Introduction
The Montreal Cognitive Assessment test (MoCA) is a brief screening instrument that assesses a wide range of cognitive functions (such as executive functions, visuospatial abilities, Naming, memory recall, Digit span, Sentence, abstract reasoning and orientation) necessary for Mild Cognitive Impairment (MCI) and dementia diagnosis (Nasreddine et. al 2005). The test time is estimated in 20 minutes and the maximum possible score is 30 points. The cuttoff point to MCI is 26 points and a score above 26 is considered normal (Nasreddine et al., 2005). Nasreddine et. aI. (2005) presented in the original study 87% specificity test in excluding normal elderly and 90% sensitivity to detect MCI. Also, the sensitivity to detect AD cases with MoCA was 100% (Nasreddine et al. Al 2005). Due to their psychometric characteristics and utility in these cases, this test was validated and adapted in different countries (Rahman et al, 2009; Sarmento, 2009; Tsai, et al, 2011; Freitas, et al, 2011). In Brazil, the recent study of Memória (2012) provided good psychometric characteristics to this test.
According to the new diagnostic criteria for the investigation of AD, the use of neuropsychological tests can increase the comprehension on the preserved capacities of these elderly, helping to adjust treatment (Albert et al, 2011; McKhann et al, 2011). It is known the existence of several screening tests in the field of gerontology and usually those with a greater precision are used (Heinik et al. Ai. 2004). Despite, Nasreddine et. aI. (2005) discusses the current concepts of aging, especially MCI and points out that new assessment tools become essential for these population, considering MCI as a recognized problem with specific diagnostic criteria and that implies a high risk of progression to AD. Within this context, the MoCA has been suggested as an effective instrument to help screening MCI and AD diagnosis (Nasreddine et. Al 2005). Its simplicity and fast administration makes it usefull in clinics and hospitals, facilitating the healthcare team work once it covers the majority of cognitive domains and have a high sensitivity to MCI (Nasreddine et . al 2005). According to Nasreddine et. al. (2005) MoCA intends to fulfill an urgent need which had not been answered by other screening instruments available to detect MCI patients and differentiate them from normal and AD elderly.
Hence, investigate its utility in differentiating AD, MCI and control elderly in a brazilian sample assumes relevance, especially with elderly with more than four years of educational level, once this is a important variable in AD and MCI diagnostic. Several studies suggests problems in differentiate cognitive functions on AD and MCI elderly with higher educational levels, because of ceiling effect of some cognitive tests (Cecato et al, 2012; Fuzikawa et al, 2007; Aprahamian et al, 2010) increasing the importance of the present study.
Thus, considering the importance of early diagnostic of demential syndromes, as well as, the importance of MOCA as a diagnostic test for dementia and MCI, a widely used instrument in the world, the aim of this study was to analyze the MOCA utility in differentiating MCI, AD and control elderly with more than four years of educational level.
Method
The cross-sectional study occurred in the Institute of Gerontology and Geriatrics in Brazil and initiated in April 2010 and ended in December 2012. 136 elderly subjects aged over 60 years, both genders and educational level over 4 years, were studied. This sample was composed of three diagnostic groups that are better described bellow.
Patients with other demential syndromes such as vascular dementia, temporal frontal dementia, Lewy bodies, or any other clinical frame that would suggest non-Alzheimer’s dementia were excluded from the sample. We also adopted as exclusion criterion patients with severe dementia (Clinical Dementia Rating ≥ 3) (Hughes et. Al., 1982), with a stroke story, both hands paralysis, major depressive disorder, Parkinson’s disease, tremors, severe hearing and visual impairments and less than 4 years of schooling.
The diagnostic criteria for dementia, were based on DSM-IV (APA, 1994) and NIA-AA (National Institute on Aging – Alzheimer Association) AD criteria (McKhann, et al. Ai. 2011). For the diagnosis of MCI, Petersen et. al. (2001) criteria were used. The study included only patients with amnestic MCI, which means only elderly with memory impairment. The inclusion criteria included not having DLA (Daily living activities) problems, not fulfill demential syndrome criteria in cognitive assessment and not having cognitive complaints. Moreover, we adopted the 1.5 standard deviation criteria suggested by Petersen et. al. (2001), in MMSE and CAMCOG memory subtests based on its normative population. Considering the many different MCI criteria (Memória, 2012), we adopted Petersen´s et. al. (2001) and a detailed clinical evaluation made by a experienced gerontologist and included in the sample only MCI patients in which agreement in these two were found.
