Introduction
Historically and nowadays, the public hospital is still considered to be an organization that has for mission the public healthcare. Traditionally this implies that financial performance and economic profitability were merely secondary notions thus no added value was searched via the logistic process.
In Morocco, the global healthcare expenses reached 6,2% of the national GDP, they increased by 10,6% since 2006 (CNS, 2010)[1]. La. The hospital pharmacy contributes nearly for 15% of the hospital budget (Di Martinelly C., A. Guinet, R. Riane,, 2005)[2] (DELOMENIE P. and YAHIEL M.,, 1996)[3].. The medical furniture expenses are regrouped under the medical logistics function and weight heavily on the operations budget of the healthcare institutions.
The (Chow, G., Heaver and Henriksson T. L., 1994)[4] study estimates that the logistic activities represent 46% of the hospitals’ operating budget. The (Landry, S., Diaz, A., Estampe, D., Bourgeon, B., Constantin, A., Karolszyk, G., Marquot, J.F., Pedrini, S., 2001)[5] study estimates it to 30% for the west European countries (France and Netherlands). Landry and Ali (2001) conclude that the logistics budget represents a third of the hospital expenses. This rate range joins other studies like (Henning,W.K., 1980)[6] ; (Kowalski, J., 1993)[7]; (Davis, R.N., 2004)[8] who had estimated those expenses as representing 25%.
Nowadays, hospitals need to satisfy quality and care security constraints. By focusing on the pharmaceutical products management, the hospitals can come up with solution to cut costs and increase their usage value with healthcare service improvement. The costs control of the drugs acquirement can be optimized by mutualizing the purchases and the logistics problematics that had been neglected. Actually, the hospital finds itself with non-efficient storage of drugs and way more perfectible transport devices between the care units.
The healthcare sphere has placed the medical supply chain reorganization and optimization among its top priorities to address. To do so, the healthcare organizations must seek inspiration in the industrial engineering sphere that has long ago taken the same path of process amelioration approaches. The purpose of this article is modeling the hospital pharmacy processes by using the BPM model and by reconfiguring the optimized chain.
Pharmaceutical Supply Chain: State Of The Art
The impact of the hospital supply chain on the healthcare institutions is a complex process characterized by various needs, users, products and distribution channels; its mission is to control and optimize the physical, informational and financial flux from the supplier to the patients; it’s needed for the products flux and numerous hospital circuits management that are essential to these healthcare institutions.
(Council of Supply Chain Management, 2010)[9] defines logistics as follows: the process to program, implement and control the procedures for the efficient shipping and storage of goods including services and information since their originating location till their usage location in order to satisfy the client’s requirement. This definition includes incoming, outgoing, internal and external movements.
Given the pharmaceutical and production systems literatures (Arriudarre, Taillefer, Rivière &Landi, 1998)[10], (Chris Cairns, 2001)[11], (Agnès Madic., 2001)[12], (Hélène Labrosse, 2006)[13] (Yann Majchrzak & Ghislaine Dervieux, 2006)[14], (Saber Aloui, 2007)[15], (Christine Di Martinelly, 2008)[16] about the subject, the drug circuit is under the pharmacist’s responsibility and has for purpose to send the drugs to the patients or care units. The hospital drugs circuits englobe 3 stages: the prescription, the dispensation and the administration (BERETZ L., 2002)[17]. This complex system reinforces the criticality; in fact the default in such process can generate negative effects, in the extreme case, the patient death.
The Procurement Function
The recent literature is optimistic regarding the possibilities of generating some financial savings from the logistic processes amelioration even for the institutions that had already developed such systems.
(Davis, R.N., 2004)[18] announces that even healthcare institutions which are related to logistical groups, can cut their expenses, regarding the internal procurement, up to 15% by controlling the internal processes.
At the hospital level, the procurement chain is constituted of two flows: the drugs and medical devices flow and the expired flow. The direct logistic has two processes; the procurement and the care units’ resupply (preparation and shipping). The hospital pharmacist has generally two types of orders: ordinary ones (planned orders) and random orders (emergency needs). The opposite flow is constituted by the expired drugs that are shipped back by the care units to the hospital central pharmacy. The transversal logistic consists of collecting, storing in specific areas and shipping the expired products to the hospital docks.
