Introduction
Idiopathic sudden sensorineural hearing loss (ISSHL) is an intriguing condition that has been in the centre of otologic research for several decades. Over the years, a large number of therapies have been proposed. During the last 30 years, systemic steroids have been gaining ground. They are currently the most widely used form of treatment for ISSHL although the evidence that supports their use is not undisputed (Wei et al., 2006 and Conlin and Parnes, 2007). As a result, patient education and shared decision making are very important when deciding for a treatment plan (Stachler et al., 2012). One of the key factors that helped the increasing acceptance of steroids as a treatment for ISSHL is the fact that they lack frequent side effects. Of course, the infrequency of side effects does not equal nonexistence, especially in certain groups of patients such as diabetics. This is one of the reasons why during the last 15 years the intratympanic route of steroid administration for ISSHL has become so popular: it lacks systemic side effects and allows greater steroid concentrations in the inner ear when compared with systemic administration (Chandrasekhar, 2001 and Parnes et al., 1999). Intratympanic (IT) steroids have been used as a monotherapy (Kakehata et al., 2006), as a combination therapy with systemic steroids (Battaglia et al., 2008), and most commonly as a salvage therapy after failure of systemic steroids (Plontke et al., 2009). We present a case of a diabetic patient with severe ISSHL in whom IT Dexamethasone was used as a salvage treatment.
Presentation of Case
A 59-year-old man presented with sudden hearing loss in his left ear, which occurred one week before presentation. It was his first episode. He reported no vertigo, otalgia, ear fullness, tinnitus or neurological symptoms. There was no history consistent with barotrauma and no history of head trauma, recent acoustic trauma, or upper respiratory tract infection. His medical history included type II diabetes mellitus (DM) treated with per os antidiabetics. Head and neck, otologic and neurotologic examinations were unremarkable except for hearing loss in the left ear. Pure tone audiometry showed a severe sensorineural hearing loss in the left ear with a 3-tone (0.5, 1 and 2 KHz) pure tone average (PTA) of 80 dB.
The patient was admitted to the otolaryngology-head and neck surgery department and treated with intravenous (iv) methylprednosolone (daily dose of 120 mg) for 10 days with tapering over the last two days. Glycemic control was achieved with subcutaneous crystallic insulin (Actrapid). He was discharged after the treatment with no improvement in his hearing.
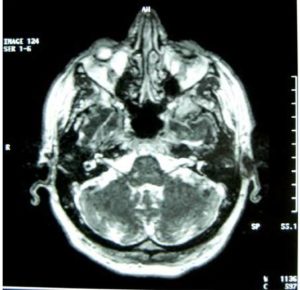
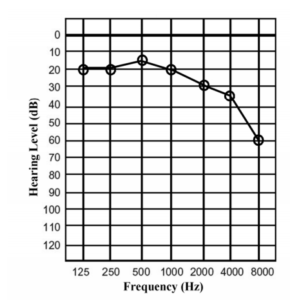
One week after his discharge (three and half weeks from the start of the hearing loss), the use of intratympanic steroids, which had been proposed unsuccessfully from the first day of his admission, was finally accepted by the patient and performed. In the meantime, a lesion in the cerebellopontine angle/internal auditory canal had been ruled out with MRI (Figure 1). A pure tone audiogram was done before the intervention and was essentially the same as at his admission. The intratympanic steroid injection was repeated three times over 8 days. With the patient lying in the right lateral position, 0.4 ml of Dexamethasone (8mg/2ml) was injected using a 27G spinal needle in the posteroinferior quadrant of the tympanic membrane after anesthesia with 5% Emla cream (lidocaine/prilocaine cream, AstraZeneca). No complications were noted. The improvement in hearing was more significant after the first two injections. The 3-tone PTA after conclusion of treatment was 27 dB and remained stable for the next three months. Subjectively, the patient reported full recovery of his hearing ability three, six, and twelve months after his treatment. His left ear audiogram after each step of treatment can be seen in Figure 2 while the audiogram of the right non-affected ear can be seen in Figure 3.