As MoCA scores were considered as depenJMED variables in the present study, it was not used as diagnostic criteria. All AD and MCI diagnostics as well as neuropsychological assessment were made by a experienced Gerontologist. Neuroimaging and other neurological exams were made to investigate whether the participants fulfilled inclusion criteria, i.e. did not have any other neurological problems that justified the symptoms. The inclusion criteria for the control group (CG) were scoring above the cutoff points on neuropsychological tests, have no dementia symptoms, GDS score lower than 7 and not have problems to perform daily living activities.
Instruments and Procedures
All patients were submitted to detailed clinical and neuropsychological screening evaluation. Neuropsychological tests applied were Cambridge Cognitive Examination (CAMCOG) (Roth, et. Al., 1986), MiniMental State Examination (MMSE) (Folstein, et. Al., 1975), the Clock Drawing Test (CDT) (Mendez, et. al., 1992; Shulman, et. al., 1993), Brazilian version of MoCA (Sarmento, 2009), Geriatric Depression Scale (GDS) with 15 short items (Yesavage, et. al., 1983), Pfeffer Functional Activities Questionnaire (PFAQ) (Pfeffer, et. al., 1982) and verbal fluency test (Brucki, et. al., 2003).
CAMCOG is a cognitive battery that integrates the Cambrigde Mental Desorders of the Elderly Examination (CAMDEX), developed by Roth, Tym, Mountjoy, Huppert, Hendrie, Verma and Goddard (1986). The maximum score is 107 and the cutoff point to dementia is 80 points. Its subtests assesses memory, Digit span, concentration, Sentence, praxis, abstract thought and perception.
MMSE were developed by Folstein, Folstein and Mchugh, in 1975 and have a maximum score of 30 points with cutoff points for dementia varying with patients educational level. Verbal Fluency is one of the simplest tests to assess cognitive impairment in initial phases of demential syndrome (Henry & Crawford, 2004). Brucki, Nitrini, Caramelli, Bertolucci and Okamoto (2003) suggests cutoff points according to schooling years and vary from 9 to 13 points. The semantic type was employed in fruit category, and in words with M, the phonemic type was used. The CDT criteria were based on Mendez and Shulman.
After the clinical and neuropsychological evaluation we performed an interview with an informant or a relative with daily contact with the respective elderly in order to report possible symptoms and add other relevant information such as behavioral changes. All patients were submitted by MoCA test after been diagnosed.
Statistical Analysis
To consider the sample calculation we used a 5% significance level and sample error (confidence interval).The minimum number of participants would be equal to 101. The collected sample from April 2010 to December 2012 totalized 136 participants, reaching the minimum sample size required.
All collected data were analyzed by SPSS 15.0 system (2007). Firstly, descriptive statistics concerning the sample distribution (age, gender and education level), setting a significance level of 5% were made. The variables were described by using frequencies and means with standard deviations.
We also calculated the accuracy of MoCA, MMSE, CAMCOG and CDT by ROC curve methodology. Mostly of measures with exception of Numbers and Pointers had abnormal distribution, assessed by means of Kolmogorov Smirnov normality test. Hence, we choosed to employ non parametric tests to evaluate group differences. In addition, we used the chi-square (x2) and Kruskall Wallis test to compare MoCA scores between CG, MCI and AD in order to check which subitems presents significant differences between groups. After that Manova were used to look for differences between the three groups regarding MoCA measures to control Type I error.
Results
From the 136 participants, 52 elderly (38.2%) received a diagnosis of Alzheimer’s disease, 45 (33.1%) of Mild Cognitive Impairment and 39 elderly (28.7%) comprised the control group (CG). Most of sample were women, (89, 65.4%), and the mean age was equal to 75.74 years (± 7.38) (minimum = 60, maximum = 92). The sample has a higher number of elderly people with more than 9 years of study. (58.8%).
The CG mean age was equal to 71.82 years (± 6.89) (minimum = 60, maximum = 89), with 74.4% women and mean educational level of 7 years (SD=1,75). The AD group showed mean age of 77.92 years (± 6.97) (minimum = 64, maximum = 91) with women comprising 63.5% and mean educational level of 7 years (SD=1,80). MCI participants have had a mean age of 76.60 years (± 7.06) (minimum = 63, maximum = 92), with 60% women and mean of 6 schooling years (SD=1,94). The frequency of the variables age, sex and education shows the large participation of women in the three diagnostic groups and higher mean age in the AD group.
