Introduction
In Australia, the current Royal Australian College of General Practitioners (RACGP) guidelines (2012) [1] and the Victorian Department of Health advice [2] do not recommend population-based prostate cancer screening. However, the Urological Society of Australia and New Zealand (USANZ) recommends PSA testing together with digital rectal examination (DRE) for men in the 55-69 age group under certain circumstances [3] and the age at which men are recommended to have a test to help identify whether their risk of prostate cancer be reduced from 50 to 40 years of age, with monitoring being determined by the individual’s risk [4].
In the past, prostate-specific antigen (PSA) screening has been reported as beneficial, [5, 6] particularly when men were fully informed of the potential risks, benefits and uncertainties of investigations and treatment [7-10]. Despite previous statements indicating there is an absence of evidence to support population screening [2, 11, 12], there is still considerable debate as to whether screening is beneficial and/or whether opportunistic screening should be offered [11-15].
Until recently, public awareness of prostate cancer and related issues was poor [16]. A national survey conducted in Australia in 2002 found that only 52% of men felt informed about prostate cancer [17]. A study undertaken in 2006 in Western Australia to ascertain men aged 40-80 understanding about prostate cancer found that 35% had no knowledge of treatments available and 53% had no knowledge of the side effects of treatments [18].
Yet, two of the most common reasons men sought and underwent testing were because of GP recommendation or media publicity [19], the latter providing an overwhelmingly positive stream of encouragement to seek testing [11, 12].
Advertising and awareness campaigns such as the Movember website [13] and social networking sites such as Twitter and Facebook play a valuable role; especially for younger generations who are more likely to use these sites [20]. Although prostate cancer is rare in men under 40 [21], the latter are rarely included in studies on prostate cancer [8, 10, 12, 19, 21] If these campaigns are successful, particularly in raising men’s awareness about prostate cancer, this may translate into men being more informed and change health habits in decades to come.
In 2010 in Australia, prostate cancer was the fourth leading cause of death, accounting for the death of 3235 men [22]. Known risk factors include a positive family history and increasing age [1, 7, 21]. While incidence rates increase for men over the age of 65 years and mortality rates increase over the age of 70 [15, 18], men’s survival rates have increased in recent years [23]. Known risk factors include a positive family history and increasing age [1, 7, 17, 21]. However, men as young as 34 have been diagnosed with prostate cancer, and younger men diagnosed are more likely to die prematurely [7, 13].
While the virtues of screening continue to be debated, men need accurate information [14]. As men generally trust GPs to provide accurate advice about symptoms, tests and treatment, and manage any diagnosis or potential problems [15, 18], GPs may be in the best position to assist men, particularly those who are poorly informed, prefer to ignore health issues, or their perception of their personal risk and vulnerability influences decisions about testing [7, 16, 18]. Another option may be for women to be included in the discussion as they often seek information to support their partner [16].
The aim of this study was to investigate “What men know about prostate cancer symptoms and treatment”.
Methods
A questionnaire comprising six single-answer and six multiple-option questions was developed and tested on two groups to ensure the questions were clear, by checking whether the questions were understood, evaluating collection procedure and ensuring there were no production mistakes. One group comprised six clinical and research colleagues (GPs) to ensure the content accurately reflected current guidelines; the second comprised ten males of varying ages to test whether the questions were clear and unambiguous [24, 25].
Participants
Adult men were invited to complete the questionnaire unassisted and anonymously.
Data Collection
Data were collected by two members of the research team (RS and KJ) at two locations; the Monash University Clayton Campus and the Australian Defence Forces (ADF) Barracks in Melbourne. Adult men were invited to participate; if they agreed, they were provided with the explanatory statement and a questionnaire for them to complete unassisted. If they did not engage, they were not spoken to. Consent was implied when the unassisted and anonymously completed questionnaire was returned to the researcher.
Data Analysis
Data were entered and analysed in SPSS [26]. As screening and testing is not currently recommended for men under 40 years, data were divided into two groups; the younger group (18-40) and the older group (41-70) to reflect this recommendation. Percentages were calculated for the cohort (n=100%) and for the two groups – the younger group 40 and under (n=193 100%) and the older group (n= 57 100%) so some comparisons could be drawn.
