Introduction
Soft-tissue foreign bodies often results from penetrating trauma. Not all retained foreign bodies are discovered in the first consultation at the emergency department. Some foreign bodies can remain for years after the initial trauma before causing any complaints. Often symptoms are not very specific and the initial injury is not remembered by the patient. Effects of these foreign bodies reactions might be granuloma up to soft-tissue masses mimicking a neoplasm or phlegmonous inflammation up to abscesses. Particularly in cases of long-standing foreign bodies, the detection of those might be challenging. We demonstrate a case of a late soft-tissue abscess caused by an attack of a male deer.
Case report
A 60-year-old woman was referred to the hospital due to the increasing pain and the beginning of reddening of her right upper leg without any acute injury. Asking about her medical history the patient revealed an attack of a male deer more than five years ago in which she suffered several thrusts caused by the deer`s antlers. The initial examination at another emergency department supposedly showed no foreign bodies in the superficial wounds from the deer attack. The primary wound healing showed no abnormalities but since that incident she often complained about unspecific pain in this area. The clinical examination showed a slightly swelled, reddened and tender area of approximately 12 x 8 cm at the right dorsal upper leg and another finding of 3 x 3 cm at the middle part of the medioventral thigh. There was no impaired blood flow or sensitivity. Plain radiography showed two bone-like structures next to the femoral diaphysis without any recognizable fractures (fig. 1).

Figure 1: Plain radiography of the right upper thigh. It shows structures with bone-like density. One is located proximally ventrolateral of the femur (*) and the other smaller one more distal at the dorsal femur diaphysis. No fractures of the surrounding bones were detected.
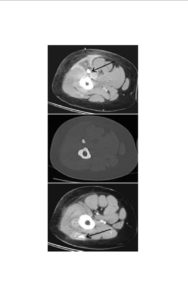
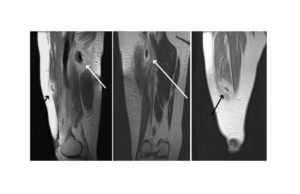
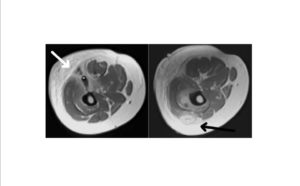
Contrast enhanced MRI and CT showed an extensive inflammatory reaction of soft-tissue in the area of the foreign bodies and further a concurring reaction of the bone marrow of the femur. The CT images also revealed a bone like structure corresponding to the plain radiography (fig. 2 – 4).
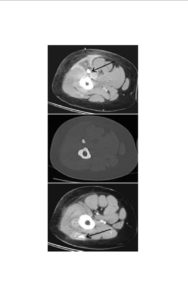
Figure 2: Contrast enhanced axial CT showed the previously described bone-like structures (arrow). These are surrounded by abscesses with strong marginal contrast enhancement (A and C). Bone windowing (B) showed a similar density compared with the femur bone.
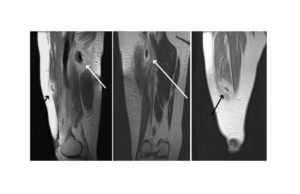
Figure 3: T1-weighted MRI in sagittal (A) and coronar (B and C) reformations. Abscess structures at the dorsal (white arrow) and ventral (black arrow) area of the thigh with extended inflammatory reaction of the surrounding soft tissue and muscles.
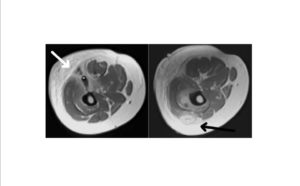
Figure 4: Axial MRI (T1w) showing the abscesses (arrow). Concerning the suspected foreign bodies the findings are not conclusive (compare * in A and B).
CT-guided biopsy of a circumscribed liquid structure next to the cranial located foreign body revealed purulent material. The patient now received surgery and antibiotic therapy. Histopathological examination identified the two excised bone-like structures (fig. 5) as a part of deer horns. After a few days the patient was discharged in good condition.

Figure 5: Surgical excised structures which could be identified as deer horn.