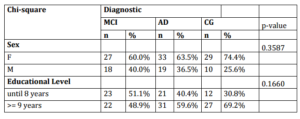
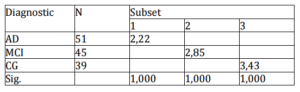
In spite of the different educational levels (X2=9,15; p=0,517) and age range (X2=7,35; p=0,356) of the three groups, they did not provided significant differences. The sex frequencies also did not differ significantly between groups with all of them having a predominancy of women. This research was approved by the Ethics Research Committee (process number 54/11). Table 1 shows these results.
Table 1. Groups Demographic Data Comparison
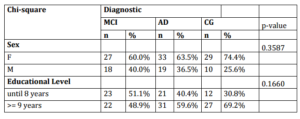
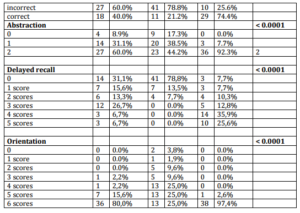
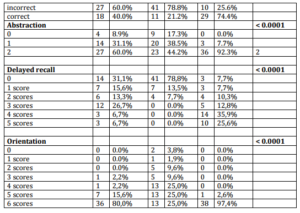
In Table 2 its ascertain significant differences in MoCa sub tests Trails (p <0.0001), contour of the clock drawing test (p = 0.0116), Numbers and Pointers (p <0.0001), Rhinos Naming (p = 0.0004), Digit Span Forward (p <0.0001), Backward (p = 0.0105), Serial 7 (p <0.0001), Sentence (p <0.0001), Abstraction (p <0.0001), Delayed recall (p <0.0001) and Orientation (p <0.0001).
The higher error rate and the lowest scores are observed in AD group, while success rates are higher in MCI and CG. CG have had the highest percentage of success in sub tests. The MoCA sub tests that were not able to differentiate diagnostic groups were Cube (p = 0.1559), Leon Naming (p = 1.000) Camel / Dromedary Naming (p = 0.0639) Letter (p = 0.3674). On these sub tests there are similar percentages of correct answers in the three diagnostic groups, except the Cube which presents a similar percentage of errors between MCI and AD.
Table 2 – Analysis of the Moca Items in Relation to Diagnostic Groups

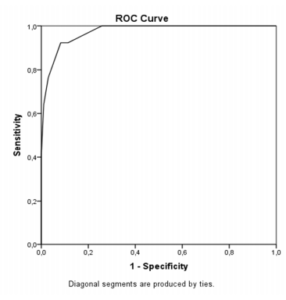
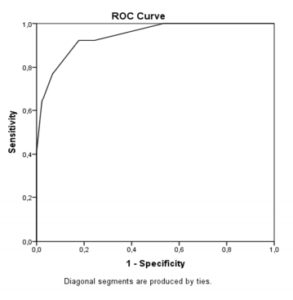
Other analyzes were made by ROC (receiver operating characteristic) curve and the results showed that MoCA total score is effective to differentiate MCI and CG, with a sensitivity of 82.2% and specificity of 92.3% (area under the curve =0,94; cutoff point=25), as well as to distinguish between CG and AD, with 98.1% sensitivity and 100% specificity (area under the curve=0,99; cutoff point=23). These data suggests that for high education level elderly, MoCA has good accuracy in the differential diagnosis of MCI and AD. Figures 1 and 2 presents ROC curves.
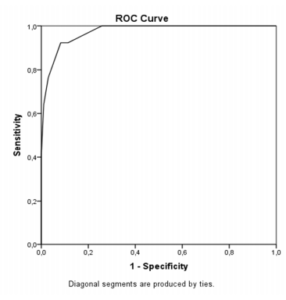
Figure 1. ROC Curve to CG and AD
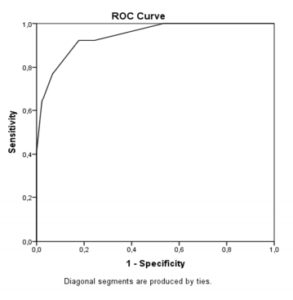
Figure 2. ROC Curve to CG and MCI
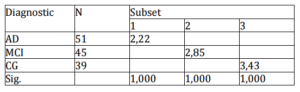
In order to correct type I error in MoCA measures we perform a MANOVA with the three groups as indepenJMED variable and MoCA subtests measures and total score as depenJMED and the results suggested significant differences between the three studied groups overall (Wilks Lambda =4,21; p=0,000). The StuJMED, Newman, Keuls post hoc analysis results are presented in Table 3. These results indicate that MoCA is a good screening test to properly differentiate the groups.
