Introduction
Breast feeding is a common practice in Bangladesh. Ninety eight percent of children are breast fed at some time. However, the recommended practice of exclusive breast feeding for 6 months is not followed optimally (BDHS, 2009). The trend of EBF, as evidenced through Bangladesh demographic and health survey (BDHS), shows more or less static figure through 1993 to 2007 and it was 46%, 42% and 43%, respectively (BDHS, 1995, BDHS, 2005, BDHS., 2009) and there has been marked improvement to 64% in 2011 (BDHS, 2011).
The global picture of breast feeding practice shows that exclusive breastfeeding rates are low, at about 25% in Africa, 45% in Asia and 31% in Latin America and the Caribbean (Lauer J A, 2004). The prevalence of continued breastfeeding is about 86% for infants 6—11 months of age in the developing world and for children 12—23 months of age, it is about 37% in Latin America, in the Caribbean 70% and 72% in Africa and Asia (Lauer J A, 2004).
The prevalence and duration of breastfeeding are recognized as important health indicators (WHO, 2001). Bangladesh is one of the few countries where most of the mothers follow the Innocenti Declarations ideal of breastfeeding for “two years and beyond”. Giasuddin, et al. reported median duration of full breast-feeding is 3.67 months, and mean and median durations of total breast-feeding are 31.3 and 30 months, respectively (Giasuddin, 2004). National survey shows the mean duration of EBF was 3.3 month, and the median duration of total breast feeding 32.8 months (BDHS, 2009).In comparison to other South Asian countries like India, Pakistan and Sri Lanka where average durations of breast-feeding were 18.4, 21.8 and 23.2 months respectively, breast-feeding duration is relatively higher in Bangladesh (Rajaretnam T, 1994, Page HJ, 1992, Mahler K, 1996).
The growth and development of a child critically depends on improved feeding practices (León-Cava N, 2002). Different studies from developing countries show that the risk of nutritional deficiency and growth retardation in children is maximum between 3 and 15 months of age, because this age period is vulnerable for suboptimal breastfeeding and inadequate complementary feeding practices (Shrimpton, 2001). In Bangladesh some liquid or solid food are often given to infants too early, and study shows 6% are given solid or semisolid food under 6 months age (BDHS, 2009). On the other hand, the delay in starting complementary food is also common and only 21% of children between 6-23 month receive an appropriate diet (BDHS, 2011).
In most of the maternity care hospitals, a lactation management centre exists to help mothers with breast feeding problems and to promote, protect and support breast feeding. There are limited data on nutritional status of lactating mothers in Bangladesh and whether maternal nutrition has any effect on breast feeding practices is not much explored. The purpose of this study was to assess the nutritional status of lactating mothers, to find out their breast feeding practices and reasons for attending the lactation management centre. This will help to address the behavioral issues for the promotion of breast feeding practices in the context of Bangladesh.
Method
This was a cross sectional study conducted at the Institute of Child Mother Health during March-April 2012. The mothers attending lactation management centre were selected consecutively. Data were collected using structured questionnaire and analyzed in SPSS program.
Results
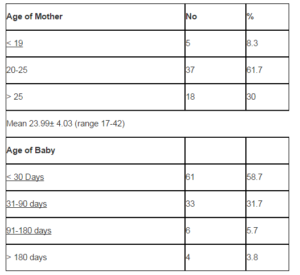
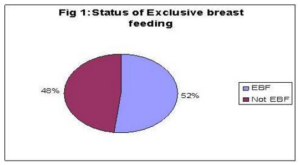
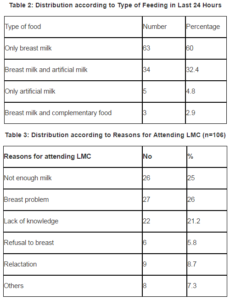
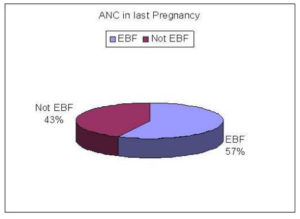
Among a total 106 mothers, 8.6% were adolescents, 61.9% belong to 20-25 yrs, and mean age was 23.9±4yrs. Most of the infants were below 6 months of age and 58.7% were <30 days old (Table-1). Exclusively, breast feeding was reported by 52% (Figure-1) Regarding the type of feeding in last 24 hours, 60% received only breast milk, 32.4% had BF and Artificial milk, and only 2.9% received CF Ä• Breast feeding (Table-2). The main reason for attending LMC was not enough milk (25%), breast problem (26%) and 21.2% stated lack of knowledge (Table-3) About 70.9% had average body build, and only 4.9% have a BMI < 18.5 (Table-4). There was no relation between the BMI of the mother and the EBF (Table 5) Among those who were delivered by CS, 60.3% were exclusively breastfed (Table-6). Exclusively, breastfeeding was more among mothers who took ANC in last pregnancy (Figure 2).
