Signs of the compartment syndrome disappeared completely during the following two days after fasciotomy, but at this time weakness of the quadriceps muscle was noted. Analysis by the neurologist revealed a paralysis of the quadriceps muscle. There were no signs of altered skin sensibility. Ultrasonography of the groin excluded the presence of a local hematoma and no signs of compression of the neurovascular structures in the groin were seen. Electromyography performed 2 weeks later revealed a lesion of the femoral nerve with only minimal spontaneous recovery in the vastus lateralis muscle. The patient stayed admitted. Six weeks after initial surgery, patient complained of a painful, swollen knee. Punction of the knee revealed a new haemarthrosis and three days later it was decided to debride the knee arthroscopically because of persistent pain. This procedure was performed under general anaesthesia and again no tourniquet was used. Blood thrombi were evacuated from the knee joint. There were no signs of impingement or proliferative synovitis. Anticoagulant therapy was stopped at this time. No new episodes of bleeding occurred after this intervention. Analysis for coagulation disorders was performed but no abnormalities could be detected. Two weeks later, a new elektromyography was performed to re-evaluate the femoral nerve paralysis. No signs of recovery could be observed at this stage and prognosis was uncertain.
The patient was eventually discharged two days later, nearly 2 months after initial surgery and she was registered for intensive rehabilitation. Seven months after the initial surgery, weakness of the quadriceps muscle was still remarkable. A new electromyography showed a normal conduction in the femoral nerve and signs of reinnervation of the quadriceps muscle. No haemarthros developed since the day of discharge. Flexion of the knee was only 45 degrees and a 5 degree extension deficit remained. At this moment patient was bound to a wheelchair for most of the time. At 10 months post-surgery, residual weakness of the quadriceps muscle was limited and knee function had improved to 70 degrees of flexion and a 5 degree extension deficit.
Discussion
Signs and symptoms of compartment syndrome include: pain out of proportion to the injury and worsening of the pain with passive stretching of the involved muscles, swelling and coldness. Late signs are paraesthesia, pulselessness and paralysis, although the presence of a pulse cannot rule out the presence of compartment syndrome (Sloper et al., 2003). Compartment syndrome complicating knee arthroscopy is documented (Kim et al., 2002, Mont et al., 1996), but it is only rare after total joint replacement and a specific cause in these cases cannot always be identified (Hailer et al., 2007). Some reports are published on compartment syndrome after TKA. Tang and Chiu were the first to describe occurrence of compartment syndrome of the calf after early postoperative dislocation of a TKA (Tang and Chiu, 2000). Haggis et al. reported on 7 cases of compartment syndrome following TKA and identified risk factors for the development of a compartment syndrome (Haggis et al., 2006). These factors include: soft-tissue compromise, often related to previous surgery, injury or complex surgery and vascular compromise or intra-operative vascular injury. In our case, no such risk factors were present. The compartment syndrome was the result of bleeding from a knee joint cyst. This has been reported previously to be one of the causes of compartment syndrome (Haggis et al., 2006). Bleeding did not occur directly in the anterior compartment, but compression of this compartment was probably indirect due to a haematoma in the flexor compartment with subsequent spontaneous compression of the popliteal vein. We did not perform pressure measurements but other causes for peroneal nerve involvement were unlikely because of normal peroneal nerve function directly postoperative and the absence of sonographic abnormalities.
An overall incidence of temporary femoral nerve injury of 0.6% has been reported after fermoral catheter placement with the use of electrical stimulation guidance (Feibel et al., 2009). Incidence of permanent neurologic injury, as manifested by weak quadriceps power, diminished sensation, and dysesthesia, is estimated to be 0.2% (Feibel et al., 2009). Femoral neuropathy can be caused by iliacus hematoma and is a well-known complication in hemophiliacs or in patients undergoing anticoagulant therapy (Puechal et al., 1992, Rodriguez-Merchan, 2012). In patients without coagulation disturbances, however, femoral neuropathy caused by iliacus hematoma rarely occurs, the cause is usually traumatism instead (Puechal et al., 1992). Concerning these traumatisms, it is hypothesised that the potential for coiling of the perineural catheter and pressure injury to the nerve, rather than intraneural puncture, pertains a risk of neurologic injury (Feibel et al., 2009). A similar trauma mechanism to the femoral nerve has probably taken place in our case, where a pulling force had been exerted onto the catheter with secondary movement of the catheter in the neural sheet. From this moment on, patient reported a sharp pain, every time fluid was injected into the catheter. Pain or paresthesias on injection of local anesthetics in patients who had nerve damage have been observed by others (Auroy et al., 1997, Auroy et al., 2002). It is possible that these injections have further aggravated the damage to the femoral nerve by increasing intraneural pressure.