Ethics approval for this study was through the Monash University Human Research Ethics Committee.
Results
A total of 250 completed surveys were returned to the researchers.
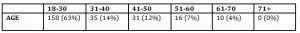
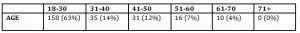
Participants’ age ranged from 18 to 70 with around three quarters aged 40 and under (77%), and one quarter aged 41 years and over (23%) (Table 1).
Table 1: Q 1: Age and age range of participants (n=250)
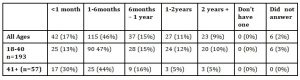
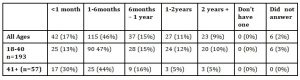
The majority had heard of prostate cancer (87%) and had visited their GP in the past 12 months (89%). Older men (41+) were more likely to have seen their GP in the past month (Table 2).
Table 2: Q 3: Period since men last saw their GP (n-250)
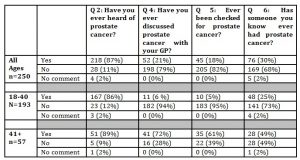
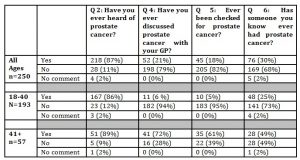
While the majority had heard of prostate cancer (87%), regardless of age, only 20% had discussed the topic with their GP, and fewer (18%) had ever been checked for prostate cancer. Around a third (30%) indicated someone they knew had prostate cancer (Table 3).
Table 3: Participants’ knowledge about prostate cancer, whether discussed with GP, ever Checked, whether someone known ever had cancer (N=250).
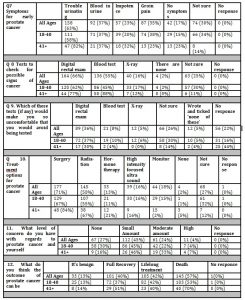
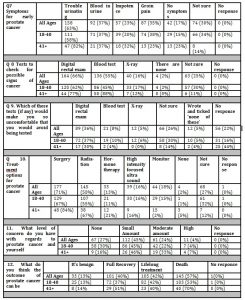
As Questions 7-12 allowed for ticking multiple options within each question, results are expressed in the percentage indicated for each option; these do not add up to 100%. Few (17%) were aware there were ‘no symptoms’ for early prostate cancer but around (30%) were not sure. Trouble urinating’ (63%) was thought to be the most likely symptom, followed by blood in urine (37%) groin pain (35%) or impotence (23%) (Q7; Table 4).
One quarter (25%) was unsure of tests available and a few (2%) indicated ‘none’. Two-thirds were aware of digital rectal exams (66%), with fewer aware of blood tests (55%). More than half of the participants were either not sure (26%) or did not respond (22%) (Q8 Table 4). Digital rectal examination (36%) was seen as more uncomfortable than blood tests (8%), regarding which tests would make individuals so uncomfortable that they would avoid being tested (Q9:Table 4). Around a quarter (27%) were not sure of treatment options, with surgery (71%) or radiation (58%), more well-known than hormone therapy (13%), high intensity focused ultrasound (16%), monitoring (18%) or none (2%) (Q10 Table 4). The level of concern individuals had regarding prostate cancer varied from none (27%), to a small amount (45%), or a moderate amount (24%) with few indicating a high level of concern (4%) (Q11: Table 4). Few thought the outcome of prostate cancer could be ‘benign’ (13%); around half thought the outcome could be full recovery (40%), lifelong treatment (42%) or death (57%) (Q12: Table 4)
Table 4: Symptoms, tests, treatment options, level of concern and outcomes (Questions 7-12 had the option of multiple responses)
Discussion
This study is unique in that an anonymous questionnaire was used for data collection, whereas other studies used a questionnaire administered by GPs [18], an interview based survey [10], telephone interviews [8, 19], face-to-face interviews [14] and/or focus groups [16]. In this study, participants were not cancer survivors [15], thus were without personal experience of prostate cancer [16] and were not likely to be members of prostate cancer support groups [14]. While some questions have been asked in these previous studies, the majority of questions and subsequent responses in this study provide new insight into what men know about prostate cancer symptoms and treatment.
