Introduction
The presence of the male gonad in a patient who appears outwardly as a female is a hallmark of testicular feminization, where peripheral target organs are resistant to androgens (Schindler 1978). We present a case with inguinal hernia including internal testis, which is thought to be an example of testicular feminization syndrome.
Case Report
A 62-year-old woman entered into emergency service with a mass in her right inguinal region complaining of pain. It was learned that she had no previous history of any palpable induration, or other things in her inguinal region, but there was swelling in her right inguinal region which became unbearably painful in the last 4 days. The patient suffered from gas and stool discharge during the first 2-3 days and vomited 4-5 times in the last day.
The patient’s vital signs were normal and stable. In the stomach examination, a right irreducible hernia was observed. The patient had guarding and tenderness on her stomach’s lower right quadrant and left hypoquadrant regions, whereas the left inguinal region was normal. An X-ray in standing position revealed 4-5 air-liquid levels belonging to the small intestine. After seeing oedematous small intestine segments, which became prolapsed from the right inguinal duct on superficial ultrasonography of the right inguinal region, herniorrhaphy under emergency conditions was planned for the patient. There was leucocytosis (WBC: 14.400 K/mm3) with a predominance of neutrophils according to the pathological findings in biochemical examinations.
Herniorrhaphy with the right inguinal incision was planned for the patient. When the hernia sac was opened, there was 10 cm of her small intestine segments strangulated in the sac; after its blood perfusion was sufficient and viable, it was reduced back inside abdomen. After reduction, a 1×1 cm mass was found to be stuck to the round ligament and hernia sac, and the mass was evaluated as reactive lymph node, excised, and sent for histopathological examination.
On day two after the operation, the patient had no postoperative problems and was discharged.
The patient was followed up every other day. The histology of mass was reported to be a testis, and after the patient was informed of this finding, she absconded from the follow-up clinic. Subsequent history revealed that the patient was completely unaware of the situation; she is married but has never menstruated and does not have children, but also she has never been conducted by any detailed examination about this issue. The patient was informed that she should undergo an examination for the accompanying gonad on her left side and have her karyotype analyzed, but she refused and did not come for her checkup and any further examination.
The patient is thought to be suffering from testicular feminization syndrome for several reasons. From a multidisciplinary perspective, she is completely feminine in terms of not only the size of her breasts, or having external female genitalia, but also because of her general proportional phenotype. Furthermore, she does not have pubic hair, she is amenorrheic and infertile, and lastly she had a testis in her right inguinal duct.
Discussion
The testicular feminization syndrome is a disorder arising from defects in androgen receptor functions and results in peripheral androgen resistance. The androgen receptor is encoded by a gene located on the X chromosome, in the Xq11-12 region. Despite the existence of the male XY karyotype, the syndrome is characterized by a female phenotype. Breast sizes are normal or sometimes bigger than normal sizes, and there is almost neither pubic nor axillary hair because of peripheral androgen nonresponse. Body proportion is no different from a karyotypic female. External genital structure is completely expressed in the phenotype, but internal genitalia ends with a smaller and blind vagina (Kim 2011, Schindler 1978). Sarpel and colleagues (2005) planned on implementing testicular feminization screening by using vaginal length measurements made on 207 girls who had inguinal hernia, and their results were found significant.
Moreover, in the internal genital structure of the uterus, the ovaries and fallopian tubes are often not observed; but instead, undescended testes were found in the abdominal cavity or labium majus (Kim 2011). Testicular feminization syndrome is observed in 1 out of 20.000 to 60.000 women in the general population and in between 0.8% and 2.4% of girls who have inguinal hernia (Schindler 1978, Sarpel 2005). Generally, it is diagnosed during examination because of the primary amenorrhea during puberty. These patients who are raised as girls by their families should be diagnosed with inguinal hernia at the earliest possible time.
Almost one-third of the patients have unilateral inguinal hernia, so diagnosis of 46XY structure is increasing as an early diagnosis possibility by karyotype study, when screening the internal genitalia in suspicious cases of female infants who have inguinal hernia (Viner 1997). After the diagnosis, the treatment should include a multidisciplinary approach including the radiologist, the endocrinologist, the gynaecologist, and the general and plastic surgeon in conjunction with the genetic counselor. At that juncture, the prophylactic gonadectomy procedure is especially important, even after puberty. This is because the existence of an undescended testis increases the risk of neoplastic transformation: the risk is 3,6% up to the age of 25 and 33% up to the age of 50 (Kim 2011).
