Discussion
Lipogranuloma is a granulomatous soft tissue reaction which involves either lipid or oil deposits and typically manifests clinically as subcutaneous nodules or rubbery lymphadenopathy. While rare, lipogranuloma is most commonly documented in the urologic literature, as the most common site is the genitals of young adults secondary to the injection of foreign materials for penile augmentation, as described by Hohaus (2003). Few reports exist in the literature which describe lipogranuloma of the head and neck. Bassichis (2003) described a lipogranuloma of the nasal sidewall 1 year status-post rhinoplasty thought to be secondary to postoperative nasal packing impregnated with petroleum ointment. Similarly, Guo (2007) reported three cases of eyelid lipogranuloma after endoscopic sinus surgery (all developed within 1 month postoperatively) in patients who suffered medial orbital wall injury and had subsequent postoperative petroleum-based nasal packing. In all cases, definitive diagnosis and treatment occurred by surgical excision of the lesion in question.
The differential diagnosis for a neck mass is commonly quite broad. When considering the diagnosis of lipogranuloma, it is important to note that the majority of patients will have some element of history which relates to lipid deposition (injection, surgical, traumatic). Though one must also consider the possibility of lymphatic migration, as the original site of deposition may be in a different anatomic location from where the lipogranulomatous lymphadenopathy manifests. Lipogranuloma may be initially confused for malignancy, and FNA may be of limited benefit, as noted by Peoc’h (2000), where biopsy not only did not provide a diagnosis, but mimicked lymphoma. Significant axillary lymphadenopathy (silicone lymphadenopathy) has also been noted in the context of patients who have undergone silicone breast augmentation mammoplasty.
The pathophysiology of lipogranuloma has been described via two different mechanisms, exogenous and endogenous. Exogenous etiology occurs secondary to the body’s inability to metabolize exogenous oils in the tissue interstitium which subsequently results in a foreign body granulomatous reaction. Endogenous etiology elicits lipid degeneration from an allergic/inflammatory mechanism as a result of severe heat/cold and/or trauma. Lipogranuloma via endogenous etiology is noted to be a more rare occurrence.
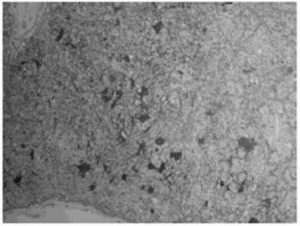
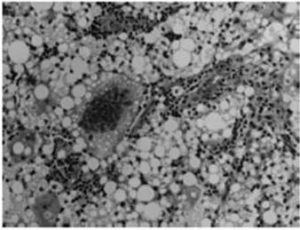
Lipogranulomatous lymphadenopathy specifically refers to the presence of endogenous lipid material within a lymph node. Hausner (1982) described lipogranulomatous lymphadenopathy, where the lipid material is typically present in both the extracellular space as well as within histiocytes, which in turn confers a vacuolated or foamy appearance to the cell. Lipid material is identified histologically based on a characteristic round, empty, droplet appearance with marked variation in size of individual droplets (FIGURE 1 & 2). Special stains for lipid, such as Oil-red-O, can be performed for confirmation.
The main differential diagnosis for this patient with lipogranulomatous lymphadenopathy, particularly in the context of a history of silicone breast augmentation mammoplasty, is silicone lymphadenopathy. After breast implant rupture, migration of silicone gel to draining lymph nodes may occur. Although silicone lymphadenopathy may be associated with chronic granulomatous inflammation, including the presence of multinucleated giant cells, it differs from lipogranulomatous lymphadenopathy in that silicone lymphadenopathy is characterized by the presence of multinucleated foreign body- type giant cells in association with and often containing refractive particles of foreign material. In this case, not only was the ruptured implant on the contralateral side, but no foreign material was identified histologically, thus ruling out silicone lymphadenopathy secondary to implant rupture. As a result, endogenous etiology for lipogranuloma formation secondary to lipid degeneration is supported given the patient history of neck trauma (motor vehicle accident).
Lipogranulomatous lymphadenopathy is a rare clinical entity, particularly in the head and neck and should be considered in the differential diagnosis of neck mass. Our aim is that this report may be useful for both otolaryngologists and health care practitioners when faced with a neck mass with complex clinical history.
References
Bassichis, B. A. & Thomas, J. R. (2003). “Foreign Body Inclusion Cyst Presenting on the Lateral Nasal Sidewall 1 Year after Rhinoplasty,” Arch Facial Plast Surg, 5(6):530-532.
Publisher – Google Scholar
Guo, Y., Peng, A., Xie, D., Li, Y., Ren, J., Xiao, M., Fan, S., Yang, X., Wu, W. & Xie, D. (2007). “Diagnosis and Management of Lipogranuloma of the Eyelids from Nasal Endoscopic Surgery,” (Article in Chinese), Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi, 21(8):340-343.
Publisher – Google Scholar
Hausner, R. J., Schoen, F. J., Mendez-Fernandez, M. A., Henly, W. S. & Geis, R. C. (1981). “Migration of Silicone Gel to Axillary Lymph Nodes after Prosthetic Mammoplasty,” Arch Pathol Lab Med, 105(7):371-372.
Publisher – Google Scholar
Hohaus, K., Bley, B., Köstler, E., Schonlebe, J. & Wollina, U. (2003). “Mineral Oil Granuloma of the Penis,” J Eur Acad Dermatol Venereol, 17:585—587.
Publisher – Google Scholar – British Library Direct
Peoc’h, M., Duprez, D., Grice, G., Fabre-Bocquentin, B., Gressin, R. & Pasquie, B. (2000) “Silicone Lymphadenopathy Mimicking a Lymphoma in a Patient with a Metatarsophalangeal Joint Prosthesis,” J Clin Pathol, 53(7):549-51.
Publisher – Google Scholar – British Library Direct