Introduction
Gastritis cystica profunda (GCP) is a rare submucosal benign gastric lesion. Its etiology is not clear, but the most important cause is prior gastric surgery. GCP can be mistaken for other gastric masses because it generally cannot be diagnosed preoperatively. There is no consensus on treatment of these lesions. Its surgeries range from simple submucosal excisions to total gastrectomies. As it is seen so rarely, we present this case to raise awareness of differential diagnoses of stomach wall masses.
Case Report
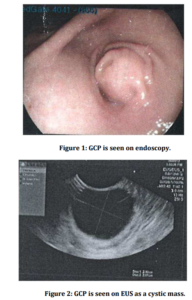
A 44-year-old female patient was admitted to hospital with complaints of abdominal pain, low back pain, bloating, and vomiting for eight months. On physical examination, there was no pathological finding in the abdomen. Family history was unremarkable. A gastroscopy was performed because the patient reported a gastric pathology. The gastroscopy revealed a mass 2 cm in diameter that was situated in the submucosal layer in the prepyloric area of the antrum that partially narrowed the pyloric passage (Figure 1). An endoscopic biopsy was not done because the gastric mucosa membrane was normal. So, abdominal ultrasound (US) and endoscopic ultrasound (EUS) are performed. A 2×2.5 cm submucosally located cystic mass lesion, including hyperechoic areas, was detected by ultrasonography at the gastric antrum. In addition, multiple gall bladder calculi were noted. There was no detected lymphadenopathy (LAP) at the perigastric area (Figure 2). There was no pathological finding on the complete blood count or biochemical tests.
Discussion
GCP is a rare benign lesion of the stomach. It was initially recognized in 15 cases that presented by Franzin (1981). Laratte et al (2012) have reviewed this condition and have mentioned that 37 cases have been reported in the English literature. It was seen more in males and the mean age is 60. It occurred most commonly in the corpus of the stomach (62%) and the fundus (24%). The most common complaints of GCP are abdominal pain, bleeding, bloating, loss of appetite, and anemia. There were no complaints in 19% of patients and it was detected incidentally in report by Laratte et al (2012)
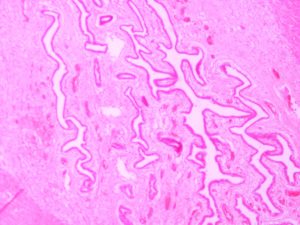
GCP describes gastric glands covered with normal gastric mucosa that exist under the submucosal layer and form cystic expansion. The pathogenesis relates to the degradation of the integrity of the muscularis mucosa layer and the emigration of epithelial cells to the submucosa. The etiology is not clear but the most important reason is previous gastric surgery. Laretta et al (2012) have stated that 65% of the patients have had a history of previous surgery. Chronic inflammation, ischemia, and a reaction to suture materials are considered to be other causes. Our patient did not have previous stomach surgery or a complaint of ulcers.
In a research study by Xu et al (2011), the writers suggest that the differential diagnosis of GCP should include lymphoma, stromal tumors, gastric cancer, and Ménétrier’s disease.
Complaints of the patients are nonspecific. Itte et al (2008) mentioned that it may present as abdominal pain, nausea, vomiting, bloating, acid reflux, and/or bleeding. Our patient had abdominal pain and vomiting, but the patient also had gallstones as an additional pathology to explain these complaints.
GCP cannot be diagnosed by routine endoscopic biopsy due to the submucosal location. However, it can be detected as a mass lesion in the stomach wall by US and tomography. An endoscopic biopsy was not performed in our patient because the gastric mucosa over the mass was normal. On endoscopy, it can be seen as a submucosal mass pending gastric lumen or the polypoid fold of the gastric wall. On EUS, it can be seen as a cystic mass in the stomach wall.
There is not a standard preoperative diagnostic or treatment protocol for GCP. Mitomi et al (1998) mentioned that ultra sound-guided percutaneous needle biopsy or endo-ultrasound-guided needle biopsy can be performed preoperatively for histopathological examination. Definitive diagnosis is usually made after resection of the lesion. Also, frozen section can be performed peroperatively. In order to avoid unnecessary extensive surgery, a preoperative diagnosis of such lesions is important.
There is no consensus about the treatment because of the rarity of GCP. Xu et al (2011) mentioned that unnecessary extensive resections were performed in some patients due to the difficulty of preoperative diagnosis. Different types of surgeries were performed ranging from submucosal excision to total gastrectomy in a research study by Laretta et al (2012).
Although GCP is a benign lesion, Mitomi et al (1998) suggested that it has been a precancerous lesion. Therefore, resection or close follow-up is proposed after the diagnosis is confirmed. The monitoring can be done with computed tomography or magnetic resonance imaging scan. The probable indications for resection are complaints such as pain, nausea, vomiting, anxiety caused by periodical controls, the high cost of controls, any suspicious findings in radiologic and pathologic tests. To date, there have been no reported cases of recurrence or a malignant change in patients who had surgery for the lesion.
Conclusion
In conclusion, GCP is a rare lesion of the stomach, and can be confused with other gastric pathologies. Preoperative diagnosis is important because it can prevent unnecessary extensive resections. GCP should be kept in mind in the differential diagnosis of gastric submucosal masses.
References
1. Franzin G, Novelli P. (1981) “Gastritis cystica profunda,” Histopathology 5:535-547 .
Publisher – Google Scholar
2. Itte V, Mallick IH, Moore PJ. (2008) “Massive gastrointestinal haemorrhage due tgastritis cystica profunda,” Cases J 1: 85
Publisher – Google Scholar
3. Laratta JL, Buhtoiarova T N, Sparber LS, Chamberlain RS. (2012) “Gastritis cystica profunda: A rare gastric tumor masquerading as a malignancy,” Surgical Science 3: 158-164
Publisher – Google Scholar
4. Mitomi H, Iwabuchi K, Amemiya A, Kaneda G, Adachi K, Asao T. (1998) “Immunohistochemical analysis of a case of gastritis cystica profunda associated with carcinoma development,” Scand J Gastroenterol 33: 1226-1229
Publisher – Google Scholar
5. Xu G, Qian J, Ren G, at al. (2011) “A case of gastritis cystica profunda,” Ir J Med Sci 180: 929—930
Publisher – Google Scholar