Regardless of age, the majority of the cohort had heard of prostate cancer (87%). While men may be embarrassed and fearful to raise the topic, the older group were slightly more likely to have discussed prostate cancer with their GP suggesting there may be an increase in the number of older men who are having discussions with their GP compared to a previous study when 62% had discussed the ‘pros and cons’ with their GP [19].
However, if GPs adopt the most recent RACGP guidelines which do not recommend opportunistic screening [1], this may explain the low percentage of participants who had discussed prostate cancer with their GP (21%) or had ever been checked for prostate cancer (18%), and expressed little concern about having prostate cancer (45%), because, most likely, these men had little or no knowledge of the function of the prostate, treatments and treatment side effects [18]. The apparent gap in the participants’ knowledge as previously reported by the Prostate Cancer Foundation of Australia [17] highlights the fact that leaving the responsibility with men to raise the topic with their GPs may not be in the men’s best interests, particularly as younger men diagnosed are more likely to die prematurely [18]. Thus, for those who expressed little or small concern, regardless of age, it is important that concerns raised and addressed so they can make an informed choice [17].
While there has been public discourse on prostate cancer in the Australian media, for example a study examined advertising regarding prostate cancer screening in newspapers and television news during the four-year period 2003-2006 [12]; around 10 percent of the statements analysed were found to be factually inaccurate or made claims not supported by the scientific literature[11]. Thus, along with no information from their GP, men’s knowledge may be impaired by the content of news broadcasts, free-to-air television and published print [11, 12]. As the two most common reasons men seek information are media publicity and GP recommendation [19], those who are not seeking information from their GP, may be turning to websites with awareness campaigns such as Movember [17] and other public social networks such as Twitter and Facebook for information [20]. The Movember campaign which began in 2003 appears to be aimed at younger generations [17]. Recent statistics suggest that accessing information on this and other topics via websites and/or social networks is growing in popularity [17, 20]
This study may be limited by the number of venues at which data were collected. The strength of this study is the unanticipated outcome of providing significant insight into younger men’s knowledge about prostate cancer symptoms and treatment; not previously available in the literature. In addition, the results may have implications for men and GPs world-wide.
Conclusion
Men of all ages need access to accurate information about symptoms, tests and treatment options for prostate cancer, and if accurate information is not available via the media, then it is imperative that men can access information from their GPs.
The apparent lack of knowledge demonstrated by participants in this research strongly suggests that it may be of value if GPs opened the conversation by informing men (regardless of age) that there are generally no symptoms of early prostate cancer, thus providing an opportunity for further discussion.
Implications for general practice include
- Regardless of age, men have limited knowledge about symptoms, screening, treatment and outcomes for prostate cancer.
- GPs need clear, concise guidelines with consistent information.
- Men feel embarrassed thus reluctant to raise the issue.
- GPs are best placed to raise the issue and provide accurate information.
Acknowledgements
We gratefully acknowledge the support of:
- The men who agreed to participate and completed the questionnaires, without their
support there would be no results to report.
- Tony Sutherland for arranging access to the ADF and assisting with data collection.
Funding
This study was unfunded.
(adsbygoogle = window.adsbygoogle || []).push({});
References
RACGP: RACGP Red Book. Guidelines for preventive activities in general practice (8th Edn). East Melbourne: RACGP; 2012.
Department of Health Victoria: Conditions we do not screen. In. Downloaded 20/3/2013 http://www.health.vic.gov.au/screening/conditions.htm: Department of Health, Victoria.; 2013.
Urological Society of Australia and New Zealand (USANZ): Urological Society of Australia and New Zealand PSA Testing Policy 2009. In. Downloaded 21/3/2013 www.usanz.org.au: ISAMZ; 2009.
Urological Society of Australia and New Zealand (USANZ): Prostate cancer test age lowered to 40. In. Downloaded 21/3/2013 www.usanz.org.au/usanz-2009-osa-testing-policy: USANZ; 2009.
Lamb DS, Slaney D, Smart R, Nacey JN, Russell G, Scott BM, Johnson CA, Adams JD, Moran S, Delahunt B: Prostate cancer: the new evidence base for diagnosis and treatment. Pathology 2007, 39(6):537-544.
