Discussion
Recently, supersonic wave coagulation cutting devices and new energy devices such as LigaSureTM have been used for many operations. However, so far traditional methods like the hand ligation technique and the bipolar electrode knife have mainly been used in parotid gland surgery to avoid facial nerve damage. Therefore, the operation is lengthy, and there are risks such as postoperative bleeding and salivary fistulas when the ligations become loosened. Moreover, ligature left inside the body can pose a risk of postoperative infection. Also, the electrode knife used during parotid gland surgery is well known for its potential to cause nerve damage by heat and direct electric current. Moreover, the possibility of heat damage from the ultrasonic wave surgical knife has also been pointed out (Kim et al., 2008). LigaSureTM Small Jaw could be used instead of hand ligation, because it was reported that heat damage was comparatively slight (Seehofer et al., 2012).
LigaSureTM Small Jaw is called a vessel sealing system. Collagen and elastin are denatured, and then the intravascular lumen is occluded; it fuses the vessel walls, and the blood stream is intercepted. First of all, LigaSureTM Small Jaw senses the tissue at the point of the device, and the best pressure is applied; the main body of LigaSureTM measures the tissue impedance, and an appropriate energy setting is selected. In addition, feedback control and high frequency energy is supplied, and the output is adjusted automatically. The output also automatically stops when the seal is completed, and the tissue is cut with the attached surgical knife by the surgeon’s hand. Generally, heat damage to tissue is believed to spread wide if the voltage is high, like with the electrode knife, and the current is low. Inversely, it is supposed that protein will fuse and integrate in a short time and scorching is suppressed because of the high current and the decreased voltage in LigaSureTM Small Jaw. A lot of experiences of the efficacy of LigaSureTM have been reported in chest, gynecological, gastroenterological, urological surgeryand so on (Levy and Emery, 2003; Leonardo et al, 2005; Tsunezuka et al., 2010; Gehrig et al., 2011).Recently, the number of reports about using ultrasonic wave coagulation cutting devices and an advanced bipolar device such as LigaSureTM has increased for thyroid surgery in the head and neck region (Prokopakis et al., 2010). As for LigaSureTM Small Jaw used in parotid gland surgery, no report has been made until now as far as we could find. We have clinically and histologically examined the effect of using LigaSureTM Small Jaw in parotid gland surgery.
As a comparison with parotid gland surgery using LigaSureTM Small Jaw, ten consecutive cases of parotid benign tumour surgery in our department using the hand ligation technique were examined. The average operation time was 165 minutes, the average amount of bleeding was 15.6ml, and the average drain custody period was 3.2 days with this conventional method. On the other hand, the average operation time was 140 minutes, the average amount of bleeding was 41 ml, and the average drain custody period was 3.0 days using LigaSureTM Small Jaw. Although the cases were limited in number, there was no significant difference between the two groups. However, shortened operation time using LigaSurePreciseTM compared with the traditional methods has been reported. It was considered that because bigger and deeper lobes of parotid gland tumour were included in the LigaSureTM Small Jaw group, therefore excessive blood loss was experienced in these cases compared with the traditional method cases. On the other hand, less bleeding has been reported when using LigaSurePreciseTM than the traditional methods, especially in patient who are at risk of haemorrhage (Prokopakis et al., 2005; Colella et al., 2005). The United States FDA (US Food and Drug Administration) authorizes LigaSureTM for cutting blood vessels and lymphatic vessels up to 7mm in diameter, and the resisting pressure is reported to be three times or more than usual arterial pressure (Kennedy et al., 1998; Heniford et al., 2001; Harold et al., 2003; Dubuc-Lissoir, 2003).Therefore, it was suggested that less bleeding was accomplished. Secure sealing of the salivary duct was also expected in the same way. We had one case of salivary fistula among the ten traditional method cases. Therefore, it was thought that a further investigation would be required concerning salivary fistulain parotid gland surgery using LigaSureTM Small Jaw.