The main actor of this supply chain is the pharmacist. He has the knowledge required to approve and reject prescriptions (as for example if there are incompatible drugs) he manages the drug storage, examines the new products and controls the procedure and analyses objectively the needs of procurement.
[1] CNS. (2010). comptes nationaux de la santé. rabat: Ministère Marocain de la santé,
[2] Christine Di Martinelly. (2008). Proposition of a framework to reengineer and evaluate the hospital supply chain. Thèse de doctorat, Institut National des Sciences Appliquées de Lyon et Facultés Universitaires Catholiques de Mons, Lyon, France et Mons, . Lyon-Mons: Thèse de doctorat, Institut National des Sciences Appliquées de Lyon et Facultés Universitaires Catholiques de Mons, Lyon, France et Mons, Belgique.
[3] DELOMENIE P. and YAHIEL M.,. (1996). Dépenses de médicaments à l’hôpital, la documentation française. Paris.
[4] Chow, G., Heaver and Henriksson T. L. (1994). Logistics performance: Definition and Measurement . International Journal of Physical Distribution and Logistics Management.
[5] Landry, S., Diaz, A., Estampe, D., Bourgeon, B., Constantin, A., Karolszyk, G., Marquot, J.F., Pedrini, S. (2001). Évaluation des coûts logistiques hospitaliers en France et aux Pays Bas. Logistique et Management, 81-87.
[6] Henning,W.K. (1980). The financial impact of materials management. Healthcare Financial Management, 36-42.
[7] Kowalski, J. (1993). Managing Hospital Materials Management,. Kowalski Dickow Associates.
[8] Davis, R.N. (2004). No more Chances for Supply Chain Savings? Look Again! Healthcare Financial Management, 68-75.
[9] Council of Supply Chain Management. (2010). Supply Chain Management Terms and Glossary. Récupéré sur Supply Chain Management Terms and Glossary.
[10] Arriudarre, Taillefer, Rivière &Landi. (1998). Intérêt de l’automatisation de la dispensation nominative journalière des médicaments. Dans l’ATC212 : réflexion au CHU d’Aix-en-Provence (pp. 41–46). ADPHRO.
[11] Chris Cairns. (2001). Robots and automation : a UK perspective. HospitalPrescriber Europe, 33–34.
[12] Agnès Madic. (2001). Informatisation du circuit du médicament à l’hôpital : de l’intention à la réalisation. Angers: Thèse de doctorat en informatique, université d’Angers.
[13] Hélène Labrosse. (2006). La dispensation nominative journalière automatisée : mise en place dans une pharmacie à usage intérieur. Lyon: Thèse de doctorat en pharmacie, université Claude Bernard – Lyon 1.
[14] Yann Majchrzak & Ghislaine Dervieux. (2006). Les nouvelles technologies au service de la sécurisation du circuit du médicament. 4th conference GISEH (pp. 183–190). Lauzanne: GISEH.
[15] Saber Aloui. (2007). Contribution à la modélisation et l’analyse du risque dans une organisation de santé au moyen d’une approche système. Paris: Thèse de doctorat, Ecole des Mines de Paris.
[16] Christine Di Martinelly. (2008). Ibidem
[17] BERETZ L. (2002). La logistique hospitalière: le point de vue de la pharmacie. Colloque “L’hôpital et la fonction logistique. Hôpital Expo.
[18] Davis, R.N. (2004). Ibidem
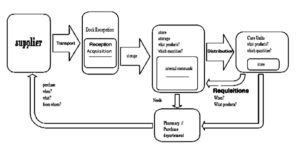
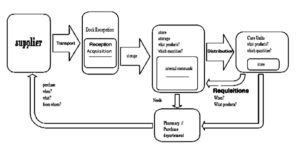
Figure 1: Pharmacy procurement decisional chain
The previous figure illustrates the decisional chain along all the stages of the pharmacy procurement circuit from the suppliers to the healthcare units.
This scheme resumes the main stages that are selection, acquisition and reception, storage, storage management and distribution. This circuit is linked to the societal and economic issues, notoriously, risks related to it and to direct and indirect costs that it generates. There is a certain progress margin in order to ameliorate it in terms of quality, security and even in a more economical plan. It’s the amelioration of the hospital business processes.
The internal drug procurement process can be described as follows: the drugs are classified and stored in the stores at the principal preparation facility of the pharmacy. The hospital health care units are replenished according to a calendar traced by the pharmacy workers. Those orders are being shipped to each care unit by its own carrier. The pharmacy is also delivering drugs specifically to some patients whom prescriptions are sent to the pharmacy by doctors to be prepared.
