Gingival Fibrous nodules or gingival nodules are variants of normal oral mucosa. These lesions were apparently identified and named by Giunta in 1999, who reported a series of five cases and additional three cases were later reported by Brannon and his co worker. These appear as either single or multiple firm, pale nodules occurring on the labial attached gingiva-alveolar mucosa junction of either arches. They are non mobile and tend to be present for a long time. No complications of these lesions have been reported. Much information and literature regarding this entity is lacking, even after a decade after the initial publication. This paper reports four new cases of gingival fibrous nodules. Clinically it is important to recognize these as they mimic certain disease process as well.
Case History
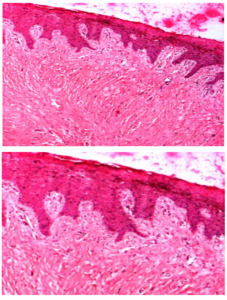
Case 1: A 24 year old male visited the Department for a routine dental check up. His medical/surgical/personal histories were unremarkable. Incidentally, the mandibular anterior region on the labial aspect showed multiple, small, slightly elevated, pink-white nodules, at the junction of marginal gingiva — alveolar mucosa, each measuring about 2-3 mm in size. They were firm in consistency, non mobile and non tender [Fig 1]. Intra oral periapical radiograph in the region showed no abnormalities. They were diagnosed as gingival fibrous nodules and excisional biopsy of one of the lesions was performed which showed non ulcerated stratified squamous epithelium and underlying connective tissue showed collagenous fibres with a few fibroblasts [Fig 2, 2a]. There was no evidence of cellular atypia. The histopathology was consistent with the clinical impression.
Fig 1: Case 1 Showing Multiple GFNs on the Mandibular Anterior Muco-Gingival Junction on the Right Side
Fig 2 and 2 (a): H&E (Low and High Power) Sections Showing Intact Epithelium and Connective Tissue Showing Collagen Bundles
Case 2: A 31 year old male visited the Department with a complaint of decay in the lower front tooth. His medical/surgical/personal histories were unremarkable. On examination, the mandibular right central incisor had initial distal caries. Also, the mandibular anterior region on the labial aspect showed two, slightly elevated, pale pink nodules, at the junction of marginal gingiva — alveolar mucosa, each measuring about 2-3 mm in size. They were firm in consistency, non mobile and non tender [Fig 3]. The patient was questioned if he was aware of the lesions for which the answer was negative. Intra oral periapical radiograph in the region showed no abnormalities. The clinical impression was that of gingival fibrous nodules. Biopsy was not performed on the lesions as the clinical presentation was similar to the previous case.
Fig 3: Case 2 Showing Multiple GFNs on the Mandibular Anterior Muco-Gingival Junction
Case 3: An 18 year old male visited the Department with a complaint of irregularly placed lower front teeth. His medical/surgical/personal histories were unremarkable. On examination, crowding of lower anterior teeth were noted, along with the multiple, elevated, whitish nodules, at the junction of marginal gingiva — alveolar mucosa, each measuring about 3-4 mm in size. They were firm in consistency, non mobile and non tender [Fig 4]. Intra oral periapical radiograph in the region showed no abnormalities. The patient was unaware of the lesions. The clinical impression was that of gingival fibrous nodules. Excisional biopsy of one of the lesions was performed which showed non ulcerated stratified squamous epithelium and underlying connective tissue of collagenous fibres with fibroblasts, consistent with the clinical impression.
Fig 4: Case 3 Showing Multiple GFNs on the Mandibular Anterior Muco-Gingival Junction on the Right and Left Sides
Case 4: A 45 year old male visited the department with a complaint of deposits over his teeth. The patient was hypertensive and was on Telmisartan 20 mg. Intra oral examination showed generalized gingivitis. Incidentally, the maxillary right anterior gingiva region showed two elevated, pink nodules, at the junction of marginal gingiva — alveolar mucosa, each measuring about 3-4 mm in size. They were firm in consistency, non mobile and non tender [Fig 5]. Intra oral periapical radiograph in the region showed no abnormalities. The patient was totally unaware of the lesions. The clinical diagnosis was that of gingival fibrous nodules. Biopsy was planned, but the patient declined the procedure citing the asymptomatic nature of the lesions.

Fig 5: Case 4 Showing Two GFNs on the Maxillary Anterior Muco-Gingival Junction on the Right Side
Discussion
Oral cavity demonstrates a wide variety of lesions. They range from normality to normal variations to pathologies. The primary responsibility of a clinician is to not only identify the pathologies but also to detect the normal variations. One among the many normal variants of the oral cavity is the Gingival Fibrous Nodules (GFN).
Gingival fibrous nodules are normal variants of the oral mucosa which appear as solitary or multiple, slightly raised, yellowish nodules, located on the attached gingiva — alveolar mucosa junction being firm in consistency, non tender and non mobile [1].