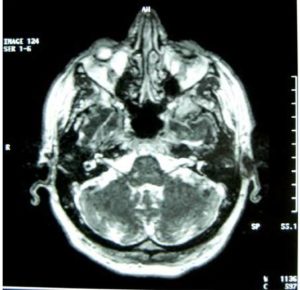
Figure 1: A Lesion in the Cerebellopontine Angle/Internal Auditory Canal was Ruled out with MRI

Figure 2: Pure Tone Audiometry (Left Ear)
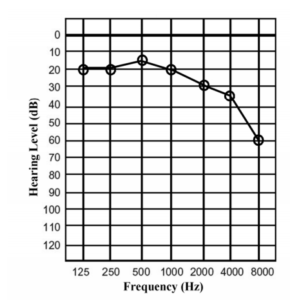
Figure 3: Pure Tone Audiometry (Right Non-Affected Ear)
Discussion
What was interesting in our case was the fact that a patient with severe ISSHL regained almost normal hearing 28 days after the onset of the disease and only after the initiation of intratympanic steroids. Bearing in mind that the natural history of this condition is largely unknown, there are still some interesting points to be made. Firstly, it is well accepted that the severity of the hearing loss is a negative prognostic and predictive factor for the final outcome with or without treatment (which was not the case in our patient) (Mattox and Simmons, 1977 and Byl, 1984). Secondly, the recovery in our patient began 25 days after the onset of the hearing loss. This is uncommon as it is accepted in the literature that the majority of patients with ISSHL recover within 2 weeks of the onset (Mattox and Lyles, 1989). Lastly, while there was no improvement with systemic steroids, the administration of IT Dexamethasone was accompanied by return to almost normal hearing after the second injection. This is in accordance with the results of Ho et al. (2004) who have used 3 injections of IT Dexamethasone on weekly intervals and found that hearing improvement was greater after the first two injections (Ho et al., 2004).
The other interesting point is that the patient presented in this case report had a known history of type 2 DM. The relationship between DM and ISSHL is a subject that remains controversial because of the lack of large epidemiological studies and the fact that the presence of DM has not been taken into consideration in the majority of the published work on the subject. Theoretically and taking into account the vascular theory explaining ISSHL, it is fair to assume that there should be an association between ISSHL and major cardiovascular risk factors such as DM. An epidemiologic survey in Japan has demonstrated an increase in the incidence and average age of ISSHL in the last 30 years, and this, according to the authors, may be partly associated with the increased prevalence of diseases such as DM. Furthermore, the prevalence of DM in elderly patients with ISSHL was found to be higher when compared with same age groups in the general population (Teranishi et al., 2007). Apart from that, there are certain retrospective studies which indicate that the degree of hearing loss is greater in patients with DM and ISSHL (Fukui et al., 2004). The evidence that correlates DM with hearing outcome after treatment of ISSHL is conflicting. Orita et al. (2007) in a retrospective study of 106 ISSHL patients, which included 8 hyperglycemic patients, found better hearing recoveries in the hyperglycemic patients (Orita et al., 2007). This finding is not supported by others who did not find a significant difference in the degree of recovery between diabetics and non-diabetics although the treatment schemes in these studies were different (Fukui et al., 2004). Lastly, an interesting study by Kakehata et al. (2006) has compared the efficacy of IT and systemic Dexamethasone in diabetic patients. It concluded that IT Dexamethasone is at least as effective as iv Dexamethasone and also devoid of the well-known systemic side effects of steroids including the difficulties in glycemic control that were encountered in 4 of the patients in the iv Dexamethasone group despite treatment with insulin (Kakehata et al., 2006).