Concerning the tasks, Camel [F(2, 135)=2,93; p=0,056], Lion [F(2, 135)=0,82; p=0,442], LetterA [F(2, 135)=1,05; p=0,354] and Cube [F(2, 135)=1,78; p=0,176] were the only measures that did not yeld significant differences between the three groups. Post hoc analysis (SNK) for all variables were taken and only Trails, Letters and Digit span forward measures differentiate the three groups. The tests that differentiate AD from MCI and CG were Clock drawing, Naming Rhino and Serial 7. These measures did not yeld significant differences between CG and MCI. Finally, Sentence and Digit Span Backward provide significant differences between CG and the other two groups, not differentiating MCI and AD.
Table 3. StuJMED Newman Keuls Post Hoc Analysis Results for Moca Total Score
Discussion
This research aimed to analyze the accuracy of MOCA sub tests by comparing healthy elderly, MCI and AD with more than 4 years of schooling. Regarding the cognitive performance of elderly, many studies point to the importance of neuropsychometrics ratings in the differential diagnosis of dementia describing a common concern which is the search to find a test with higher predictive value for the differential diagnosis of mild cognitive impairment specially in elderly with low educational levels (Gainotti, et . al., 1994; Giovannetti, et. al., 2001; Gold, et. al., 2007; Pedret-Valls, et. al., 2011; Cecato, Fiorese, Montiel, Bartholomeu & Martinelli, 2012).
Considering the MoCA test, the presented data show that the majority of its sub tests can differentiate the three studied groups. The results shows that Trails, clock test, Rhinos appointment, Sentence, abstraction, delayed recall and orientation were important measures to differentiate the groups. In these sub tests can be observed the highest errors rates in the AD group. The MCI group had intermediate scores which means they did not achieve enough points for healthy elderly, but also did not get lower scores that suggests dementia.
The Cube, Leo and Camel / Dromedary Naming and Digit span sub tests were not important in differentiating the groups. Regarding the cube task, the participants showed very similar error rates in all three groups. Also, the naming of animals and Digit span test showed similar hits percentage within the groups.
MoCA was developed as an assessment tools for help diagnosing MCI and mild dementia (Nasreddine, et. Al, 2005). When compared to MMSE (one of the most widely used screening instruments in the world), the MoCA has more memory and executive function items (Nasreddine, et. Alma, 2005), and a more structured language subclause (Cecato et. al., 2010). In this research it became clear that MOCA has accuracy and could be usefull in helping diagnosing and differentiating clinical frames (MCI and AD) and could also help detect MCI because of its power to differentiate this group of CG what could be usefull to prevent progression to AD. Other studies also indicate the effectiveness of the MoCA as an instrument to facilitate the MCI differential diagnosis.
Another study that supports the hypothesis that MoCA is an effective tool for helping diagnosis of cognitive impairment was conducted by Markwick, et. al. (2012). The authors discovered that even cognitive impaired patients can present MMSE normal scores and lower scores in MoCA. The results showed obvious decline in the MoCA subtests, and the conclusion reached by the researchers was that MoCA appears to be a more sensitive screening test than MMSE for early detection of cognitive decline.This data is consistent to results found in this study, in which MoCA has good sensitivity and specificity in differentiating MCI cases of AD and normal elderly.
The educational level also reinforces the hypothesis of better performance in MoCA compared to other instruments, since the sample corresponds to elderly people with more than four years of study and the differences in schooling years between the groups were not statisticaly significant (X2=9,15; p=0,517). New researches could have better control on this variable, because of its relevance on cognitive assessment. Nevertheless, this research points out that MoCA can be a good screening instrument to assess the studied clinical frames in elderly with higher levels of education, helping differential diagnosis of MCI and AD. It is worth to mention that the AD diagnosis is complex and demand other clinical remarks to assert. Its worth to note that dementia diagnoses requires evidence of functional declines and MoCA does not assess that. Hence, it may be usefull in screening cognitive aspects of demential frames and MCI that can help the proper diagnose.
As detailed above, the test MoCA is better structured than MMSE, with more memory items as well as language and executive functions tests (Cecato et al, 2010; Nasreddine, et al, 2005). We can conclude that MoCA is an appropriate instrument for help mild cognitive impairment diagnosis among brazilian elderly, with over four years of study, showing predictive value in differentiating AD from MCI. Further studies are needed with larger numbers of participants to yeld validity evidences to the test also for elderly with low educational level.
