Discussion
A lithopedion is a dead fetus which underwent intra-abdominal calcification and not spontaneous resorption⁴.
There is a report in the literature on a lithopedion presenting as an ovarian neoplasm⁴.
Most cases of lithopedia are discovered incidentally at surgery, autopsy, or on x-ray².
Abdominal pregnancies are rare, and usually are secondary to tubal rupture or tubal abortion. There is subsequent re-implantation of the embryo onto the bowel, omentum or mesentery4,5.
The risk factors for ectopic pregnancies in general are infertility, previous pelvic infection, congenital anomalies, endometriosis, previous ectopic pregnancy and tubal surgery5.
The mortality risk from abdominal pregnancy is higher than that of tubal pregnancy, and intra-uterine pregnancy³.
In these patients the mortality is usually due to intra-abdominal bleeding, which leads to anaemia. Other causes of death are infections, disseminated intravascular coagulopathy, pulmonary embolism and fistulae caused by penetration of fetal bones³.
A lithopedion can develop following extra-uterine pregnancy, fetal death after the first trimester, failure to diagnose extra-uterine pregnancy early, and conditions favourable for calcification1,2.
In 1881 Kuechenmeister classified retained abdominal pregnancy into 3 classes1,2.
Lithokelyphos in which only the fetal membranes are calcified.
Lithokeyliphopedion in which both the membranes and fetus are calcified.
True lithopedion in which the fetus is calcified, but calcification of the membranes is absent or minimal.
Complications of lithopedion are caecal volvulus, intestinal obstruction, abscess formation, perforation of the urinary bladder and rectum as well as extrusion of fetal parts through the abdominal wall⁴.
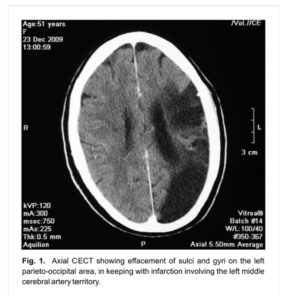
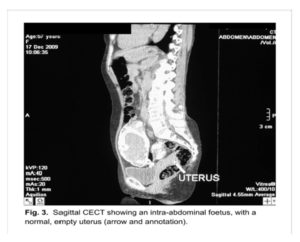
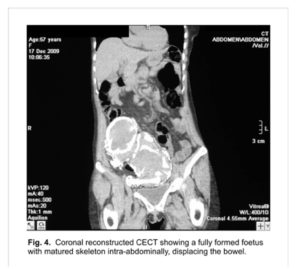
An x-ray of the abdomen is enough to confirm the diagnosis. Computerised tomography (CT scan), and magnetic resonance imaging (MRI) clearly demonstrate the pathology, and assist with the diagnosis of associated complications prior to surgery¹. The CT scan clearly shows the empty uterus and adnexae free of ovular membranes, as in our case.
The differential diagnosis to be considered, especially if the foetus is not clearly defined are teratomas, ovarian tumours, calcified uterine fibroids, inflammatory masses, urinary tract and bladder tumours¹. In a foetus with well formed skeleton, radiological investigations will reveal the diagnosis of a lithopaedion¹.
Some cases of retained abdominal pregnancy may remain stable without surgical intervention, while others may need early surgical intervention after thorough consideration of the morbidity and the risk of complications if not treated accordingly⁴.
Conclusion
Intra-abdominal pregnancy may be fatal, with significant maternal and perinatal mortality5.
A finding of lithopedion implies an absence of adequate medical attention or some rather serious mistakes in medical judgement2,6.
The case can never over-emphasize the importance of good history taking, systematic and thorough patient examination at all levels of healthcare. A clinical diagnosis is virtually impossible but radiological investigations like X-Rays, CT-Scan and MRI will clinch the diagnosis. Discovery of such a condition calls for holistic patient management, considering the psycho-social impact on the patient and family.
In our patient we believe the lithopaedion was not diagnosed earlier because it was not symptomatic and she never sought medical attention for it. It was an incidental finding in a patient who presented with a hypertensive cerebrovascular accident.
References
1. Passini JR, Roxana K, Angela PM, et al. Calcified abdominal pregnancy with eighteen years of evolution: Case Report. Sao Paulo Med J/Rev Paul Med 2000;118(6):192-194
Google Scholar
2. Lachman N, Satyapal KS, Kalideen JM, et al. Lithopedion: A Case Report. Clin Anat 2001;14:52-54
Publisher – Google Scholar
3. Kun KY, Wong PY, Ho MW, et al. Abdominal pregnancy presenting as a missed abortion at 16 weeks’ gestation. HKMJ 2000 Dec;6(4):425-427
Google Scholar
4. Kim SM, Park S, Lee TS. Old Abdominal Pregnancy Presenting as an Ovarian Neoplasm. J Korean Med Sci 2002;17:274-275
Google Scholar
5. Cotter A, Izquierdo L, Heredia F. Abdominal pregnancy [monograph on the internet] The Fetus.net,2000 [2000-10-22-11] Available from: http://www.thefetus.net/page.php?id=1032
6. Woodbury JW, Jarrett JC. Abdominal lithopedion retained for thirteen years: Case Report with review. Am J Obst & Gynec 1960;80:590-595
Google Scholar