Nerve palsy can be a complication of tourniquet use and a total tourniquet time of more than 120 minutes is a significant risk factor for the development of peroneal nerve palsies. There are, as far as we know, no femoral nerve laesions reported in current literature that were the result of long tourniquet time. Given the absence of these reports, the obvious trauma exerted onto the catheter in our case and a tourniquet time of only 20 minutes, it is unlikely that the use of a tourniquet has played a role in the pathogenesis of the femoral nerve injury in our case. Time to neurologic recovery of a femoral nerve lesion ranges from 36 hours to 6 months (Feibel et al., 2009, Capdevila et al., 2005). In our case, at 7-month follow-up, clinical weakness of the quadriceps muscle persisted, but EMG showed evidence of reinnervation (fasciculation potentials). The long-term prognosis therefore seems favourable.
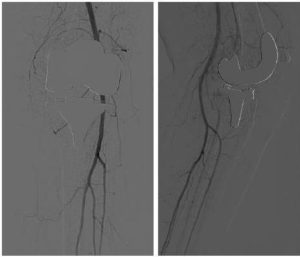
Several causes for recurrent haemarthrosis have been pointed out. Early bleeding is mostly due to direct vascular injury, arteriovenous fistula, arterial aneurysm and pseudoaneurysm (Saksena et al.). Furthermore, early bleeding may be the result of a loose tag of synovial tissue remaining from surgery that becomes entrapped between the moving components of the prosthesis early in the postoperative course (Kindsfater and Scott, 1995). It also can be the result of a platelet factor 3 availability defect (Malhotra et al., 2005). In our case, no such cause for recurrent bleeding could be identified. It has been stated previously that causes of haemarthrosis remain unclear in 35,8% of cases (Suzuki et al., 2006). Unexplained haemarthrosis after TKA, as was the case in our patient, should ideally be treated in stages (Rukavina et al.). In every case needle aspiration should be performed first for relief of pain and stiffness, followed by cooling, elevation, rest and discontinuing anticoagulants when possible (Ohdera et al., 2004). If conservative treatment is not successful a femoral arteriography should be considered with the possibility for immediate embolization of the source of bleeding. If embolization is unsuccessful, arthroscopy is the next step. Entrapped tissue and any source of bleeding can then be localized and treated. If this approach is unsuccessful an open synovectomy is indicated (Rukavina et al.). In our case, bleeding stopped after discontinuing anticoagulant therapy. However, this was only done at a later stage, after invasive therapies had already been performed. Theoretically, these invasive therapies could have been unnecessary in our case if anticoagulants were discontinued in an early phase. Moreover, the use of fondaparinux 5mg/ml on itself could have been an initiating factor for the bleeding episodes as it is stated that the risk of major bleeding (defined as fatal bleeding, bleeding involving a critical organ, bleeding leading to reoperation and overt bleeding with a bleeding index of ≥ 2) is significantly higher than with enoxaparin 30mg twice daily (Bauer et al., 2001, Turpie et al., 2002). Furthermore, a statistically significant relationship was reported between the incidence of major bleeding and the timing of the first fondaparinux injection between 3 and 9 hours post-surgery (Turpie et al., 2002). In our case, injection was administered 6 hours after surgery. Given these observations, the use of fondaparinux as anticoagulant therapy has therefore likely played a role in the pathogenesis of this bleeding complication.
Conclusion
Total knee arthroplasty is one of the most successful procedures with long survival and is perceived as a save procedure. In this case three very uncommon complications occurred together in one patient. We believe this case stresses the importance for orthopaedic surgeons to continuously and carefully monitor their patients postoperatively in order to adequately diagnose complications, also the rare ones, and to take appropriate measurements to minimize dramatic outcomes of these complications. Furthermore, we believe that careful and critical use of anticoagulants is mandatory for lowering the risk of postoperative bleeding complications in patients with TKA.