Table1: Distribution according to Age of Mother and Child (n= 106)
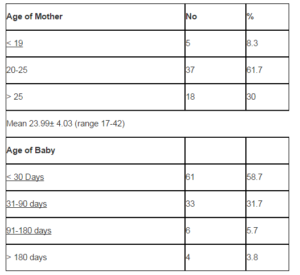
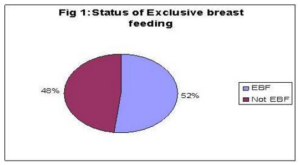
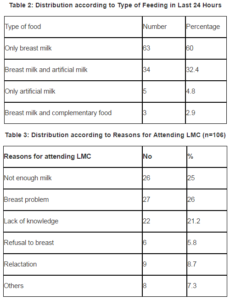

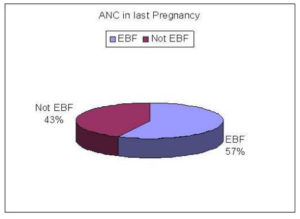
Figure 2: Relation between ANC in Last Pregnancy and EBF (n=106)
Discussion
The assessment of exclusive breast feeding status based on a 24-hour recall may not always represent a true picture, especially when there is chance of over reporting, as Lauer found that infants consuming water or water-based drinks along with breast milk are also classified as exclusive breast feeding (Lauer J A, 2004, Armitage, 2002). Routine feeding practices of infants may also change when ill or if the mother is not available at the time of feeding. Some community-based studies have found that infants classified as exclusively breastfeeding with 24-hour recall receive other liquids and even solid foods on a less-than-daily basis (Armitage, 2002, Haidar, 2000). In this study, 90% were within 3 months of age but only 60% were exclusively breastfed, and this is consistent with national data (BDHS, 2011). In comparing the records of 24-hour recall and those from mothers’ daily records, it was found that 24-hour recall overestimated exclusive breastfeeding rates by about 40% at both two and four months of age (Haidar, 2000).
Malnutrition is a common problem in Bangladesh. Survey shows 59% of women (15-49 year) have normal BMI, 30% had <18.5, and 12% have BMI 25 or above (BDHS, 2009). A previous study showed 34% of women had BMI< 18.5 (BDHS, 2004)The quantitative relationship between maternal nutritional status and dietary intake with the volume and composition of the mother’s milk has been studied. Jelliffe, 1978 found the composition of the mother’s milk of marginally nourished mothers is generally maintained within or near the range reported for well nourished women, but protein and fat concentration are influenced by maternal nutritional status and dietary intake (Boerma, 1993).
Prentice et al. found a positive relationship between maternal in triceps skin fold thickness measurement and fat concentration in Gambian women (Prentice, 1981). Hanafi et al. found a significant reduction in the concentrations and amounts of energy and protein in the milk of malnourished mothers (Hanafi, 1972). Brown et al reported that the increase in triceps skin fold thickness of mothers was associated with increases in fat and energy concentration of breast milk, and increases in body weight were associated with the increase in the amount of milk and all its major nutrients (Brown, 1986). In the current study, the majority of mothers were well nourished however, a quarter of them complained of insufficient milk production.
One common problem for breast feeding perceived by lactating mother is low milk production. Study found 54% lactating mothers mentioned that their babies do not get sufficient breast milk, and their complaint was more prevalent among urban than rural mothers (Akhtar, 1998). For sustenance of exclusive breast feeding in the first 3 months it is most crucial and is vulnerable to distortions due to the perception of not enough milk. A study shows that the common perception of not enough milk is the most important factor that hampers exclusive breast feeding and trigger the introduction of artificial milk (Haidar, 2010).
