Introduction
Esophageal diverticula are rare with a reported prevalence of 0,06-4% (Hoghooghi et al., 2006, Watanabe et al., 1996). As symptoms are often unspecific and size usually progresses slowly over time, years can pass before diagnosis. Epiphrenic esophageal diverticula are located in the lower third of the esophagus and may be complicated by esophagitis, bleeding, malignancy and very seldom perforation.
We describe a rare case of an epiphrenic esophageal diverticulum, complicated by perforation and leakage below the diaphragm, in a patient with known benign esophageal stricture and esophagitis.
Case presentation
A 57-year old male patient with known benign esophageal stricture, dysphagia and recurrent pneumonia was referred to our emergency department with suspected aspiration pneumonia. The patient had been known with frequent esophagitis and chronic stenosis in the lower eosophagus for 6 years, for which he was treated with daily proton pump inhibitors and frequent dilatation of the esophagus. His last esophagogastroduodenoscopy (EGD) was performed 6 months prior to the admission; and it revealed the known distal stenosis requiring dilatation of esophagus, with a balloon diameter of 18 mm. The patient had earlier had a percutaneous endoscopic gastrostomy (PEG) tube because of dysphagia, but the tube had recently been removed because of an infection. He had undergone previous surgery with gastro-entero-anastomosis (GEA) because of pyloric stenosis 2 months earlier, and now suffered from cough, bronchial rales, dysphagia, and fatigue. Known comorbidities consisted of insulin-dependent diabetes mellitus type 1, chronic pancreatitis and a history of previous fungal pneumonia. At referral, clinical examination revealed an emaciated man with elevated temperature (38,5 Celsius rectal), a blood pressure of 100/77 mmHg, pulse of 88 and a body mass index of 15.9 kg/m2. Laboratory findings showed Hb of 5,9 mmol/l, Potassium of 3,0 mmol/l, Sodium of 128 mmol/l, Albumin of 19 g/l, Blood Glucose Level of 2,2 mmol/l, CRP of 137 mg/l and a leucocyte count of 2,5 bio/l. Hypoglycemia was corrected with a combination of glucose infusion and short-acting insulin and treatment with broad-spectrum antibiotics was initiated. Because of poor health condition and anorexia, he got parenteral nutrition.
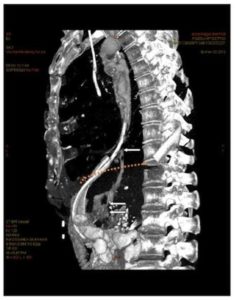
A few days after admission, placement of a new PEG tube was contemplated, and prior to this, a thoracoabdominal computed tomography with intravenous and oral contrast was performed. The CT scan demonstrated left side pleural effusion, dilatation of the mid-esophagus (mega-esophagus), and surprisingly a gastrointestinal leakage below the diaphragm at mid-level of the minor curvature of the stomach (Fig. 1).
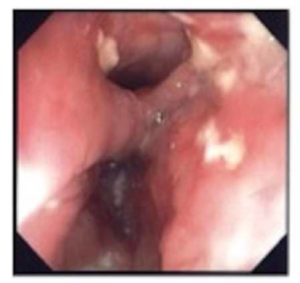
Figure 2: Photodocumentation from the esophagoscopy, photo taken at the same level as the upper arrow in Fig. 1
The photo demonstrates the neck of the diverticulum in the distal part of esophagus.
The lower lumen is the esophagus and the upper lumen is the diverticulum.
At the esophagogastric junction there was a stenosis, as described earlier. The second lumen appeared to be a diverticulum with the same diameter as the esophagus, lying parallel to the esophagus on the patient’s right side and ending blindly after 20 cm. After the application of Gastrografin into the diverticulum under fluoroscopic control, contrast extravasation below the diaphragm in close proximity to the minor curvature of the stomach was demonstrated. The GEA looked completely unsuspicious. The patient was treated with a left side chest tube, and the serous pleural fluid was sent for cultivation, but was later found without bacterial growth. The patient was transferred to the Department of Abdominal Surgery for further treatment. Since the patient was in poor health condition and the leakage was only minimal, without any signs of peritonitis, a conservative treatment option involving the placement of a nasogastric tube, total parenteral nutrition and treatment with broad-spectrum antibiotics was chosen. Upon improvement of the patients’ condition, dilatation of the stricture and the placement of a PEG tube for nutritional purposes were performed.
