Introduction
Amyloidosis is a rare disease. We presented a case of an idiopatic isolated intestinal amyloidosis without extraintestinal manifestations that caused episodes of intestinal pseudo-obstruction and a severe duodenitis with gastrointestinal bleeding. The diagnosis was supported by pathologyc findings.
Case Report
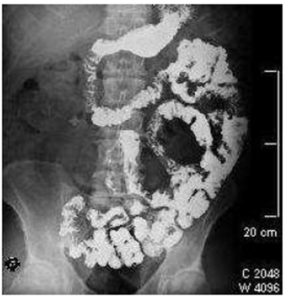
We presented a case of A 54 year old Hispanic male with recurrent episodes of abdominal distension and up to three previous hospitalizations with a diagnosis of partial bowel obstruction that resolved with conservative management. The physical examination revealed overweight (BMI= 28 Kg/m2). A colonoscopy was performed with the discovery of three hyperplastic polyps, and barium small bowel radiographic studies showed folds thickening of jejunal and ileal loops (Fig. 1).
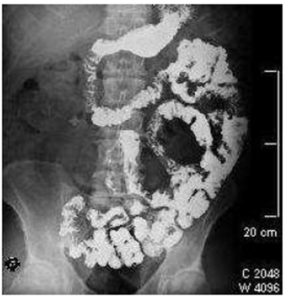
Figure 1: Small bowel radio graphics with barium. Morphological changes of jejunal bowel loops are shown that explain the symptoms of partial intestinal obstruction experienced by the patient
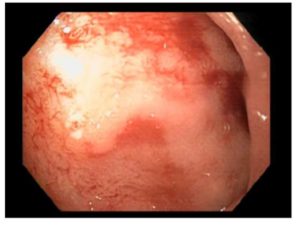
In upper endoscopy, a hemorrhagic duodenitis was found with active bleeding by a visible vessel that was stopped after combined endoscopic therapy (Fig. 2 and 3).
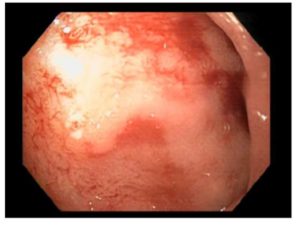
Figure 2: Upper endoscopic findings A visible vessel after endoscopic therapy located in the
duodenal bulb is observed
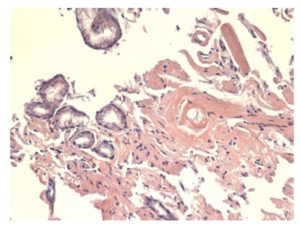
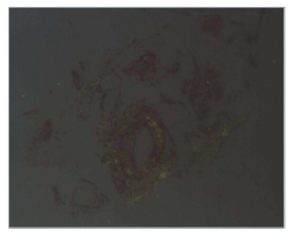
The blood cell count was normal, and celiac serological tests were negative. After a month, there was an endoscopic control with evidence of severe duodenitis, and biopsy revealed hyaline deposits in the walls of blood vessels and extravascular area positive for Congo red staining with birefringence under polarized light (Fig. 4 and 5).

Figure 3: Upper endoscopic findings The descending duodenum is edematous with recent
bleeding due to intestinal amyloidosis
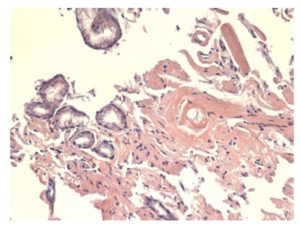
Figure 4: Microscopic findings (x400) Deposits of hyaline material were identified in extravascular area that resulted in a positive reaction using the Congo red stain
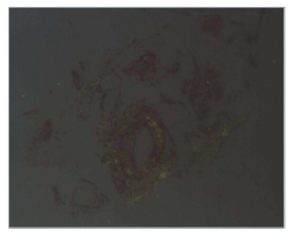
Figure 5: Microscopic findings Birefringence of amyloid deposits under polarized
light after Congo red staining is observed
Laboratory tests and images were completed without finding secondary etiology of amyloidosis or other organ involvement. Currently, the patient is maintained with prokinetic agents that may benefit dysmotility-related symptoms. He has not had a recurrence of intestinal pseudo-obstruction.
Discussion
Amyloidosis is a rare disease that is caused by an abnormal extracellular deposition of fibrillar protein wiht typical pathologic properties, and it could be systemic or localized to a single organ, such as the gastrointestinal tract. Primary amyloidosis (monoclonal immunoglobulin light chains) is the most common form of amyloidosis with amyloid deposition in the muscularis mucosae, submucosa, and muscularis propria leading to the thickening of intestinal folds, and it usually presents with constipation, mechanical obstruction, or chronic intestinal pseudo-obstruction like this case. Whereas, secondary amyloidosis (serum acute phase-reactant, amyloid A protein) has been related to fine granular appearance and mucosal friability with erosions, because deposition occurs mainly in the propria mucosae with symtomps of diarrhea. There are no pathognomonic radiologic or endoscopic findings, and diagnosis could be delayed. Therefore, intestinal amyloidosis should be considered among differential diagnoses of severe duodenitis with complications. Only a few reports of hemorrhagic intestinal amyloidosis have been published.
This case was a localized intestinal amyloidosis without evidence of systemic disease or an associated plasma cell discrasia. Histologic analysis showed no significant patological changes in the duodenal mucosa, but the presence of amyloid deposits in additional cuts in the submucosa. Although we did not identify the type of amyloid, patients with these clinicopathological features correspond to primary amyloidosis and should be treated symptomatically, because the rate of progresion is low and they have excellent survival without systemic therapy.
The treatment of primary amyloidosis includes myeloma-type chemotherapy with variable outcomes; whereas in secondary amyloidosis, it includes control of the primary disease. Gastrointestinal tract surgery should be performed only if the benefits clearly outweigh the risks. Herein, we presented an infrequent case of intestinal amyloidosis with an impact on the quality of life.
Potential conflict
The author worked in Clinica Ricardo Palma, but actually is working at Hospital Edgardo Rebagliati Martins (EsSalud) in Lima, Perú nal tract”. Nat Rev Gastroenterol Hepatol 6: 608-617
References
1. Cowan AJ, Skinner M, Seldin DC, Berk JL, Lichtenstein DR, O’Hara CJ, Doros G, Sanchorawala V. (2013).“Amyloidosis of the gastrointestinal tract: a 13-year, single-center, referral experience”. Haematologica 98(1): 141-6.
Publisher – Google Scholar
2. Ebert EC, Nagar M. (2008). “Gastrointestinal manifestations of amiloidosis”. Am J Gastroenterol 103: 776-787.
Publisher – Google Scholar
3. Hokama A, Kishimoto K, Nakamoto M, Kobashigawa C, Hirata T, Kinjo N et al. (2011). “Endoscopic and histopathological features of gastrointestinal amiloidosis”. World J Gastrointest Endosc 3(8): 157-161.
Publisher – Google Scholar
4. Kim YJ, Kim HS, Park SY, Park SW, Choi YD, Park CH et al. (2012). “Intestinal Amyloidosis with intractable diarrhea and intestinal pseudo-obstruction”. Korean J Gastroenterol 60: 172-176.
Publisher – Google Scholar
5. Sattianayagam PT, Hawkins PN, Gillmore JD. (2009). “Systemic amyloidosis and the gastrointesti
Publisher – Google Scholar