Introduction
Hydatidosis is a parasitic disease caused mostly by Echinococcus granulosis in human and many other mammals. It is characterized by a worldwide spread but is endemic mainly around the Mediterranean Sea (Fernández-Ruiz, M., 2008). The liver followed by the lung are the most common sites of the disease (Arikanoglu, Z., 2012). However, other sites such as the heart and spleen are rarely affected. Primary and isolated involvement of the spleen is unusual. It has an incidence of 0.5 – 4%. The rarity of splenic hydatid disease may pose a diagnostic challenge for clinicians, especially in non endemic areas (Fernández-Ruiz, M., 2008). Herein we report the case of a 65-year-old female presenting with moderate fever and heaviness in the left upper abdomen and found to have isolated splenic hydatidosis.
Case Presentation
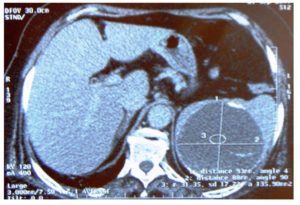
A 65-year-old female resident of Jemmel (Monastir – Tunisia) was presented with five months history of moderate fever and gradual increasing sensation of heaviness in her left hypochondrium. Patient complained of malaise with nausea, vomiting and intermittent fever since 2 months. There was no history of dyspepsia, or weight loss or other complaints. Physical examination was unremarkable except for the presence of a palpable painless tip of spleen. There was no hepatomegaly or lymphadenopathy. Chest, cardiovascular, central nervous, and the musculoskeletal systems were normal on examination. Ultrasonographic examination of the abdomen revealed an enlarged spleen (13 cm) with well encapsulated cystic lesion measuring 9 cm x 7 cm. The contrast enhanced computed tomography (CT) scan revealed splenomegaly (14 cm) with well defined homogenous hypodense lesion with an enhancing capsule measuring 93 mm x 88 mm in size (Figure). The liver and other abdominal organs and the chest were not involved.
White blood cells count was 5400/mm3 and C- reactive protein level was normal. Renal function test, liver function test and electrolytes revealed no abnormalities. Blood cultures were negatives. IgM Ecchinococcus antibodies were positives. A diagnosis of primary splenic hydatidosis was retained. Oral albendazole therapy was applied one month before surgery at 10 mg/kg/day in two divided doses. Then splenectomy was performed. Histopathological examination of the spleen confirmed the diagnosis of hydatidosis since there was acellular fibrous wall cyst with germinal layer and scolices in the center. Postoperatively, the patient continued on oral albendazole for 6 months without any side effects. One year later, the patient remains symptom free and no long-term complications were observed during the follow-up.
Discussion
Hydatic disease is common in areas where sheep and cattle rearing are important, particularly in Tunisia. It is a zoonotic infection caused by the tapeworm of the genus Echinococcus (Hariqbal, S., 2003). The most common form is cystic hydatid disease, that is caused by Echinococcus granulosus, whereas the alveolar type is caused by E. multilocularis (Ibrahim, A., 2011). The primary hosts are the members of the canidae family, usually dogs, wolves and coyotes. The life cycle of this worm may also involve other animals called intermediate hosts and are infected via the ingestion of eggs shed in the feces of infected animals (Hariqbal, S., 2003). Humans are accidental intermediate hosts that become infected by handling soil, dirt or animal hair containing parasite eggs. Hydatidosis most commonly affects the liver and the lungs (Fernández-Ruiz, M., 2008). Primary and isolated involvement of spleen, as in our case, is rare. It has a frequency of 0.5 – 4% within abdominal hydatid disease (Fernández-Ruiz, M., 2008). Splenic hydatid cysts are generally asymptomatic. Diagnosis is usually made accidentally for unrelated complaints. When the cyst grows in size, it gives painful mass in the left upper abdomen. Other clinical presentations are possible