The patient was discharged 10 days after admission. A few weeks later, he got the diagnosis achalasia and was he was seen every second months for dilatation of esophagus in the GIT Outpatient Clinic.
Eight months after admission, he was diagnosed with an aggressive pulmonary cancer, and died shortly after.
Discussion
The patient in our case report presented with a tubular paraesophageal structure with a proximal opening in the lower third of esophagus. The most likely explanation for this finding is an epiphrenic pulsion diverticulum, while less likely, in accordance with the clinical picture and the patient’s age, is an esophageal duplication. A definitive diagnosis could only have been achieved by resection and histopathological examination of the specimen, which was not possible, since the patient was not eligible for surgery.
A diverticulum is in general an out-pouching or sac of the epithelial-lined tissue of the gastrointestinal canal. Esophageal diverticula are most commonly false diverticula, involving only the mucosa and submucosal layers of the esophageal wall (Baker et al., 1999). Diverticula of the esophagus are generally categorized by their location, e.g. upper (usually Zenker’s diverticula) and lower (epiphrenic) diverticula, with the epiphrenic type located in the terminal 10-15 cm of the esophagus. Further categorization relates to presumed mechanism, termed pulsion vs. traction, whereas the first being the most common. Pulsion diverticula are false diverticula, caused by excessive outward pressure on the esophageal wall, in time causing an out-pouching of the esophagus. Traction diverticula are true diverticula, caused by traction from the outside of the esophagus, due to periesophageal inflammation or fibrosis (as seen in e.g. tuberculosis or histoplasmosis). Studies suggest that pulsion diverticula develop as a consequence of an underlying motility disorder of the esophagus in up to 80% of patients (Baker et al., 1999, do Nascimento et al., 2006, Schima et al., 1997). The motility disorders encountered with pulsion diverticula are either non-specific, diffuse esophageal spasm or achalasia, all characterized by functional obstruction and high luminal pressures. However, an obstruction of the esophagus can also be of mechanical nature, including strictures and tumours. Duodenal obstruction has also been described to be associated with pulsion diverticula of the esophagus(Thomas et al., 2001).
The most common symptom of an esophageal diverticulum is dysphagia, followed by regurgitation and/or vomiting (Thomas et al., 2001). Other known symptoms are retrosternal pain, cough (mostly nocturnal, a symptom of aspiration) weight loss and halitosis (do Nascimento et al., 2006). With an underlying motor disorder being very common, it is important to acknowledge that symptoms often are a reflection of the motor disorder, rather than of the diverticulum itself.
Complications from esophageal diverticula are ulceration and bleeding, pneumonia (due to aspiration), fistula, perforation and even cancer. Diverticular perforations are extremely rare and can be spontaneous or most often iatrogenous due to instrumentation.
The only reasonable medical therapy in patients with esophageal diverticula consists of proton pump inhibitors, since esophagitis is not uncommon in these patients. Furthermore, all patients with esophageal diverticula should be evaluated for surgical treatment, since complications such as bleeding and perforation can be life threatening. Besides resection of the diverticulum, the underlying motor disorder should be approached as well in order to prevent recurrence as well as operative leakage. Surgical treatment can either be performed by thoracotomy or video-assisted thoracoscopy (VATS), with excision of the diverticular sac by means of a stapling device, or simple suturing, or a combination of both with oversewing of the stapler line. As mentioned before, the procedure should be combined with esophageal myotomy in order to treat an underlying motor disorder, which is shown to lower the risk of persistent or recurrent symptoms, diverticular recurrence and postoperative leakage from a diverticulectomy suture line (Thomas et al., 2001). Since surgical treatment can be associated with serious complications, especially in patients suffering from malnutrition and severe comorbidities, non-operative treatment such as dilatation of an underlying stenosis and nutrition via nasogastric tube or PEG tube are valuable treatment options in selected cases.