In this organization, the drugs are stored by a distribution automate, and the pharmacists make an inventory of the existing drugs and resupply them if necessary. The incompatibility of the system displayed data and the identified component displayed by the automate distorts the inventory results and does not allow a rapid and perfect identification of the expired drugs. These dysfunctions can stop the resupply process.
Each one of the various actors involved in this process (doctors, nurses, pharmacists, furnishers, aids, patients, etc.) have a point of view, a responsibility level, and needs that are related to the way of functioning and to the organization of the institution, thus making it more complex and impeding the efficient work of the drugs and medical devices circuit.
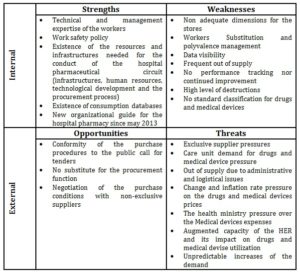
The procurement function SWOT diagnosis of the pharmaceutical supply chain, which is a strategical tool that permits to distinguish the opportunities and threats related to the external environment and the strengths and weakness of its internal value chain. This organization is the melting pot of various actors and is composed of significant and diverse quantities of therapeutical products whose complexity is highly increasing.
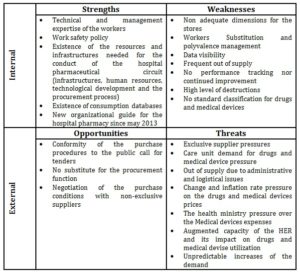
Figure 2: Pharmaceutical supply chain procurement function SWOT analysis
The lean approach identifying the value chain permits us to represent the articulation between the different care stages and optimize the transition points that are the riskiest, the numerous transversal processes that can be easily apprehended and rationalized by mapping the value chain. This approach permits us to decompartmentalize the care units by showing to each actor his place in the pharmaceutical supply chain.

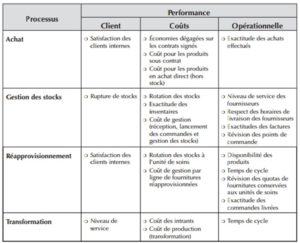
Figure 3: Procurement function value chain
The medical center managers must face more and more complex constraints. They must find new solution to answer a transforming and innovating environment. They must also develop new management decision making tools in order to pilot in a more efficient way their establishments that are under stricter budgetary pressures (Marty, C., & Merlin, H., 2007)[i].
To determinate the methods that could be applied to manage the pharmaceutical chain, it’s interesting to expose the problematic in order to determine the applicable methods. The health care sector is service production oriented and it could be profitable to establish an analogy with the industrial sector that had already pursued numerous studies in the same field. Groot et al (1993) and (Flagle D. C., 2002)[ii] have considered the hospital as a production center, with important specifications, yet identical characteristics (temporary deployment of rare resources to satisfy a critical demand and partially uncontrollable) in order to apply technics originated from the industrial area (Christine Di Martinelly, 2008)[iii],.
The core problem is the stakeholders multiplicity, the administration board that represents the funding source of the hospital and needs to be ready to answer the political and media pressures, the managers that are responsible for the hospital’s operations but are unable to completely grasp the complex reality of the clinical world, the doctors hold the true clinical decision making power but regarding their independent status, they can easily search for a better environment last but not least the nurses who know the healthcare system better than anyone of the above but had never had nor the knowledge nor the power to manage it.
The process reorganization of the healthcare chain is unavoidable. By doing so, we are looking for the best performance with the best costs regarding the technical, economic and regulatory conditions to dispense an optimal care to the patients.
The Model Demarche
The pharmaceutical supply chain complexity is linked as already pointed to the diversity of the stakeholders and the transversal flux. The 6th figure shows for each of the supply chain processes the major managing preoccupations.
It is important to understand those mechanisms. The model approach is then well suited and answers the issues of representing, communicating and analyzing the pharmaceutical supply chain. This will permit us to better understand the functioning of the system, the nature and the logic behind the interactions between the stakeholders about the actions and operations.
[i] Marty, C., & Merlin, H. (2007). Mesurer la performance des hôpitaux publics en France. Fondement méthodologiques, proposition d’un modèle d’évaluation, enjeux. cahier de recherche, HEC PARIS.