References
Albert, M. S., DeKosky, S. T., Dickson, D., Dubois, B., Feldman, H. H., Fox, N. C. et al. (2011). “The Diagnosis of Mild Cognitive Impairment Due to Alzheimer’s Disease: Recommendations from the National Institute on Aging-Alzheimer’s Association Workgroups on Diagnostic Guidelines for Alzheimer’s Disease,” Alzheimer’s & Dementia, 7(3) 270-279.
Publisher – Google Scholar
American Psychiatry Association. (1994). ‘Diagnostic and Statistical Manual of Mental Disorders,’ 4ªed. Washington, DC.
Google Scholar
Brucki, S. M. D., Nitrini, R., Caramelli, P., Bertolucci, P. H. F. & Okamoto, I. (2003). “Sugestões Para O Uso Do Mini-Exame Do Estado Mental No Brasil,” Arquivos de neuro-psiquiatria, 61(3-B) 777-781.
Publisher – Google Scholar
Cecato, J. F., Fiorese, B., Montiel, J. M., Bartholomeu, D. & Martinelli, J. E. (2012). “Clock Drawing Test in Elderly Individuals with Different Education Levels: Correlation with Clinical Dementia Rating,” American Journal of Alzheimer’s Disease and Other Dementias, 27, 620-624.
Publisher – Google Scholar
Cecato, J. F., Martinelli, J. E., Bartholomeu, L. L., Basqueira, A. P., Yassuda, M. S. & Aprahamian, I. (2010). “Verbal Behavior in Alzheimer’s Disease Patients: Analysis in Repetition Phrases,” Dement Neuropsychol, 4(3) 202-206.
Publisher
Folstein, M. F., Folstein, S. E. & Mc Hugh, P. R. (1975). “Mini-Mental State: A Practical Method for Grading the Cognitive State of Patients for the Clinician,” Journal of Psychiatric Research, 12, 189-198.
Publisher – Google Scholar
Freitas, S., Simões, M. R., Alves, L. & Santana, I. (2011). “Montreal Cognitive Assessment: Validation Study for Mild Cognitive Impairment and Alzheimer Disease,” Alzheimer Disease & Associated Disorders, 12, 37-42.
Publisher – Google Scholar
Gainotti, G. & Marra, C. (1994). “Some Aspects of Memory Disorders Clearly Distinguish Dementia of the Alzheimer’s Type from Depressive Pseudo-Dementia,” Journal of Clinical and Experimental Neuropsychology, 16(1) 65-78.
Publisher – Google Scholar
Giovannetti, T., Lamar, M., Cloud, B. S., Swenson, R., Fein, D., Kaplan, E. et al. (2001). “Different Underlying Mechanisms for Deficits in Concept Formation in Dementia,” Archives of Clinical Neuropsychology, 16(6), 547-60.
Publisher – Google Scholar
Gold, C. A., Marchant, N. L., Koutstaal, W., Schacter, D. L. & Budson, A. E. (2007). “Conceptual Fluency at Test Shifts Recognition Response Bias in Alzheimer’s Disease: Implications for Increased False Recognition,” Neuropsychologia,45(12), 2791-2801.
Publisher – Google Scholar
Heinik, J., Solomesh, I. & Berkman, P. (2004). “Correlation between the CAMCOG, the MMSE, and Three Clock Drawing Tests in a Specialized Outpatient Psychogeriatric Service,” Archives of Gerontology and Geriatrics, 38(1), 77-84.
Publisher – Google Scholar
Hughes, C. P., Berg, L., Danziger, W. L., Coben, L. A. & Martin, R. L. (1982). “A New Clinical Scale for the Staging of Dementia,” The British Journal of Psychiatry, 140, 566-572.
Publisher – Google Scholar
Markwick, A., Zamboni, G. & De Jager, C. A. (2012). “Profiles of Cognitive Subtest Impairment in the Montreal Cognitive Assessment (Moca) in a Research Cohort with Normal Mini-Mental State Examination (MMSE) Scores,” Journal of Clinical and Experimental Neuropsychology, 34(7), 750-757.
Publisher – Google Scholar
Mckhann, G. M., Knopman, D. S., Chertkow, H., Hyman, B. T., Jack, C. R. Jr., Kawas, C. H. et al. (2011). “The Diagnosis of Dementia Due to Alzheimer’s Disease: Recommendations from the National Institute on Aging-Alzheimer’s Association Workgroups on Diagnostic Guidelines for Alzheimer’s Disease,” Alzheimer’s & Dementia 7(3), 263—269.