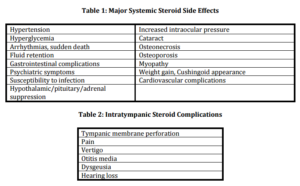
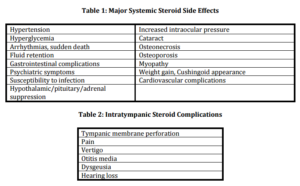
The main side effects of systemic steroids administration can be seen in Table 1. It should be noted that steroid toxicity is dependent on the dose and the duration of use although the exact threshold duration or dose for each side effect is not known (Huscher et al., 2009, Chrousos et al., 1993, and White et al., 1994). The reported adverse effects of short-term systemic steroid use on patients with ISSHL are rare. In Table 2, the reported so far complications of intratympanic steroid administration can be seen (Rauch et al., 2011). They are rare as well and dependent on the delivery method used.
Conclusion
Intratympanic steroids seem to be an excellent alternative to systemic steroids (Rauch et al., 2011). Particularly in patients who are suffering from DM, glaucoma, peptic ulcer, or uncontrollable hypertension, where the side effects of systemic steroids cannot be overlooked, this route of treatment should be considered seriously (Seggas et al., 2011). Further research is needed in the choice of drug, optimal method for intratympanic delivery, dosage requirements and efficacy. In any case, given the high spontaneous recovery rate of ISSHL, the unknown pathophysiology and the fact that most treatment schemes are based on conflicting evidence, the physician should have in mind the maxim “Primum non nocere” when confronting a patient with this condition.
References
Battaglia, A., Burchette, R. & Cueva, R. (2008). “Combination Therapy (Intratympanic Dexamethasone + High-Dose Prednisone Taper) For the Treatment of Idiopathic Sudden Sensorineural Hearing Loss,” Otology & Neurotology, 29, 453-60.
Publisher – Google Scholar
Byl, F. M., Jr. (1984). “Sudden Hearing Loss: Eight Years’ Experience and Suggested Prognostic Table,” The Laryngoscope, 94, 647-61.
Publisher – Google Scholar
Chandrasekhar, S. S. (2001). “Intratympanic Dexamethasone for Sudden Sensorineural Hearing Loss: Clinical and Laboratory Evaluation,” Otology & Neurotology, 22, 18-23.
Publisher – Google Scholar
Chrousos, G. A., Kattah, J. C., Beck, R. W. & Cleary, P. A. (1993). “Side Effects of Glucocorticoid Treatment. Experience of the Optic Neuritis Treatment Trial,” JAMA, 269, 2110-2.
Publisher – Google Scholar
Conlin, A. E. & Parnes, L. S. (2007). “Treatment of Sudden Sensorineural Hearing Loss: Ii. A Meta-Analysis,” Archives of Otolaryngology Head & Neck Surgery, 133, 582-6.
Publisher – Google Scholar
Fukui, M., Kitagawa, Y., Nakamura, N., Kadono, M., Mogami, S., Ohnishi, M., Hirata, C., Ichio, N., Wada, K., Kishimoto, C., Okada, H., Miyata, H. & Yoshikawa, T. (2004). “Idiopathic Sudden Hearing Loss in Patients with Type 2 Diabetes,” Diabetes Research and Clinical Practice, 63, 205-11.
Publisher – Google Scholar
Ho, H. G., Lin, H. C., Shu, M. T., Yang, C. C. & Tsai, H. T. (2004). “Effectiveness of Intratympanic Dexamethasone Injection in Sudden-Deafness Patients as Salvage Treatment,” The Laryngoscope, 114, 1184-9.
Publisher – Google Scholar
Huscher, D., Thiele, K., Gromnica-Ihle, E., Hein, G., Demary, W., Dreher, R., Zink, A. & Buttgereit, F. (2009). “Dose-Related Patterns of Glucocorticoid-Induced Side Effects,” Annals of Rheumatic Diseases, 68, 1119-24.
Publisher – Google Scholar
Kakehata, S., Sasaki, A., Oji, K., Futai, K., Ota, S., Makinae, K. & Shinkawa, H. (2006). “Comparison of Intratympanic and Intravenous Dexamethasone Treatment on Sudden Sensorineural Hearing Loss with Diabetes,” Otology & Neurotology, 27, 604-8.
