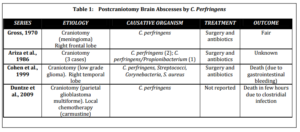
C. perfringens is a large, nonmotile, Gram-positive and spore-forming bacillus that is ubiquitous in the environment (Tekkok et al., 1996) and it is also part of the normal flora of the human bowel and genital tract (Colen et al., 2007). It is the most common cause of the gas gangrene, one of the most fulminant infections in humans, and it is detected in 60 to 90% of cases of Clostridial myonecrosis (Colen et al., 2007). It is not very common in neurosurgery (Duntze et al., 2009); nonetheless, more than 50% of the gas-containing brain abscesses are attributable to C. perfringens, with approximately 40 cases reported in the literature (Colen et al., 2007). In their review, Colen et al. found that the vast majority of them (80%) are consequence of penetrating traumatic brain injury (Cohen et al., 1999), (Colen et al., 2007), (Tekkok et al., 1996), followed by middle ear infection and cancer. Surgery is a far less common risk factor and to authors’ knowledge, there are only 6 cases of postcraniotomy brain abscesses due to C. perfringens previously reported in the literature (Table 1) (Ariza et al., 1986), (Cohen et al., 1999), (Duntze et al., 2009), (Gross, 1970).
Ariza et al. reviewed the intracranial focal infections treated in the intensive care unit and reported 5 patients with abscesses after craniotomy. Three of them were caused by C. perfringens, with the association of Propionibacterium in one case. All of them were successfully treated with surgical excision and antibiotics (Ariza et al., 1986). Gross presents the case of a brain abscess due to C. perfringens after a right frontal craniotomy for a meningioma, with good results after surgery and antibiotics (Gross, 1970). Cohen et al. report a patient who underwent a temporal lobectomy for low grade glioma excision and worsened in the immediate post-operative period. The CT scan showed a gas-containing collection in the surgical field with significant surrounding edema and cultures were positive for C. perfringens, Corynebacterium, Staphylococcus and Streptococcus. After surgical debridement and broad spectrum antibiotics the patient recovered, but he developed severe gastrointestinal bleeding and died unexpectedly (Cohen et al., 1999). Duntze et al. present a patient operated on for a glioblastoma with local carmustine chemotherapy and who developed a brain abscess due to C. perfringens three weeks later. Progression was especially fulminant, leading to patient’s death in a few hours (Duntze et al., 2009). In the present case, the patient was admitted with evidence of wound infection, two months after the last surgery. His neurological condition worsened in few hours and urgent debridement had to be performed. Multiple surgeries, impossibility of dural closure or direct contamination should be considered as predisposing factors for infection.
The optimal treatment for brain abscesses caused by C. perfringens requires a high index of clinical suspicion and early diagnosis. After a craniotomy, the radiological finding of intracranial air requires differentiating between a gas-containing abscess cavity and a postoperative pneumocephalus (Cohen et al., 1999) or other gas-like images, such as craneoplasties. Urgent surgical intervention with radical debridement and drainage is the main component of the management of clostridial cerebral abscesses (Cohen et al., 1999), (Tekkok et al., 1996), followed by intensive antibiotic therapy. Hyperbaric oxygen therapy has been reported by several authors, without clear results (Cianci, 1994), (Keogh, 1973), (Stephens, 1996).
Antibiotics without surgical intervention were used in very few cases; one of the patient reported experienced complete recovery, but had hyperbaric oxygen therapy, and the other patient died (Colen et al, 2007).
Almost half of the cases (30-50%) of clostridial brain abscesses are polimycrobial, as it is in our case. Gram-negative bacilli, including Klebsiella, E. coli and Proteus, and less often, Gram positive, such as Staphylococcus andStreptococcus, are involved in the suppurative process (Cohen et al., 1999). Fungal association should be suspected when failure of antibiotic treatment and cultures should be retained for long periods (6 weeks) to confirm the diagnosis (Tekkok et al, 1996). Despite the seriousness of clostridial wound infections outside the central nervous system, it is surprising that brain abscesses caused by these organisms are not uniformly fatal, with a global death rate attributable toC. perfringens of 10 to 11% (Cohen et al., 1999), (Colen et al., 2007).
Conclusion
C. perfringens is the most frequently involved pathogen in gas-containing brain abscesses, and it should be included in the differential diagnosis of postcraniotomy infections with such features. Urgent surgical intervention and broad spectrum antibiotics are the most efficient treatment to achieve a good functional outcome.
References
Ariza, J., Casanova, A., et al. (1986). “Etiological Agent and Primary Source of Infection in 42 Cases of Focal Intracranial Suppuration,” Journal of Clinical Microbiology, 24 (5) 899-902.
Publisher – Google Scholar
Cianci, P. (1994). “Adjunctive Hyperbaric Oxygen Therapy in the Treatment of the Diabetic Foot,” Journal of American Podiatric Medical Association, 84 (9) 448-55.
Publisher – Google Scholar
Cohen, J. E., Mierez, R. & Tsai, E. C. (1999). “Postcraniotomy Gas-Containing Brain Abscess: A Neurosurgical Emergency. Case Report,” Surgical Neurology, 51 (5) 568-70.
Publisher – Google Scholar
Colen, C. B., Rayes, M., et al. (2007). “Outcome of Brain Abscess by Clostridium Perfringens,” Neurosurgery, 61 (6) E1339; discussion E1339.
Publisher – Google Scholar
Domingo, Z. (1994). “Clostridial Brain Abscesses,” British Journal of Neurosurgery, 8 (6) 691-4.
Publisher – Google Scholar
Duntze, J., Litre, C. F., et al. (2009). “Clostridial Brain Abscess after Glioblastoma Resection: Case Report and Critical Review of the Literature,” Neurochirurgie, 55 (6) 569-72.
Publisher – Google Scholar
Gross, S. W. (1970). “Clostridium Welchii Brain Abscess Following Craniotomy for Meningioma: A Case Report,” The Mount Sinai Journal of Medicine, 37 (1) 23-6.
Publisher – Google Scholar
Heineman, H. S. & Braude, A. I. (1963). “Anaerobic Infection of the Brain: Observations on Eighteen Consecutive Cases of Brain Abscess,” The American Journal of Medicine, 35 682-697.
Publisher – Google Scholar
Keogh, A. J. (1973). “Clostridial Brain Abscess and Hyperbaric Oxygen,” Postgraduate Medical Journal, 49 (567) 64-6.
Publisher – Google Scholar
Stephens, M. B. (1996). “Gas Gangrene: Potential for Hyperbaric Oxygen Therapy,” Postgraduate Medicine, 99(4) 217-224.
Publisher – Google Scholar
Tekkok, I. H., Higgins, M. J. & Ventureyra, E. C. G. (1996). “Posttraumatic Gas-Containing Brain Abscess Caused by Clostridium Perfringens with Unique Simultaneous Fungal Suppuration by Myceliophthora Thermophila: Case Report,”Neurosurgery, 39(6) 1247-51.
Publisher – Google Scholar