Figure 6: A male european deer marking his territory by rubbing it antlers on trees and bushes.
Discussion
The male european deer (Capreolus c. Capreolus, fig. 6) has got small antler`s with bone-like composition of organic and inorganic substances. The deer is an herbivorous, ruminate animal and attacks against humans are very rarely described. In turf wars, male deer might cause to each other severe injuries with their antlers. Only hand raised or reintroduced deer seems to have a tendency of losing their natural fear and may consider humans as a rival.
Retained soft-tissue foreign bodies are often not assumed and much less detected at initial examination in the emergency department. In an earlier study by Anderson et al., 38% of foreign bodies were overlooked in the first examination. Although plain radiography is routinely obtained in soft-tissue lacerations Manthey et al., ascertained that it often fails in detecting small or non-radiopaque foreign bodies. Like Horton et al., and Boyse et al., mentioned sonography has shown excellent rates in detection and exact localization of foreign bodies of different materials and is – at the same time – able to detect associated lesions in the soft-tissue (e.g. abscesses) and neurovascular abnormalities. Soft-tissue foreign bodies have nonspecific MRI imaging characteristics although Monu et al., demonstrated the use of MRI in the differential diagnosis in those cases. CT imaging is specific in detecting radiopaque foreign bodies and surrounding complications but due to the radiation risk a cautious use is advisable. An additional problem in the diagnosis path of long-standing retained foreign bodies is that, the acute symptoms might not be put in context with the (minor) initial trauma by the patient and/or physician. The initial trauma may has occurred many years ago as for example battlefield injuries in World War II. These retained foreign bodies are mostly radiopaque (e.g. bullets or shrapnels). Even though the localization in the body is known, the acute symptoms may not be related to it by the patient. In a retrospective survey by Surov et al., only 2% of metal foreign bodies from World War II became clinically apparent from infection, migration or soft tissue reaction [6].
Conclusion
In our case the retained foreign bodies were radiopaque and the findings corresponded with patient`s history. The further imaging modalities used in this case were applied to evaluate the extent of the apparent inflammatory processes in the soft-tissue. CT clearly identified the structures not as calcified but bone-like without revealing any fractures in the thigh and also provided pathogen detection of the abscess by biopsy. MRI could display the soft-tissue reaction, further a concurring reaction of the bone marrow and lastly ruled out soft-tissue masses in the sense of neoplasm. the findings in the different imaging modalities facilitated the surgery and further more facilitated the antibiotic therapy. In this case no sonography was applied because of the explicit finding in the plain radiography. Certainly it has detected the abscesses but due to the depth of the foreign bodies, the radiography has failed to detecte these foreign bodies. As mentioned above sonography has its value in the first examination in addition to plain radiography when foreign bodies are suspected. The key points in the diagnosis of retained foreign bodies are a thorough clinical examination, the investigation of the patient`s history to initiate the assumption of the existence of a foreign body and then to choose the right imaging method.
In Europe, attacks by feral animals are very rare. Due to this fact the experiences with the pattern of injuries caused by those might be restricted in an emergency department. Thus one should be aware that any penetrating trauma caused by animals could leave pathogens, toxins and foreign bodies behind in the tissue. In case of doubt it is important to think about additional imaging modalities in due time.
References
1. Anderson M. A., Newmeyer III W. L. and Kilgore Jr E. S. (1982) “Diagnosis and treatment of retained foreign bodies in the hand,” Am J Surg, 144 (1) 63-67.
Publisher – Google Scholar
2. Boyse T. D., Fessell D. P., Jacobson J. A., Lin J., van Holsbeeck M. T. and Hayes C. W. (2001) “US of soft-tissue foreign bodies and associated complications with surgical correlation,” RadioGraphics, 21 (5) 1251-1256.
Publisher – Google Scholar
3. Horton L. K., Jacobson J. A., Powell A., Fessell D. P. and Hayes C. W. (2001) “Sonography and radiography of soft-tissue foreign bodies,” AJR, 176 (5) 1155-1159.
Publisher – Google Scholar
4. Manthey D. E., Storrow A. B., Milbourn J. M. and Wagner B. J. (1996) “Ultrasound versus radiography in the detection of soft-tissue foreign bodies,” Ann Emerg Med, 28 (1) 7-9.
Publisher – Google Scholar
5. Monu J. U. V., McManus C. M., Ward W. G., Haygood T. M., Pope Jr T. L. and Bohrer S. P. (1995) “Soft-Tissue masses caused by long-standing foreign bodies in the extremities: MR imaging findings,” AJR, 165 (2) 395-397.
Publisher – Google Scholar
6. Surov A., Thermann F., Behrmann C., Spielmann R. P. and Kornhuber M. (2012) “Late sequelae of retained foreign bodies after world war II missile injuries,” Injury 4
Publisher – Google Scholar