Publisher – Google Scholar
Mattox, D. E. & Lyles, C. A. (1989). “Idiopathic Sudden Sensorineural Hearing Loss,” American Journal of Otology, 10, 242-7.
Publisher – Google Scholar
Mattox, D. E. & Simmons, F. B. (1977). “Natural History of Sudden Sensorineural Hearing Loss,” The Annals of Otology Rhinology and Laryngology, 86, 463-80.
Publisher – Google Scholar
Orita, S., Fukushima, K., Orita, Y. & Nishizaki, K. (2007). “Sudden Hearing Impairment Combined with Diabetes Mellitus or Hyperlipidemia,” European Archives of Oto-Rhino-Laryngology, 264, 359-62.
Publisher – Google Scholar
Parnes, L. S., Sun, A. H. & Freeman, D. J. (1999). “Corticosteroid Pharmacokinetics in the Inner Ear Fluids: An Animal Study Followed by Clinical Application,” The Laryngoscope, 109, 1-17.
Publisher – Google Scholar
Plontke, S. K., Lowenheim, H., Mertens, J., Engel, C., Meisner, C., Weidner, A., Zimmermann, R., Preyer, S., Koitschev, A. & Zenner, H. P. (2009). “Randomized, Double Blind, Placebo Controlled Trial on the Safety and Efficacy of Continuous Intratympanic Dexamethasone Delivered Via a Round Window Catheter for Severe to Profound Sudden Idiopathic Sensorineural Hearing Loss after Failure of Systemic Therapy,” The Laryngoscope, 119, 359-69.
Publisher – Google Scholar
Rauch, S. D., Halpin, C. F., Antonelli, P. J., Babu, S., Carey, J. P., Gantz, B. J., Goebel, J. A., Hammerschlag, P. E., Harris, J. P., Isaacson, B., Lee, D., Linstrom, C. J., Parnes, L. S., Shi, H., Slattery, W. H., Telian, S. A., Vrabec, J. T. & Reda, D. J. (2011). “Oral vs Intratympanic Corticosteroid Therapy for Idiopathic Sudden Sensorineural Hearing Loss: A Randomized Trial,” JAMA, 305, 2071-9.
Publisher – Google Scholar
Seggas, I., Koltsidopoulos, P., Bibas, A., Tzonou, A. & Sismanis, A. (2011). “Intratympanic Steroid Therapy for Sudden Hearing Loss: A Review of the Literature,” Otology & Neurotology, 32, 29-35.
Publisher – Google Scholar
Stachler, R. J., Chandrasekhar, S. S., Archer, S. M., Rosenfeld, R. M., Schwartz, S. R., Barrs, D. M., Brown, S. R., Fife, T. D., Ford, P., Ganiats, T. G., Hollingsworth, D. B., Lewandowski, C. A., Montano, J. J., Saunders, J. E., Tucci, D. L., Valente, M., Warren, B. E., Yaremchuk, K. L. & Robertson, P. J. (2012). “Clinical Practice Guideline: Sudden Hearing Loss,” Otolaryngol Head and Neck Surgery, 146, S1-35.
Publisher – Google Scholar
Teranishi, M., Katayama, N., Uchida, Y., Tominaga, M. & Nakashima, T. (2007). “Thirty-Year Trends in Sudden Deafness from Four Nationwide Epidemiological Surveys in Japan,” Acta Oto-laryngologica, 127, 1259-65.
Publisher – Google Scholar
Wei, B. P., Mubiru, S. & O’leary, S. (2006). “Steroids for Idiopathic Sudden Sensorineural Hearing Loss,” The Cochrane Library, Cd003998.
Publisher – Google Scholar
White, K. P., Driscoll, M. S., Rothe, M. J. & Grant-Kels, J. M. (1994). “Severe Adverse Cardiovascular Effects of Pulse Steroid Therapy: Is Continuous Cardiac Monitoring Necessary?,” Journal of the American Academy of Dermatology, 30, 768-73.
Publisher – Google Scholar