Schroder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, Kwaitkowski M, Lujan M, Lilja H, Zappa M et al: Screening and Prostate-Cancer Mortality in a Randomized European Study. N Engl J Med 2009, 360(13):1320-1328.
Baade PD, Steginga SK, Pinnock CB, Aitken JF: Communicating prostate cancer risk: what should we be telling our patients? MJA 2005, 182(9):472-475.
Gattellari M, Ward JE: A community study using specified and unspecified scenarios to investigate men’s views about PSA screening. Health Expectations 2004, 7:274-289.
RACGP: RACGP Red Book. Guidelines for preventive activities in general practice (7th Edn). South Melbourne: RACGP; 2009.
Weller D, Pinnock C, Silagy C, Hiller JE, Marshall VR: Prostate cancer testing in SA men: influence of sociodemographic factors, halth beliefs and LUTS. ANZ Journal of Public Health 1998, 22(3):400-402.
MacKenzie R, Chapman S, Barratt A, Holding S: “The new is [not] all good”: misrepresentations and inaccuracies in Australian news media reports on prostate cancer screening. MJA 2007, 187(9):507-510.
MacKenzie R, Chapman S, Holding S, McGeechan K: ‘A matter of faith, not science’: analysis of media coverage of prostate cancer screening in Australian news media 2003 – 2006. Journal of the Royal Society of Medicine 2007, 100(November):513-521.
Movember: Movember Global Annual Report. In. www.movember.com (Downloaded 18/2/2013): Movember; 2012.; 2012.
Oliffe J: Being Screened for Prostate Cancer. A Simple Blood Test or a Commitment to Treatment? Cancer Nursing 2006, 29(1):1-8.
Oliffe J, Thorne S: Men, Masculinities, and Prostate Cancer: Australian and Canadian Patient Perspectives of Communication with Male Physicians. Qualitative Health Research 2012, 17(2):149-161.
Madjar I, Denham J, Rashid P: Do women have a role in early detection of prostate cancer? Lessons from a qualitative study. AFP 2007, 36(5):375-377.
Prostate Cancer Foundation of Australia: Prostate Cancer Statistics. In. Downloaded 13/2/2013 http://www.prostate.org.au/articleLive/pages/Prostate-Cancer-Statistics.html: Prostate Cancer Foundation of Australia; 2013.
Arnold-Reed DE, Hince DA, Bulsara MK, Ngo H, Eaton M, Wright AR, Jones FR, Kaczmarczyk W, Marangou AG, Brett TD: Knowledge and attitudes of men about prostate cancer. MJA 2008, 189(6):312-314.
Slevin TJ, Donnelly N, Clarkson JP, English DR, Ward JE: Prostate cancer testing: behaviour, motivation and attitudes among Western Australian men. MJA 1999, 171(4):185-188.
Australian Interactive Media Industry Association (AIMIA): Yellow social Media Report. What Australian people and businesses are doing with social media. In. Downloaded 21/3/2013 http://about.sensis.com.au: AIMIA; 2012.
Frydenberg M, Wijesinha S: Diagnosing prostate canceer. What GPs need to know. AFP 2007, 36(5):345-347.
Australian Bureau of Statistics: Causes of Death, Australia, 2010. Leading Causes of Death by Gender. In. Downloaded 20/3/2013 http://www.abs.gov.au/ausstats/abs@.nsf/0/BBC4B00DFF0E942ACA2579C6000F6B15?opendocument#: ABS, Canberra; 2012.
Cancer Australia: Prostate cancer statistics. In. Downloaded 20/3/2013 http://canceraustralia.gov.au/affected-cancer/cancer-types/prostate-cancer/prostate-cancer-statistics: Cancer Australia; 2013.
Dillman DA: Mail and Internet Surveys. The Tailored Design Method (Second Edition). New York, Canada: John wiley & Sons, Inc.,; 2006.
Polgar S, Thomas SA: Introduction to Research in the Health Sciences (Fourth Edition). Sydney, Australia: Elsevier Churchill Livingstone,; 2005.
Pellant J: SPSS Survival Manual (4th Edition). NSW, Australia: Allen & Unwin; 2011.