Afonso, P. V., Ozden, S., Cumont, M.- C., Seilhean, D., Cartier, L., Payam, R., Mason, S., Lambert, S., Huerre, M., Gessain, A. et al. (2008). “Alteration of Blood-Brain Barrier Integrity by Retroviral Infection,” PloS Pathogens, 4: 1-11.
Publisher – Google Scholar
Afonso, P. V., Ozden, S., Prevost, M. C., Schmitt, C., Seilhean, D., Weksler, B., Couraud, P. O., Gessain, A., Romero, I. A. & Ceccaldi, P. E. (2007). “Human Blood-Brain Barrier Disruption by Retroviral-Infected Lymphocytes: Role of Myosin Light Chain Kinase in Endothelial Tight-Junction Disorganization,” The Journal of Immunology, 179; 2576-2583.
Publisher – Google Scholar
Alberti, C., Cartier, L., Valenzuela, M., Puente, J., Tanaka, Y. & Ramirez, E. (2011). “Molecular and Clinical Effects of Betamethasone in Human T-cell Lymphotropic Virus Type-I-Associated Myelopathy/Tropical Spastic Paraparesis Patients,” Journal of Medical Virology 83:1641-9.
Publisher – Google Scholar
Cartier, L., Castillo, J. L., Cabrera, M. E., Araya, F., Matutes, E., Ford, A. M. & Greaves, M. F. (1995/b). “HTLV-I Positive Progressive Spastic Paraparesis (TSP) Associated with a Lymphoid Disorder in Three Chilean Patients,” Leukemia and Lymphoma, 17: 459-464.
Publisher – Google Scholar
Cartier, L., Castillo, J. L., Cea, J. G. & Villagra, R. (1995/a). ‘Chronic Dacrosyalpadenitis in HTLV-l Associated Myelopathy,’ Journal of Neurology, Neurosurgery & Psychiatry, 58: 244-246.
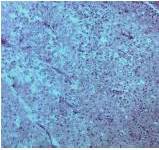
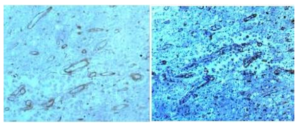
Cartier, L., Cea, J. G., Vergara, C., Araya, F. & Born, P. (1997). “Clinical and Neuropathological Study of Six Patients with Spastic Paraparesis Associated with HTLV-I an Axomyelinic Degeneration of the Centralnervous System,” Journal of Neuropathology & Experimental Neurology, 56:403—413.
Publisher – Google Scholar
Cartier, L.,Vergara, C. & Valenzuela, M. A. (2007). “Inmunohistoquímica de Los Cambios Degenerativos del Sistema Nervioso Central en Paraparesias Espásticas Asociadas al Virus Linfotrópico Humano T Tipo I (HTLV-I),” Revista Médica de Chile,135: 1139-1146.
Publisher – Google Scholar
Castillo, J. L., Cea, J. G., Verdugo, R. J. & Cartier, L. (1999). “Sensory Dysfunction in HTLV-I Associated Myelopathy/Tropical Spastic Paraparesis (HAM/TSP): A Comprehensive Neurophysiologic Study,” European Neurology42:17-22.
Publisher – Google Scholar
Gessain, A., Barin, F., Vernant, J. C., Gout, O., Calender, A. & De The G. (1985). ‘Antibodies to Human T-lymphotropic Virus in Patients with Tropical Spastic Paraparesis,’ Lancet, U:407-410.
Ijichi, T., Miyata, K., Mori, S., Nakajima, K., Okanoue,T. & Tsuchihashi, Y. (1993). “Asymptomatic Primary Biliary Cirrhosis in HTLV-l Associated Myelopathy,” The American Journal of Gastroenterology, 88; 2107-2109
Publisher
Jairus, S., Paul, F., Franciotta, D., Waters, P., Zipp, F., Hohlfeld, R., Vincent, A. & Wildemann, B. (2008). “Mechanisms of Disease: Aquaporin-4 Antibodies in Neuromyelitisóptica,” Nature Clinical Practice Neurology, 4: 202-214
Publisher
Nakagawa, M., Izumo, S., Ijichi, S., Kubota, H., Arimura, K., Kawabata, M.& Osame, M. (1995). “HTLV-I-Associated Myelopathy: Analysis of 213 Patients Based on Clinical Features and Laboratory Findings,” Journal of Neurovirology, 1:50—61.
Publisher – Google Scholar
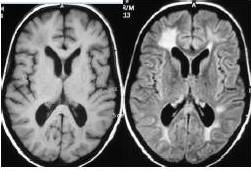
Ogata, A., Nagashima, K., Tashiro, K., Miyakawa, A. & Mikuni, C. (1993). “MRI Pathological Correlate of Brain Lesions in a Necropsy Case of HTLV-I Associated Myelopathy,” Journal of Neurology, Neurosurgery & Psychiatry, 56:194-196.
Publisher – Google Scholar
Osame, M., Matsumoto, M., Usuku, K., Izumo, S., Ijichi, N., Amitani, H., Tara, M. & Igata, A. (1987). “Chronic Progressive Myelopathy Associated with Elevated Antibodies to Human T-Lymphotropic Virus Type I and Adult T-cell Leukemia-Like Cells,” Annals of Neurology 21: 117-122
Publisher – Google Scholar
Schachter, D., Cartier, L. & Borzutzky, A. (2003). “Osteoporosis in HTLV-I Associated Myelopathy/Tropical Spastic Paraparesis (TSP/HAM),” Bone, 33: 192-96
Publisher – Google Scholar
Shakudo, M., Inoue, Y. & Tsutada, T. (1999). “HTLV-I-Associated Myelopathy: Acute Progression and Atypical MRI Findings,” American Journal of Neuroradiology, 20: 1417-1421.
Publisher
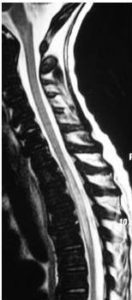
Tajima, Y., Kishimoto, R., Sudoh, K., Matsumoto, A., Miyazaki, Y., Kikuchi, S. et al. (2003). “Spinal Magnetic Resonance Image Alterations in Human T Lymphotropic Virus Type I-Associated Myelopathy Patients before and after Immunomodulating Treatments,” Journal of Neurology, 250: 750—753
Publisher – Google Scholar
Watanabe, M., Yamashita, T., Hara, A. et al. (2001). “High Signal in the Spinal Cord on T2-Weighted Images in Rapidly Progressive Tropical Spastic Paraparesis,” Neuroradiology 231-233
Publisher – Google Scholar
Yukitake, M., Takase, Y., Nanri, Y., Kosugi, M., Eriguchi, M., Yakushiji, Y., Okada, R., Mizuta, H. & Kuroda, Y. (2008). “Incidence and Clinical Significances of Human T-cell Lymphotropic Virus Type I-Associated Myelopathy with T2 Hyperintensity on Spinal Magnetic Resonance Images,” Internal Medicine 47: 1881-1886.
Publisher – Google Scholar