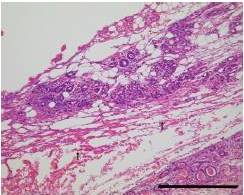
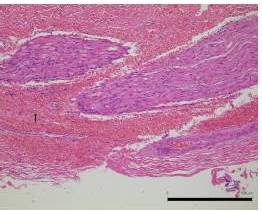
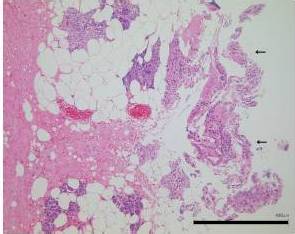
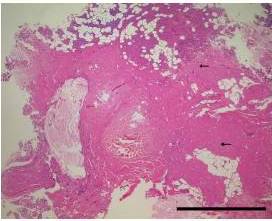
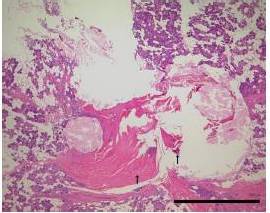
It was mentioned in previous reports (Kennedy et al., 1998; Heniford et al., 200; Harold et al., 2003; Dubuc-Lissoir, 2003) on LigaSureTM use that heat was transmitted from the device to the surrounding structures to the extent of about 1.5-3.3mm. Cell denaturation was limited to about 1mm of the surrounding tissues in our investigation of damage by LigaSureTM Small Jaw to the cutting stump. Preservation of the facial nerve was thought to be possible, if there was a distance of 1mm or more between the cutting edge and the facial nerve. It was reported that facial palsy was also a rare complication after parotid gland surgery using LigaSurePreciseTM (Prokopakis et al., 2005; Colella et al., 2005).
Previous reports said the operation time with LigaSurePreciseTM was shortened. This was supposed to be due to the omission of hand ligation time. Similar to the previous report, in our cases operation time with LigaSureTM had a tendency to be shorter, although the difference was not significant because of the limited number of cases.
Although there were no clinical or histology investigations about its use in parotid gland surgery so far, LigaSureTM Small Jaw was thought to be as a useful device as LigaSurePreciseTM was reported to be in the past. Regarding complications of parotid gland surgery using LigaSureTM Small Jaw and damage to near organs, coexisting complications such as facial palsy, salivary fistulas and postoperative bleedings were not identified in our study, but the number of cases was limited. According to past reports on LigaSurePreciseTM and our study, LigaSureTM Small Jaw has the potential to reduce complications and shorten operation time. Further research is necessary to investigate the cost-effectiveness of LigaSureTM Small Jaw.
Conclusion
In this study, complications of parotid gland surgery using LigaSureTM Small Jaw are not identified, though the number of cases is limited. Moreover, histological examination reveals less damage to the nerve at the cut edge of the connective tissue, nerve and salivary gland in the LigaSureTM Small Jaw group. Our findings indicate that LigaSureTM Small Jaw is a safe and useful device for parotid gland surgery.
(adsbygoogle = window.adsbygoogle || []).push({});
References
Colella, G. & Giudice, A. (2006). “LigaSure Device in Parotid Gland Surgery,” Otolaryngol Head Neck Surg, 135, 172-173.
Publisher – Google Scholar
Colella, G., Giudice, A., Vicidomini, A. & Sperlongano, P. (2005). “Usefulness of the LigaSure Vessel Sealing System during Superficial Lobectomy of the Parotid Gland,” Arch Otolaryngol Head Neck Surg, 131, 413-416.
Publisher – Google Scholar
Dubuc-Lissoir, J. (2003). “Use of a New Energy-Based Vessel Ligation Device during Laparoscopic Gynecologic Oncologic Surgery,” SurgEndosc, 17, 466-468.