Publisher – Google Scholar
Memória, C. M. (2012). Propriedades Psicométricas Do CANS-MCI: Um Teste Computadorizado Para a Avaliação Do Comprometimento Cognitivo Leve Em Idosos, Dissertação De Mestrado. FMUSP. Universidade De São Paulo. São Paulo. Brazil.
Publisher
Mendez, M. F., Ala, T. & Underwood K. L. (1992). “Development of Scoring Criteria for the Clock Drawing Task in Alzheimer’s Disease,” Journal of the American Geriatrics Society, 40, 1095-1099.
Publisher – Google Scholar
Nasreddine, Z. S., Phillips, N. A., Bédirian, V., Charbonneau, S., Whitehead, V., Collin, I. et al. (2005). “The Montreal Cognitive Assessment, MoCA: A Brief Screening Instruments for Mild Cognitive Impairment,” Journal of the American Geriatrics Society, 53(4), 695-699.
Publisher – Google Scholar
Petersen, R. C., Stevens, J., Ganguli, M., Tangalos, E. G., Cummings, J. & Dekosky, S. T. (2001). “Pratice Parameter: Early Detection of Dementia: Mild Cognitive Impairment,” Neurology, 56, 1133-1142.
Publisher – Google Scholar
Pfeffer, R. I., Kurosaki, T. T., Harrah, C. H. Jr., Chance, J. M. & Filos, S. (1982). “Measurement of Functional Activities in Older Adults in the Community,” Journal of Gerontology. 37, 323-329.
Publisher – Google Scholar
Rahman, T. T. A. & El Gaafary, M. M. (2009). “Montreal Cognitive Assessment Arabic Version: Reliability and Validity Prevalence of Mild Cognitive Impairment among Elderly Attending Geriatric Clubs in Cairo,” Geriatrics & Gerontology International, 9(1), 54-61.
Publisher – Google Scholar
Roth, M., Tym, E., Mountjoy, C. Q., Huppert, F. A., Hendrie, H., Verma, S. et al. (1986). “CAMDEX. A Standardised Instrument for the Diagnosis of Mental Disorder in the Elderly with Special Reference to the Early Detection of Dementia,” The British Journal of Psychiatry, 149, 698-709.
Publisher – Google Scholar
Sarmento, A. L. R. (2009). Apresentação E Aplicabilidade Da Versão Brasileira Da Moca (Montreal Cognitive Assessment) Para Rastreio De Comprometimento Cognitivo Leve [MD]. São Paulo (SP): Escola Paulista De Medicina Da Universidade Federal De São Paulo. Programa De Pós-Graduação.
Publisher – Google Scholar
Shulman, K. I., Gold, D. P., Cohen, C. A. & Zucchero, C. A. (1993). “Clock-Drawing and Dementia in the Community: A Longitudinal Study,” International Journal of Geriatric Psychiatry, 8(6), 487-496.
Publisher – Google Scholar
Siedlecki, K. L., Stem, Y., Reuben, A., Sacco, R. L., Elkind, M. S. V. & Wright C. B. (2009). “Construct Validity of Cognitive Reserve in a Multiethnic Cohort: The Northern Manhattan Study,” Journal of the International Neuropsychological Society, 15(4), 558-569.
Publisher – Google Scholar
Tsai, C. F., Lee, W. J., Wang, S. J., Shia, B. C., Nasreddine, Z. & Fuh, J. L. (2011). “Psychometrics of the Montreal Cognitive Assessment (Moca) and its Subscales: Validation of the Taiwanese Version of the Moca and an Item Response Theory Analysis,” International Psychogeriatrics, 12, 1-8.
Publisher – Google Scholar
Valls-Pedret, C., Olives, J., Bosch, B., Caprile, C., Castellví, M., Molinuevo, J. L. et al. (2011). “Landscape Test for Assessing Visual Memory in Alzheimer’s Disease,” Rev Neurol, 53(1), 1-7.
Publisher – Google Scholar
Yesavage, J. A., Brink, T. L., Rose, T. L., Lum, O., Huang, V., Adey, M. et al. (1983). “Development and Validation of a Geriatric Depression Screening Scale: A Preliminary Report,” Journal of Psychiatric Research, 17(1), 37-49.
Publisher – Google Scholar