Discussion
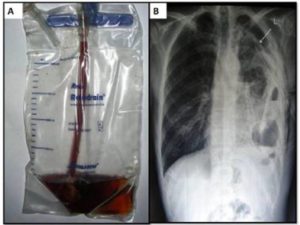
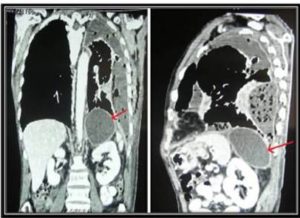
Spontaneous rupture of abdominal pseudopancreatic cyst into pleural cavity is extremely unusual complication of pancreatitis. The ruptured cyst passes either through the aortic or oesophageal hiatus or directly through diaphragm into pleural cavity leading to pancreaticopleural fistula (Tombroff et al, 1973). The enzyme-rich pleural fluid is due to disruption of the dorsal pancreatic ductal system (Traverso & Kozarek, 1999).Typically, the patients are middle-aged males(40—50 years) with chronic pancreatitis related mainly to alcohol abuse. As reported by Ali et al (2009) and King et al (2010), due to predominant pulmonary symptoms in form of cough and dyspnoea, the diagnosis is often delayed and the patients are usually worked up extensively for pulmonary pathology.Chest X-ray is the first line of investigation but it only gives information of pleural effusion. However majority of the cases give past history of recurrent attacks of pancreatitis and pleural fluid aspirate is characteristically haemorrhagic in appearance with very high amylase level.A CT scan of the chest and abdomen confirms the diagnosis.Ali et al (2009) and Megibow et al (2001) observed that endoscopic retrograde cholangiopancreatography (ERCP) and magnetic resonance cholangiopancreatography (MRCP) are useful diagnostic modalities in delineating pancreatic ductal anatomy and in localizing the site of leak before operative intervention.
Regarding treatment of such cases, Ali et al (2009) and King et al (2010) suggested that in acute cases presenting with respiratory distress due to massive pleural effusion, urgent thoracocentasis/tube thoracostomy should be done. It helps in relief of symptoms and encourages apposition of serosal surfaces. Medical management with octreotide significantly reduces fistula output and decreases the time to fistula closure. If fistula persists despite conservative treatment, ERCP, sphincterotomy and stent placement will decompress the duct and helps in fistula closure. In resistant cases, surgical intervention in form of distal pancreatectomy or Roux-en-Y pancreaticojejunostomy at the site of leak may be required.
References
Ali, T., Srinivasan, N., Le, V., Chimpiri, A. R. & Tierney, W. M. (2009). “Pancreaticopleural Fistula,” Pancreas, 38:e26—31.
Publisher – Google Scholar
King, J. C., Reber, H. A., Shiraga, S. & Hines, O. J. (2010). “Pancreatic-Pleural Fistula is Best Managed by Early Operative Intervention,” Surgery, 147:154—59.
Publisher – Google Scholar
Maringhini, A., Ciambra, M., Patti, R., Randazzo, M. A., Dardanoni, G., Mancuso, L., Termini, A. & Pagliaro, L. (1996). “Ascites, Pleural, and Pericardial Effusions in Acute Pancreatitis. A Prospective Study of Incidence, Natural History, and Prognostic Role,” Dig Dis Sci, 41(5): 848-52.
Publisher – Google Scholar – British Library Direct
Megibow, A. J., Lavelle, M. T. & Rofsky, N. M. (2001). “MR Imaging of the Pancreas,” Surg Clin North Am, 81: 307—20.
Publisher – Google Scholar – British Library Direct
Tombroff, M., Loicq, A., de Koster, J.- P., Engleholm, L. & Govaerts, J.- P. (1973). “Pleural Effusion with Pancreatico-Pleural Fistula,” Br Med J, i: 330—1.
Publisher – Google Scholar
Traverso, L. W. & Kozarek, R. A. (1999). “Interventional Management of Pancreatic Fluid Collections,” Surg Clin North Am, 79: 745—57.
Publisher – Google Scholar – British Library Direct