like renal arterial compression and systemic hypertension or rupture of the splenic hydatid cyst to the other organs (Pukar, M.M., 2013). Our patient was admitted to hospital for sensation of heaviness in her left hypochondrium. The diagnosis is suspected when a cystic lesion is seen in abdominal ultrasonography. The differential diagnosis for splenic hydatid cysts includes epidermoid cysts, cystic hemangiomas or lymphangiomas, splenic abscesses or hematoma (Fernández-Ruiz, M., 2008). Specific laboratory tests using different serological reactions; indirect hemagglutination, complement fixation, and indirect immunofluorescence are useful for diagnosis. Immunoelectrophoresis highlights the specific arc 5 of hydatidosis, giving no cross-reaction with other helminths but negative serology does not exclude hydatid disease (Krassimira, K., 2006). The treatment of the splenic hydatid is debated. Certain authors recommend total splenectomy while others are in favour of conservative surgery. The surgical technique depends on data of imaging and the association with other locations (Rauf Ahmad Wani et al., 2005). If, surgical excision of the cyst remains the cornerstone of curative treatment; nevertheless, good results have been reported with chemotherapy based on albendazole (Usharani, A et al., 2013). Medical treatment is indicated in cysts inaccessible for surgical removal or as a complementary therapy to reduce recurrence. Preoperative administration of anthelmintics sterilizes and softens the cysts, reduces intracystic pressures providing more safety in surgical removal of cysts. According to the WHO guidelines, preoperative administration should begin between 1 month and 4 days before surgery for albendazole and 3 months before surgery for mebendazole (Arikanoglu, Z et al., 2012). WHO also recommends albendazole after surgery to reduce the risk of preoperative dissemination of hydatic scolices. In our case, albendazole therapy was taken before and after surgery with good outcomes and with no recurrence through the period of follow-up.
Conclusion
Primary splenic hydatid cyst is a rare clinical condition which must be considered in the differential diagnosis of a cystic lesion of spleen in endemic areas like Tunisia. Owing to the potential risk of threatening complications, surgery should be advised to the patient.
References
1.Arikanoglu, Z., Taskesen F, Gumus H and al (2012). ” Selecting a surgical modality to treat a splenic hydatid cyst: total splenectomy or spleen-saving surgery?,”J Gastrointest Surg, 16 (6), 1189-93.
Publisher– Google Scholar
2. Fernández-Ruiz, M., Juan-Manuel Guerra-Vales, Ana-Belén Enguita-Valls, Juan Vila-Santos, Francisco-Javier García-Borda, Carlos Morales-Gutiérrez (2008). ”Splenic hydatid cyst, a rare location of extrahepatic echinococcis : Report of six cases,” European Journal of Internal Medicine, 19 (7), 51-53.
Publisher
3. Hariqbal, S., Sumeet Arora. (2003). “Primary hydatid cyst of spleen,”Medical Journal Armed Forces India, 59 (2), 169-170.
Publisher
4. Ibrahim, A., Fatih Akbıyık, Aysegul Altunkeser. (2011). “Laparoscopic cystectomy for splenic hydatid cyst,” Journal of Pediatric Surgery, 46 (11), 1-3.
Publisher – Google Scholar
5. Krassimira, K., Penka Stefanova, Mira Bosheva. (2006).”Surgery in children with hydatid disease of the spleen,” Journal of Pediatric Surgery, 4 (7), 1264-1266.
6. Pukar, M.M., Shabari M. Pukar (2013). “Giant solitary hydatid cyst of spleen — A case report,”
7. International Journal of Surgery Case Reports, 4 (4), 435-437.
8. Rauf Ahmad Wani, Ajaz A. Malik, Nisar A. Chowdri, Khurshid A. Wani, Sameer H. Naqash (2005). “Primary extrahepatic abdominal hydatidosis,” International Journal of Surgery, 3 (2), 125-127.
Publisher – Google Scholar
9. Usharani, A., Deepica. G, Aruna. S, Kulkarni. S, Sai Kamal Kumar. G, Balamuralikrishna P. (2013).”Cases report of hydatid cyst,”Journal of Epidemiology and Global Health, 3 (2), 63-66.
Publisher