Publisher – Google Scholar
Gehrig, T., Müller-Stich, B. P., Kenngott, H., Fischer, L., Mehrabi, A., Büchler, M. W. & Gutt, C. N. (2011). “LigaSure versus Conventional Dissection Technique in Pancreatoduodenectomy: A Pilot Study,” Am J Surg, 201, 166-170.
Publisher – Google Scholar
Harold, K. L., Pollinger, H., Matthews, B. D., Kercher, K. W., Sing, R. F. & Heniford, B. T. (2003). “Comparison of Ultrasonic Energy, Bipolar Thermal Energy, and Vascular Clips for the Hemostasis of Small-, Medium-, and Large-Sized Arteries,” SurgEndosc, 17, 1228-1230.
Publisher – Google Scholar
Heniford, B. T., Matthews, B. D., Sing, R. F., Backus, C., Pratt, B. & Greene, F. L. (2001). “Initial Results with an Electrothermal Bipolar Vessel Sealer,” SurgEndosc, 15, 799-801.
Publisher – Google Scholar
Kennedy, J. S., Stranahan, P. L., Taylor, K. D. & Chandler, J. G. (1998). “High-Burst-Strength, Feedback-Controlled Bipolar Vessel Sealing,” SurgEndosc, 12, 876-878.
Publisher – Google Scholar
Kim, F. J., Chammas, M. F. Jr., Gewehr, E., Morihisa, M., Caldas, F., Hayacibara, E., Baptistussi, M., Meyer, F. & Martins, A. C. (2008). “Temperature Safety Profile of Laparoscopic Devices: Harmonic ACE (ACE), Ligasure V (LV), and Plasma Trisector (PT),” SurgEndosc, 22, 1464-1469.
Publisher – Google Scholar
Leonardo, C., Guaglianone, S., De Carli, P., Pompeo, V., Forastiere, E. & Gallucci, M. J. (2005). “Laparoscopic Nephrectomy Using Ligasure System: Preliminary Experience,” Endourol, 19, 976-978.
Publisher – Google Scholar
Levy, B. & Emery, L. (2003). “Randomized Trial of Suture versus Electrosurgical Bipolar Vessel Sealing in Vaginal Hysterectomy,” Obstet Gynecol, 102, 147-151.
Publisher – Google Scholar
Prokopakis, E. P., Lachanas, V. A., Helidonis, E. S. & Velegrakis, G. A. (2005). “The Use of the Ligasure Vessel Sealing System in Parotid Gland Surgery,” Otolaryngol Head Neck Surg, 133, 725-728.
Publisher – Google Scholar
Prokopakis, E. P., Lachanas, V. A., Vardouniotis, A. S. & Velegrakis, G. A. (2010). “The Use of the Ligasure Vessel Sealing System in Head and Neck Surgery: A Report on Six Years of Experience and a Review of the Literature,” B-ENT, 6, 19-25.
Publisher – Google Scholar
Schiphorst, A. H. W., Twigt, B. A., Elias, S. G. & van Dalen, T. (2012). “Randomized Clinical Trial of LigaSure versus Conventional Suture Ligation in Thyroid Surgery,” Head Neck Oncol, 18, 4, 2.
Publisher – Google Scholar
Seehofer, D., Mogl, M., Boas-Knoop, S., Unger, J., Schirmeier, A., Chopra, S. & Eurich, D. (2012). “Safety and Efficacy of New Integrated Bipolar and Ultrasonic Scissors Compared to Conventional Laparoscopic 5-mm Sealing and Cutting Instruments,” SurgEndosc, 26, 2541-2549.
Publisher – Google Scholar
Tsunezuka, Y., Waseda, R.- I. & Yachi, T. (2010). “Electrothermal Bipolar Vessel Sealing Device LigaSureV for Pulmonary Artery Ligation–Burst Pressure and Clinical Experiences in Complete Video-Assisted Thoracoscopic Major Lung Resection for Lung Cancer,” ThoracSurg, 11, 229-233.
Publisher – Google Scholar