When considered from this standpoint, our patient presents as a rare occurrence. When the literature is examined, patients who have surgery because of inguinal hernia, whereupon a testis is discovered, are almost always children or young patients (Arikan 2003, Papanastasopoulos 2009). In 2008, Costopoulos and colleagues diagnosed a patient (aged 31) with testicular tumor formation like that of the other patients found in the literature (Costopoulos 2008,Kim 2011). When evaluated from this perspective, our patient is the second only to the 67-year-old patient who was reported by Schindler and colleagues in 1978.
One of the problems is the late discovery. To avoid tumorigenesis, the surgeon who plans hernia renovation for girls who especially have inguinal hernia is faced with a great task. The most critical motion, which is necessary, is to put forward a round ligament during the operation, and if it cannot be put forward, a testicular feminization differential diagnosis should be kept in mind and the patient should be provided with internal genitalia screening and karyotype analysis if necessary (Hurme 2009). In case a patient refuses a detailed examination like our patient, and because being face to face with medicolegal problems is possible, providing necessary information and counseling is critically important (Berg 2007). In light of this case, we agree that testicular feminization should be considered in cases of finding a bulk in the inguinal canal at every age.
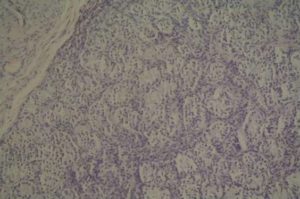
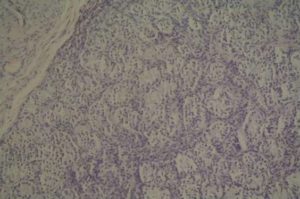
Figure 1: Seminiferous Tubules Coated by Sertoli Cells (H&E, X200)
References
Arikan, S., Yücel, A. F., Barut, G., et al. (2003). “Irreducible Inguinal Hernia, Bowel Obstruction, and Torsion of Testis in a Patient with Testicular Feminization Syndrome,” Hernia. 2003; 7(3):153-5. Epub 2003 Mar 20.
Publisher – Google Scholar
Berg, J. S., French, S. L., Mccullough, L. B., et al. (2007). “Ethical and Legal Implications of Genetic Testing in Androgen Insensitivity Syndrome,” J Pediatr. 2007; 150 (4):434-8.
Publisher – Google Scholar
Costopoulos, C., Ariyarathenam, A. V. & Bullock, N. (2008). “An Inguinal Hernia That Was Not Meant to Be: A Female with Seminoma,” Hernia. 2008; 12 (1):99-101. Epub 2007 Jul 10.
Publisher – Google Scholar
Hurme, T., Lahdes-Vasama, T., Makela E., et al. (2009). “Clinical Findings in Prepubertal Girls with Inguinal Hernia with Special Reference to the Diagnosis of Androgen Insensitivity Syndrome,” Scand J Urol Nephrol. 2009; 43 (1):42-6.
Publisher – Google Scholar
Kim, H. O., Kim, C. H, Kim, S. A., et al. (2011). “A Large Advanced Seminoma in an Older Woman with Androgen Insensitivity Syndrome,” Clin Exp Reprod Med. 2011; 38 (2):115-8. Epub 2011 Jun 30.
Publisher – Google Scholar
Papanastasopoulos, P., Panagidis, A., Verras, D., et al. (2009). “A Case of Complete Androgen Insensitivity Syndrome Presenting with Incarcerated Inguinal Hernia: An Immunohistochemical Study,” Fertil Steril. 2009; 92 (3):1169.E11-4. Epub 2009 Jun 21.
Publisher – Google Scholar
Sarpel, U., Palmer, S. K. & Dolgin, S. E. (2005). “The Incidence of Complete Androgen Insensitivity in Girls with Inguinal Hernias and Assessment of Screening by Vaginal Length Measurement,” J Pediatr Surg. 2005; 40 (1):133-6; Discussion 136-7.
Publisher – Google Scholar
Schindler, A. M. & Csank-Brassert, J. (1978). “Late Discovery of a Case of Testicular Feminisation,” J Med Genet. 1978; 15 (3):229-32.
Publisher – Google Scholar
Viner, R. M., Teoh, Y., Williams, D. M., et al. (1997). “Androgen Insensitivity Syndrome: A Survey of Diagnostic Procedures and Management in the UK,” Arch Dis Child. 1997; 77 (4):305-9.
Publisher – Google Scholar