References
Auroy, Y., Benhamou, D., Bargues, L., Ecoffey, C., Falissard, B., Mercier, F. J., Bouaziz, H. & Samii, K. (2002). ”Major Complications of Regional Anesthesia in France: The SOS Regional Anesthesia Hotline Service,” Anesthesiology, 97 (5) 1274-1280.
Publisher – Google Scholar – British Library Direct
Auroy, Y., Narchi, P., Messiah, A., Litt, L., Rouvier, B. & Samii, K. (1997). ”Serious Complications Related to Regional Anesthesia: Results of a Prospective Survey in France,” Anesthesiology, 87 (3) 479-486.
Publisher – Google Scholar
Bauer, K. A., Eriksson, B. I., Lassen, M. R. & Turpie, A. G. G. (2001). ”Fondaparinux Compared with Enoxaparin for the Prevention of Venous Thromboembolism after Elective Major Knee Surgery,” The New England journal of medicine, 345 (18) 1305-1310.
Publisher – Google Scholar – British Library Direct
Capdevila, X., Pirat, P., Bringuier, S., Gaertner, E., Singelyn, F., Bernard, N., Choquet, O., Bouaziz, H. & Bonnet, F. (2005). ”Continuous Peripheral Nerve Blocks in Hospital Wards after Orthopedic Surgery: A Multicenter Prospective Analysis of the Quality of Postoperative Analgesia and Complications in 1,416 Patients,” Anesthesiology, 103 (5) 1035-1045.
Publisher – Google Scholar
Colwell, C. W. (2009). ”The ACCP Guidelines for Thromboprophylaxis in Total Hip and Knee Arthroplasty,” Orthopedics, 32 (12 Suppl) 67-73.
Publisher – Google Scholar
Feibel, R. J., Dervin, G. F., Kim, P. R. & Beaule, P. E. (2009). ”Major Complications Associated with Femoral Nerve Catheters for Knee Arthroplasty: A Word of Caution,” The Journal of Arthroplasty, 24 (6 Suppl) 132-137.
Publisher – Google Scholar
Geerts, W. H., Bergqvist, D., Pineo, G. F., Heit, J. A., Samama, C. M., Lassen, M. R. & Colwell, C. W. (2008). ‘Prevention of Venous Thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition),” Chest, 133 (6 Suppl) 381S-453S.
Google Scholar
Haggis, P., Yates, P., Blakeway, C., Fick, D., Morgan, D. A. F., Holt, M. & Wood, D. (2006). ”Compartment Syndrome Following Total Knee Arthroplasty: A Report of Seven Cases,” Journal of Bone and Joint Surgery Br, 88 (3) 331-334.
Publisher – Google Scholar – British Library Direct
Hailer, N. P., Adalberth, G. & Nilsson, O. S. (2007). ”Compartment Syndrome of the Calf Following Total Knee Arthroplasty–A Case Report of a Highly Unusual Complication,” Acta Orthopaedica, 78 (2) 293-295.
Publisher – Google Scholar – British Library Direct
Idusuyi, O. B. & Morrey, B. F. (1996). ”Peroneal Nerve Palsy after Total Knee Arthroplasty. Assessment of Predisposing and Prognostic Factors,” Journal of Bone and Joint Surgery Am, 78 (2) 177-184.
Publisher – Google Scholar – British Library Direct
Kim, T. K., Savino, R. M., McFarland, E. G. & Cosgarea, A. J. (2002). ”Neurovascular Complications of Knee Arthroscopy,” American Journal of Sports Medicine, 30 (4) 619-629.
Publisher – Google Scholar – British Library Direct
Kindsfater, K. & Scott, R. (1995). ”Recurrent Hemarthrosis after Total Knee Arthroplasty,” The Journal of Arthroplasty, 10 Suppl S52-55.