Breast problems were the cause for attending lactation management centre in about one fourth of the mothers. Care seeking practices of mothers attending the lactation management centre of ICMH was compared between 2000 and 2006. It was found that breast problems were mentioned by 32.5% vs. 40% and not enough milk was complained of in 20% vs. 27.5% of mothers attending the centre during 2000 and 2006 respectively (Tasnim, 2007). In a study at Rajshahi medical college, it was found that 12% of the mothers had different types of breast problems. The most important problem was breast engorgement, next was sore nipples, flat nipple, cracked nipple and breast abscess (Hossain, 2005). The examination of breast for the identification of any problem like retracted nipple may help to prepare mothers for exclusive breast feeding. At the same time, routine examination of breast during postnatal period is mandatory to boost up maternal confidence and detect any breast problem like crack nipple, sore nipple early, and prevent complications.
Strategies for the promotion of breastfeeding include a combination of factors like hospital norms and services, legislation and institutional policies, health worker training, mass media campaigns, peer counseling and education, and mother-to-mother support groups (Green, 1999, Hill, 2004). Support for breast feeding during immediate postpartum period is crucial to boost up the mother’s confidence and sustaining breast feeding. However, high rates of initiation of exclusive breast feeding and low sustenance often co-exist. Rooming in and bedding in during hospital stay has a positive effect in sustaining exclusive breast feeding. It is often said mothers after caesarean section face more difficulty in early initiation and exclusive breast feeding because of pain and other problems. However, they can successfully initiate breast feeding soon after operation and can room in with their infants if proper support is given. The current study found that EBF was more among mothers who underwent caesarean section. This might be the effect of hospital policy in accordance with baby friendly hospital.
Access to information and motivation on BF during prenatal period is an important predictor of postnatal successful lactation performance. Community based behavior change programs focusing on hospital norms and services, legislation and institutional policies, health worker training, mass media campaigns, peer counseling and education, mother to mother support and a combination of these strategies has shown marked increases in exclusive breastfeeding of infants 0 to 6 months in different countries of Africa (Quinn, 2005). Although antenatal care was received by most of the mothers in this study exclusive breast feeding was not optimum indicating some gaps in the counseling, and there should be more emphasis on this issue.
Conclusion
Lactation problems are more likely in the first month of the baby and the feeling of insufficient milk in the breast is a major threat to sustenance of exclusive breast feeding.
About one fifth of mothers perceived to have lack of knowledge which indicates people’s concern for breast feeding. Maternal nutritional status does not relate with breast feeding practices. Exclusive breast feeding was more among those delivered by caesarean section, probably due to greater contact with health care providers and their active support.
References
Akhter, H. H., Akhter, M. & Azad, K. M. (1998). “A National Baseline Survey to Assess the Breastfeeding Practices in Bangladesh,” BIRPERHT.
Publisher – Google Scholar
Armitage, P., Berry, G. & Matthews, J. N. S. (2002). “Modelling Categorical Data,” In Statistical Methods in Medical Research, 4th edition, Oxford, England: Blackwell; 485-502.
Publisher – Google Scholar
Bangladesh Demographic and Health survey 1993-94. (1995). ‘Extended Analysis. National Institute of Population Research and Training,’ Mitra and associates.
Bangladesh Demographic and Health survey (2011). “National Institute of Population Research and Training,” Mitra and associates.
Publisher
BDHS (2001). “Bangladesh Demographic and Health Survey 1999-2000,” National Institute of Population Research and Training, Mitra and associates.
Publisher – Google Scholar
BDHS (2005). ‘Bangladesh Demographic and Health Survey 2004,’ National Institute of Population Research and Training, Mitra and associates.
Google Scholar
BDHS. (2009). ‘Bangladesh Demographic and Health Survey 2007,’ National Institute of Population Research and Training (NIPORT). Mitra & associates.
Google Scholar
Boerma, J. T. & Sommerfelt, A. E. (1993). ‘An Assessment of the Quality of Breast-Feeding Data in DHS-I Surveys,’Calverton, Maryland, USA: Macro International.