Digestive duplications present themselves in to ways: either as duplication cysts (most frequent form, contributing approximately 95% of cases) or as tubular structures (Coumaros et al., 2010), containing smooth muscle layers and digestive mucus membrane. Ileum and esophagus are the most frequent locations, and esophageal diverticula (ED) represent 10-20% of congenital esophageal malformations (Neo et al., 2004). Digestive duplications are usually identified during childhood, with 70-90% of cases diagnosed before the age of 2 years (Coumaros et al., 2010). When diagnosed in adulthood, symptoms are most often caused by complications such as infection or rupture (Neo et al., 2004). Treatment of an esophageal duplication cyst is enucleation of the cyst. Because of the rarity of tubular ED, no standard treatment has been recommended, and the choice of management depends on size and location of the duplication, as well as the local surgical expertise.
The patient’s symptoms were compatible with those of a stricture or dysmotility of the esophagus, which corresponded with the endoscopic findings of a giant dilatation proximal to the double lumen esophagus, formed as a consequence of a year-old relative stricture or because of achalasia.
We believe that the most likely diagnosis in our patient was a long pulsion diverticulum, which progressed gradually over time, forming a long paraesophageal tubular structure ending below the diaphragm. Since earlier, repeated EGDs (through 6 years), of which the most recent before this episode beeing performed 6 months ago, revealed no findings of an esophageal duplication or diverticulum, and the patient had been asymptomatic until the age of 50 years, esophageal duplication seems to be very unlikely.
Conclusion
Epiphrenic esophageal diverticula complicated by perforation are an extreme rarity, and a case with perforation and leakage below the diaphragm has never been reported before. Furthermore this case report demonstrates, that in selected cases, even with a large diverticulum and perforation, a conservative treatment option may be a valuable treatment option.
References
1. Baker, M. E., Zuccaro, G., Jr., Achkar, E.and Rice, T. W. (1999). Esophageal diverticula: patient assessment. Semin Thorac Cardiovasc Surg, 11, 326-36.
2. Coumaros, D., Schneider, A., Tsesmeli, N., Geiss, S.and Becmeur, F. (2010). Endoscopic management of a tubular esophageal duplication diagnosed in adolescence (with videos). Gastrointest Endosc, 71, 827-30.
Publisher – Gogle Scholar
3. Do Nascimento, F. A., Lemme, E. M.and Costa, M. M. (2006). Esophageal diverticula: pathogenesis, clinical aspects, and natural history. Dysphagia, 21, 198-205.
Publisher – Google Scholar
4. Hoghooghi, D., Coakley, F. V., Breiman, R. S., Qayyum, A.and Yeh, B. M. (2006). Frequency and etiology of midesophageal diverticula at barium esophagography. Clin Imaging, 30, 245-7.
Publisher – Google Scholar
5. Neo, E. L., Watson, D. I.and Bessell, J. R. (2004). Acute ruptured esophageal duplication cyst. Dis Esophagus, 17, 109-11.
Publisher – Google Scholar
6. Schima, W., Schober, E., Stacher, G., Franz, P., Uranitsch, K., Pokieser, P., Wenzl, E., Resch, A.and Herold, C. J. (1997). Association of midoesophageal diverticula with oesophageal motor disorders. Videofluoroscopy and manometry. Acta Radiol, 38, 108-14.
Publisher – Google Scholar
7. Thomas, M. L., Anthony, A. A., Fosh, B. G., Finch, J. G.and Maddern, G. J. (2001). Oesophageal diverticula. Br J Surg, 88, 629-42.
Publisher – Google Scholar
8. Watanabe, S., Matsuda, K., Arima, K., Uchida, Y., Nishioka, M., Haruo, T.and Uohashi, T. (1996). Detection of subclinical disorders of the hypopharynx and larynx by gastrointestinal endoscopy. Endoscopy, 28, 295-8.
Publisher – Google Scholar