Publisher – Google Scholar – British Library Direct
Malhotra, R., Bhan, S. & Kiran, E. K. (2005). ”Haemarthroses after Total Knee Arthroplasty Caused by an Isolated Platelet Factor 3 Availability Defect,” Journal of Bone and Joint Surgery Br, 87 (11) 1549-1552.
Publisher – Google Scholar – British Library Direct
Mont, M. A., Dellon, A. L., Chen, F., Hungerford, M. W., Krackow, K. A. & Hungerford, D. S. (1996). ”The Operative Treatment of Peroneal Nerve Palsy,” Journal of Bone and Joint Surgery Am, 78 (6) 863-869.
Publisher – Google Scholar – British Library Direct
Ohdera, T., Tokunaga, M., Hiroshima, S., Yoshimoto, E. & Matsuda, S. (2004). ”Recurrent Hemarthrosis after Knee Joint Arthroplasty: Etiology and Treatment,” The Journal of Arthroplasty, 19 (2) 157-161.
Publisher – Google Scholar
Peel, T. N., Buising, K. L. & Choong, P. F. M. (2011). ”Prosthetic Joint Infection: Challenges of Diagnosis and Treatment,”ANZ Journal of Surgery, 81 (1-2) 32-39.
Publisher – Google Scholar
Puechal, X., Liote, F. & Kuntz, D. (1992). ”Bilateral Femoral Neuropathy Caused by Iliacus Hematomas during Anticoagulation after Cardiac Catheterization,” American Heart Journal, 123 (1) 262-263.
Publisher – Google Scholar
Pulido, L., Parvizi, J., Macgibeny, M., Sharkey, P. F., Purtill, J. J., Rothman, R. H. & Hozack, W. J. (2008). ”In Hospital Complications after Total Joint Arthroplasty,” The Journal of arthroplasty, 23 (6 Suppl 1) 139-145.
Publisher – Google Scholar
Ritter, M. A., Berend, M. E., Meding, J. B., Keating, E. M., Faris, P. M. & Crites, B. M. (2001). ”Long-Term Follow up of Anatomic Graduated Components Posterior Cruciate-Retaining Total Knee Replacement,” Clinical Orthopaedics and Related Research, (388) 51-57.
Publisher – Google Scholar – British Library Direct
Rodriguez-Merchan, E. C. (2012). ”Peripheral Nerve Injuries in Haemophilia,” Blood transfusion, 1-7.
Publisher – Google Scholar
Rukavina, A., Kerkhoffs, G. M. M. J., Schneider, P. & Kuster, M. S. (2010). ”Recurrent Hemarthrosis after Total Knee Arthroplasty,” Knee Surgery and Sports Traumatology Arthroscopy, 18 (7) 898-900.
Publisher – Google Scholar
Saksena, J., Platts, A. D. & Dowd, G. S. E. (2010). ”Recurrent Haemarthrosis Following Total Knee Replacement,” Knee, 17 (1) 7-14.
Publisher – Google Scholar
Sloper, P. J. H., Hing, C. B., Donell, S. T. & Glasgow, M. M. S. (2003). ”Intra-Operative Tibial Plateau Fracture during Unicompartmental Knee Replacement: A Case Report,” Knee, 10 (4) 367-369.
Publisher – Google Scholar
Suzuki, M., Kakizaki, J., Tsukeoka, T., Tsuneizumi, Y., Miyagi, J. & Moriya, H. (2006). ”A Case of Spontaneous Hemoarthrosis after a Total Knee Arthroplasty,” Modern Rheumatology, 16 (4) 248-250.
Publisher – Google Scholar – British Library Direct
Tang, W. M. & Chiu, K. Y. (2000). ”Silent Compartment Syndrome Complicating Total Knee Arthroplasty: Continuous Epidural Anesthesia Masked the Pain,” The Journal of Arthroplasty, 15 (2) 241-243.
Publisher – Google Scholar – British Library Direct
Turpie, A. G. G., Bauer, K. A., Eriksson, B. I. & Lassen, M. R. (2002). ”Fondaparinux vs Enoxaparin for the Prevention of Venous Thromboembolism in Major Orthopedic Surgery: A Meta-Analysis of 4 Randomized Double-Blind Studies,”Archives of internal medicine, 162 (16) 1833-1840.
Publisher – Google Scholar – British Library Direct