Brown, K. H., Akhtar, N. A., Robertson, A. D. & Ahmed, M. G. (1986). “Lactational Capacity of Marginally Nourished Mothers: Relationships between Maternal Nutritional Status and Quantity and Proximate Composition of Milk,” Pediatrics, 78: 909
Publisher – Google Scholar
Giashuddin, M. S. & Kabir, M. (2004). “Duration of Breast-Feeding in Bangladesh,” Indian Journal of Medical Research; 119: 267-272
Publisher – Google Scholar
Green, C. P. (1999). “Improving Breastfeeding Behaviors: Evidence from Two Decades of Intervention Research,”Published for USAID by the LINKAGES Project, Washington, DC;
Publisher – Google Scholar
Haider, R., Ashworth, A., Kabir, I. & Huttly, S. R. A. (2000). “Effect of Community-Based Peer Counselors on Exclusive Breastfeeding Practices in Dhaka, Bangladesh: A Randomized Controlled Trial,” Lancet, 356:1643-1647. PubMed Abstract | Publisher Full Text
Publisher – Google Scholar
Haider, R., Rasheed, S., Sangvi, T. G., Hassan, N., Pachon, H., Islam, S. & Jalal, C. S. B. (2010). “Breastfeeding in Infancy: Identifying the Program-Relevant Issues in Bangladesh,” International Breastfeeding Journal; 5:21-32
Publisher – Google Scholar
Hanafy, M. M., Morsey, M. R. A., Seddick, Y., Habib, Y. A. & El Lozy, M. (1972). “Maternal Nutrition and Lactation Performance,” Journal of Tropical Pediatrics; 18:187-191
Publisher – Google Scholar
Hill, Z., Kirkwood, B. & Edmond, K. (2004). “Family and Community Practices that Promote Child Survival, Growth and Development: A Review of the Evidence,” Geneva, Switzerland: World Health Organization;
Publisher – Google Scholar
Hossain, M. A., Haque, M. I., Siddiqui, A. B. & Bari, M. I. (2005). “Activities of Lactation Management Centre of Rajshahi,”Journal of Teachers Association, December; 18 (2)
Publisher – Google Scholar
Jelliffe, D. B. & Jelliffe, E. F. P. (1978). Human Milk in the Modern World, Oxford, Oxford University Press,
Publisher – Google Scholar
Lauer, J. A., Betrán, A. P., Victora, C. G., de Onís, M. & Barros, A. J. D. (2004). “Breastfeeding Patterns and Exposure to Suboptimal Breastfeeding among Children in Developing Countries: Review and Analysis of Nationally Representative Surveys,” BMC Medicine 2:26 doi:10.1186/1741-7015-2-26
Publisher – Google Scholar
León-Cava, N., Lutter, C., Ross, J. & Martin, L. (2002). Quantifying the Benefits of Breastfeeding: A Summary of the Evidence, Published by PAHO and by the LINKAGES Project for USAID, Washington, DC;
Publisher – Google Scholar
Mahler, K. (1996). “Women Breast-Feeding Infants Longer in Many Developing Countries,” International Family Planning Perspectives 22: 134-5.
Publisher – Google Scholar
Page, H. J., Lesthaeghe, R. J. & Shah, I. H. (1982). “Illustrative Analysis: Breastfeeding in Pakistan,” WFS Scientific Reports No. 37. Voorburg, Netherlands: International Statistical Institute; 115.
Publisher – Google Scholar
Prentice, A., Prentice, A. M. & Whitehead, R. G. (1981). “Breast-Milk Fat Concentrations of Rural African Women: 2 Long Time Variations within a Community,” British Journal of Nutrition; 45: 495-503
Publisher – Google Scholar
Quinn, V. J., Guyon, A. B., Schubert, J. W., Stone-Jiménez, M., Hainsworth, M. D. & Martin, L. H. (2005). “Improving Breastfeeding Practices on a Broad Scale at the Community Level: Success Stories From Africa and Latin America,”Journal of Human Lactation 21(3).
Publisher – Google Scholar
Rajaretnam, T. (1994). ‘Trend and Differentials in Breast-Feeding and Amenorrhea Durations in a Rural Area in south India,’ Demography India 23: 83-95.
Shrimpton, R., Victora, C. G., de Onis, M., Costa Lima, R., Blössner, M. & Clugston, G. (2001). “Worldwide Timing of Growth Faltering: Implications for Nutritional Interventions,” Pediatrics. 2001; 107:E75.
Publisher – Google Scholar
Tasnim, S. & Banu, L. P. (2007). ‘Care Seeking for Breast Feeding in a Periurban Hospital,’ Bangladesh Medical Journal; 36 (1): 4-6
WHO (2001). ‘Resolution WHA54.2: Infant and Young Child Nutrition (WHA54.2) Geneva,’ Switzerland: World Health Organization.
Google Scholar