[ii] Flagle D. C. (2002). Some Origins of Operations Research in the Health. Operations Research, 52-60.
[iii] Christine Di Martinelly. (2008). Ibidem
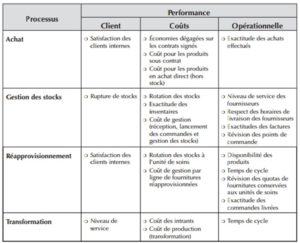
Figure 4: Pharmaceutical supply chain processes and stakeholders
As defined in the ISO 8402 and ISO 9004, the process approach is a conglomeration of inputs and outputs. Those resources can include human factor, machines, techniques and methods. This approach highlights the final purpose of organizational activities, define the contribution of each member in reaching the goals of the organization, attain customer satisfaction, interface control, dysfunction sources and finally ameliorate the organization performances.
The practice has shown that a transversal process approach leads to a better grasp of the activities and their interactions. Resources combination deployed in each stage of the process, their layout in a certain environment, can be compulsory to the final product quality. This study concentrates on the medical devices and drugs procurement process. The procurement and storage management of this operational unit is difficult because of the duality between the abundance of products and suppliers, and the user’s requirement and preferences. This demarche requires to take into consideration the external logistic network. The final goal is to optimize the pharmacy functioning, to dimension the storages, to ameliorate the storage management and to distribute efficiently pharmaceutical products. In order to attain those purposes, it’s necessary to understand the ameliorable units functioning and the various stakeholders in the drugs acquisition, storage and distribution processes.
To model those processes, we’ve chosen the business process management model. This representation is suitable to give us a standard understandable rating of all the actors in the company. Based on an “action” block chain simple logic describing the organization processes and procedures, it presents the advantage of incorporating a large number of events (error, time, stops, etc.) but also actors and data. This model permits to identify the people, the resources, the products, the actions, the logic and the chronology of the actions. The first step is to identify the system behavior, the materials that have to be generated, the actors and processes while taking into account the information and legal constraints, then to make detailed description of the actor, materials and processes, to give an explanation of the activities of the model and after that a representation of the process, the dependencies between the activities and finally to retrace the detailed information and the physical flux.
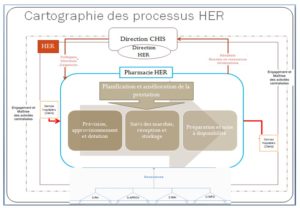
Figure 7 retraces the process mapping of the HER hospital pharmacy that allow us to identify for each process the actors, the activities (event or decisions) and the flux.
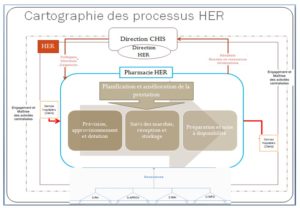
FIGURE 5: Hospital Pharmacy Process Map
The BPM approach consists of computer modeling the core processes of the company in their human and material aspects. This demarche purpose is to end with a better global view of the core processes of the system and their interactions in order to be able to optimize them, as far as possible, to maximize the automation via core applications. This BPM approach preconizes the use of an iterative and incremental methodology that permits frequent adjustments and by doing so leading to a process amelioration
This mapping helped us build a BPM model of the procurement process: preparation and availability. It has for first function to supply an understandable and standard rating of all the actors of the enterprise. Based on the simple logic of “action” block chain describing the processes and procedures of any organization, it also helps incorporating numerous events that represent a significant number of different signals (errors, time, halts) and also actors and data.
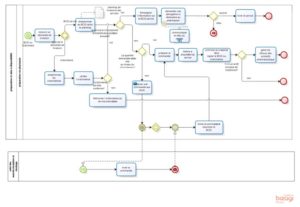
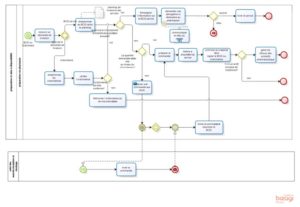
FIGURE 6: BPM model of the preparation and availability process
This model shows the drugs flux through various processes. This model permits to emphasize the major activities that are taking place in the drug circuit but also the actors and their functions that have been classified by pool (pharmacy, etc.) in order to identify their action zone. In addition, the BPM development identifies the key points of our processes on two levels: events and decisions to sort and classify them then to study and understand the impact on the activities, actors and the processes’ evolution rhythm.