Terminology: Although it was Giunta who first identified, investigated and coined the term Gingival Fibrous Nodules for the lesions, these were apparently identified as normal variants, the reference of which can be found in Burket’s text book of Oral Medicine [2]. Brannon and his co worker have suggested the name mucogingival papule for these lesions as they are more papular and are consistently located at the mucogingival junction [3].
Etiopathogenesis: the lesions are considered as normal variants and are similar to other collagenous normal variants of the oral cavity such as retro cuspid papillae [1, 3]. Hence, a definite etiopathogenesis has not been defined. It has been suggested that they are nothing more than accentuated anatomy, giving the peculiar appearance [3].
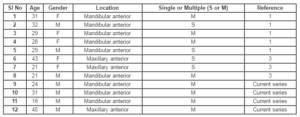
Epidemiology: Analysis of the all reported cases including the present case was done. The demographics are summarized in table. Accordingly, a total of 12 cases of GFN are available. The exact prevalence of this entity is yet to be determined. Out of these 12 cases, it appears as though it is more common in males (Males = 7 and Females = 5) and is found in younger subjects of about 25-30 years of age and is slightly uncommon after the fourth decade. No racial predilection is noted. These are found on the labial gingiva of either maxilla or mandible, although the mandible appears to be a favoured location, located along the muco-gingival junction [1, 3]. No additional inference could be drawn from the analysis.
Clinical Features: GFNs clinically appear as pink-white, slightly elevated solitary or multiple nodules or papules with smooth surface, which are solid and firm in consistency while the size may range from 1-4 mm. They are well defined, non tender and non mobile. They are entirely asymptomatic and rarely subjects will be aware about their presence. Generally these lesions are long of long duration. . Radiographically no bony changes will be evident.
Clinical Differential Diagnosis: A few disease processes can mimic GFNs in their clinical appearances. They include the bony exostosis, gingival cysts [4], multiple hamartomas, and gingival manifestations of tuberous sclerosis [5], papillomas and fibromas [6]. These lesions although rarely resemble GFN, based on their clinical manifestations differentiation can be made from GFNs.
Exostosis appears as hard nodules on palpation though on visual examination may appear similar to GFN. Gingival cysts may be firm to fluctuant, due to presence of fluid underneath and occur as single lesion unlike GFN [1].
Epulides are localized tumour-like gingival enlargements which are non- neoplastic. Most arise from the interdental gingiva unlike GFNs which arise much inferiorly. Subgingival plaque and calculus may cause chronic irritation may initiate the formation of epulides. Fibrous, vascular and giant cell epulides are the three common types. The fibrous epulis in particular appears as a solitary, sessile or pedunculated mass on the gingiva, of varying size, with histopathology similar to GFNs but with predominant plasma cell infiltrate which is rarely seen in GFNs. Further, amorphous calcifications or trabeculation of bone is found in 1/3 of the cases [7].
Histopathology: Under H&E stain, the lesions show accumulation of dense collagen tissue underlying stratified squamous cell epithelium with absence of inflammation [1,3]. Histopathologically, although it is mentioned that tuberous sclerosis may resemble GFNs, the clinically manifestations of the spectrum are quite different [1].
Management: Since these lesions are variants of normal mucosa, no special management would be necessary [1, 3]. Biopsy can be performed to rule out the possibility of any other disease process. It is also stated that once these lesions are recognized clinically, biopsy could be avoided [1].
Recurrence: Two out of the five cases reported by Giunta showed recurrence. It has been proposed that the reason for a normal variant of the mucosa to recur following surgical excision is nothing but a repair process of re-establishing the surgical defect [3].
Analysis of GFN Reported in the Literature Including the Present Case
Table: Demographics of Gingival Fibrous Nodules
1. Giunta L J. (1999). Gingival fibrous nodule. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 88:451-4.
Publisher
2. Lynch M A, Brightman VJ and Greenberg MS. (1997) Burket’s Text book of Oral Medicine: Diagnosis and Treatment, 9th ed, Lippincot-Raven, Philadelphia,USA, pg 156
3. Brannon RB and Pousson RR. (2003) Gingival fibrous nodule- anomaly or pathology? . J Dent Hyg,77(1):50-52
4. Hata T, Irei I, Hosoda M, Mandai T, Ishida K, Ito S et al. (2009) Secondarily developed gingival cyst of the adult : A case report. Kawasaki Medical Journal, 35:333-35
Google Scholar
5. Harutunian K, Figueiredo R, Gay-Escoda C. (2011) Tuberous sclerosis complex with oral manifestations: A case report and literature review. Med Oral Patol Oral Cir Bucal.16:e478-81.
Publisher – Google Scholar
6. Rossmann J A. (2011). Reactive Lesions of the Gingiva: Diagnosis and Treatment Options. The Open Pathology Journal, 5, 23-32.
Publisher – Google Scholar
7. Soames J. V. and Southam J. C. (2005) Oral Pathology, 4th Ed, Oxford University Press Inc., New York, USA, pg 119-122