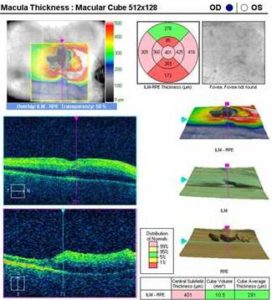
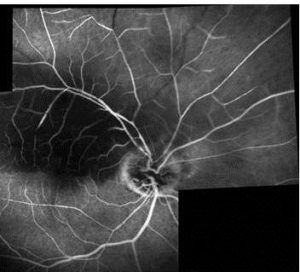
The presented additional examinations confirmed the diagnosis of retinal embolization syndrome in the right eye. We decided to implement standard treatment for retinal artery occlusion disorders.
Despite the immediate lowering intraocular pressure therapy (anterior chamber paracentesis + timolol eye-drops topically and 2 tablets of acetazolamide administered orally) during follow-up, after 1, 3 and 6 months we did not observe any distinct improvement in visual acuity.
Discussion
The two main clinical manifestations of CES are peripheral cutaneous involvement and acute renal insufficiency. The precise clinical syndrome depends on the location of the source of embolism. Since the abdominal aorta is the most common location of atherosclerosis, the kidneys, visceral organs, and lower extremities are commonly involved. Atheromas of other arteries, such as the ascending aorta or the carotid, may result in emboli, producing neurologic, retinal, or cardiac symptoms. The risk factors for CES include advanced age, smoking, hypertension, diabetes mellitus, hyperlipidemia, and peripheral vascular disease. CES is seen following invasive vascular procedures as in our patient, thrombolytic therapy, or anticoagulants, but may occur spontaneously as well [1].
CES has been observed after both surgical CEA and percutaneous carotid stenting. Most perioperative complications are ischemic cerebral lesions and they are due to CES or hypoperfusion from carotid clamping, being a part of the surgical procedure. On the contrary, the events in the later postoperative period are related to thromboembolism from the newly debrided arterial walls or dissection of an intimal flap [3].
Carotid stenting is emerging as an alternative procedure to carotid endarterectomy in patients with significant carotid artery stenosis. Nevertheless, still numerous microemboli can be shed during carotid angioplasty [4]. The risk of periprocedural ischemic strokes due to embolism after carotid stenting is about 5%. This risk is nowadays considerably lowered due to the use of embolism protection devices [5-7].
The most common cause of RAO is embolism. In stable conditions (without any invasive procedures), the carotid artery and the heart are the most common sources. Carotid artery disease can cause RAO by three mechanisms: embolism, hemodynamically and serotonin induced arterial spasm. The major source of emboli is plaques in the carotid arteries, like in the present case, and much less frequently stenosis. On the contrary, during and after cardiovascular procedures, embolic material originates from other arteries [8-10].
Atheromatous plaque embolism may occur at the time of CEA procedure when plaque material dislodges and embolizes to intracranial vessels, like central retinal artery or branches of retinal artery. It may also occur at a later time as it happened in our case.
In the present case, clinical evaluation suggests that cholesterol plaques moved during CEA are the main cause of retinal embolization. It is uncommon according to the fact that most CESs happen after endovascular procedures and are attributable to endovascular catheter usage.
Conclusions
The present case report shows that there is a rare possibility of RAO due to CES as a complication of the surgical restoration of ICA. Detached intravascular embolic material in the reopened artery is probable cause of this complication.
References
1. Saric, M. & Kronzon, I. (2011). “Cholesterol Embolization Syndrome,” Current Opinion in Cardiology, 26 (6) 472-479.
Publisher – Google Scholar
2. Nucci, C., Martelli, E., Appolloni, A. & Palma, S. (1997). “A Case of Central Retinal Artery Occlusion after Carotid Endoarterectomy,” Eye (London, England), 11 (Pt 5) 755-757.
Publisher – Google Scholar
3. Sila, C. A. (1998). “Neurologic Complications of Vascular Surgery,” Neurologic Clincs, 16 (1) 9—20.
Publisher – Google Scholar
4. Rapp, J. H., Pan, X. M., Yu, B., Swanson, R. A., Higashida, R. T., Simpson, P. & Saloner, D. (2003). “Cerebral Ischemia and Infarction from Atheroemboli <100 Microm in Size,” Stroke , 34 (8) 1976—1980.
Publisher – Google Scholar
5. Zahn, R., Mark, B., Niedermaier, N., Zeymer, U., Limbourg, P., Ischinger, T., Haerten, K., Hauptmann, K. E., Leitner, E. R., Kasper, W., Tebbe, U. & Senges, J. (2004). “Embolic Protection Devices for Carotid Artery Stenting: Better Results than Stenting without Protection?,” European Heart Journal, 25 (17) 1550—1558.
Publisher – Google Scholar
6. Roubin, G. S., Iyer, S., Halkin, A., Vitek, J. & Brennan, C. (2006). “Realizing the Potential of Carotid Artery Stenting: Proposed Paradigms for Patient Selection and Procedural Technique,” Circulation, 113 (16) 2021—2030.
Publisher – Google Scholar
7. Kastrup, A., Groschel, K., Krapf, H., Brehm, B. R., Dichgans, J. & Schulz, J. B. (2003). “Early Outcome of Carotid Angioplasty and Stenting with and without Cerebral Protection Devices: A Systematic Review of the Literature,” Stroke, 34 (3) 813—819.
Publisher – Google Scholar
8. Blanco, V. R., Moris, C., Barriales, V. & Gonzalez, C. (2000). “Retinal Cholesterol Emboli during Diagnostic Cardiac Catheterization,” Catheterization and Cardiovascular Interventions, 51 (3) 323-325.
Publisher – Google Scholar
9. Bucci, F. A. Jr., Dimitsopulos, T. M. & Krohel, G. B. (1989). “Branch Retinal Artery Occlusion Secondary to Percutaneous Transluminal Coronary Angioplasty,” British Journal of Ophthalmology, 73 (4) 309-310.
Publisher – Google Scholar
10. Stefansson, E., Coin, J. T., Lewis, W. R. 3rd., Belkin, R. N., Behar, V. S., Morris, J. J. Jr. & Anderson, W. B. (1985). “Central Retinal Artery Occlusion during Cardiac Catheterization,” American Journal of Ophthalmology, 99 (5) 586-589.
Publisher – Google Scholar