Conclusion
Through this article, we have been able to describe, by using a map, the pharmaceutical products procurement and distribution system, the actors of the hospital pharmaceutical logistical circuit. Then, we SWOT analyzed the system to know its strengths, weaknesses, opportunities and threats. Finally, we did propose a BPM model to ameliorate the drug and medical devices availability. This study will lead us to position our point of view over the various stakeholders, so as to analyze, by immersion, the cultural, organizational, technical, legal, regulatory or financial dimensions that could permit us to analyze the value chain map and then identify the dysfunctions and wasted products related to the processes, the roots of the problems, and to operationally study the drug distribution scenarios.
(adsbygoogle = window.adsbygoogle || []).push({});
References
- Trivalle, C., 2014. Médicaments et ruptures de stock : il n’y a plus de laboratoire au numéro que vous avez demandé. NPG Neurologie – Psychiatrie – Gériatrie, Issue 14, p. 61—62.
- CNS, 2010. comptes nationaux de la santé, rabat: Ministère Marocain de la santé, .
- Di Martinelly C., A. Guinet, R. Riane,, 2005. Chaîne logistique en milieu hospitalier : modélisation des processus de distribution de la pharmacie. Besançon- France, s.n.
- DELOMENIE P. and YAHIEL M.,, 1996. Dépenses de médicaments à l’hôpital, la documentation française, Paris: s.n.
- Arriudarre, Taillefer, Rivière &Landi, 1998. Intérêt de l’automatisation de la dispensation nominative journalière des médicaments. Dans: l’ATC212 : réflexion au CHU d’Aix-en-Provence. l.:ADPHRO, p. 41–46.
- Chris Cairns, 2001. Robots and automation : a UK perspective.. HospitalPrescriber Europe, 33–34.
- Agnès Madic., 2001. Informatisation du circuit du médicament à l’hôpital : de l’intention à la réalisation.. Angers: Thèse de doctorat en informatique, université d’Angers.
- Hélène Labrosse, 2006. La dispensation nominative journalière automatisée : mise en place dans une pharmacie à usage intérieur.. Lyon: Thèse de doctorat en pharmacie, université Claude Bernard – Lyon 1.
- Christine Di Martinelly, 2008. Proposition of a framework to reengineer and evaluate the hospital supply chain. Thèse de doctorat, Institut National des Sciences Appliquées de Lyon et Facultés Universitaires Catholiques de Mons, Lyon, France et Mons,. Lyon-Mons: Thèse de doctorat, Institut National des Sciences Appliquées de Lyon et Facultés Universitaires Catholiques de Mons, Lyon, France et Mons, Belgique.
- Saber Aloui, 2007. Contribution à la modélisation et l’analyse du risque dans une organisation de santé au moyen d’une approche système. Paris: Thèse de doctorat, Ecole des Mines de Paris.
- Marty, C., & Merlin, H., 2007. Mesurer la performance des hôpitaux publics en France. Fondement méthodologiques, proposition d’un modèle d’évaluation, enjeux.. cahier de recherche, HEC PARIS.
- Chow, G., Heaver and Henriksson T. L., 1994. Logistics performance: Definition and Measurement. International Journal of Physical Distribution and Logistics Management.
- Landry, S., Diaz, A., Estampe, D., Bourgeon, B., Constantin, A., Karolszyk, G., Marquot, J.F., Pedrini, S., 2001. Évaluation des coûts logistiques hospitaliers en France et aux Pays Bas.. Logistique et Management, 81-87.
- Henning,W.K., 1980. The financial impact of materials management. Healthcare Financial Management, 36-42.
- Kowalski, J., 1993. Managing Hospital Materials Management,. Kowalski Dickow Associates.
- Davis, R.N., 2004. No more Chances for Supply Chain Savings? Look Again!. Healthcare Financial Management, 68-75.
- BERETZ L., 2002. La logistique hospitalière: le point de vue de la pharmacie. l., Hôpital Expo.
- Council of Supply Chain Management, 2010. Supply Chain Management Terms and Glossary.
- Flagle D. C., 2002. Some Origins of Operations Research in the Health. Operations Research, 52-60.
- Yann Majchrzak & Ghislaine Dervieux, 2006. Les nouvelles technologies au service de la sécurisation du circuit du médicament. Lauzanne, GISEH, p. 183–190.