Introduction
Acute lower respiratory tract infection (ALRI) is the major cause of morbidity and mortality in paediatric age group and responsible for 120 million episodes of pneumonia and 1.3 million under-five childhood global deaths (Walker et al., 2013). In Bangladesh, Acute Respiratory Tract Infections (ARI) alone is responsive 38.8% of total Paediatric hospital admission, 40% to 60% of total Paediatric OPD visit (Akbar et al., 1992, WHO, 1984) and among the 182936 under-five childhood deaths in Bangladesh, 14% were due to pneumonia (Black et al., 2010). The two most common causes of ALRI in children below 2 years of age are bronchiolitis and community acquired pneumonia (CAP) (Haque et al., 2012, Kabir et al., 2009a, Kabir et al., 2009b). Pneumonia can be diagnosed clinically in a febrile and coughing child based on fast breathing and chest in-drawing the two important features for the diagnosis of pneumonia in children (Chisti et al., 2009, Chisti et al., 2011). Additionally, crackles, occasional rhonchi and end point consolidation and other infiltrates on X-ray chest might help for the diagnosis of pneumonia in children (Cherian et al., 2005). The important clinical features to distinguish pneumonia from bronchiolitis are age, nutritional status, fever, runny nose, and an auscultatory finding in lungs such as wheeze and crackles (Kabir et al., 2003a).
The first report of bronchiolitis in an epidemic form in Bangladesh was in the year 2001-2002 (Kabir et al., 2003b, Kabir, 2002) most of which was due to respiratory syncytial virus (RSV) during winter and early spring (Haque et al., 2012). The peak age of bronchiolitis is between 2 and 6 months with the incidence of as high as 83% of all cases of ALRI (Kabir et al., 2009a, Grover et al., 2011). Though there has been awareness about bronchiolitis in Bangladesh, still the diagnosis of pneumonia gets upper hand to level any child presenting with fast breathing and chest in-drawing (Kabir and Mridha, 2003). There are lot of recent advances in the management of bronchiolitis (Verma et al., 2013), but still these children are indiscriminately treated with costly antibiotics like ceftriaxone (Kabir et al., 2003b). Although, bronchiolitis used to be associated with coryzal symptoms followed by rapid onset of wheezing, fever, tachypnea, chest in-drawing, crepitations and rhonchi with radiographic evidence of hyperinflation (Ahamed and Kabir, 2003). In the guideline for the management of bronchiolitis by the Bangladesh Pediatric Pulmonology Forum (BPPF) , cough and respiratory distress preceded by runny nose in young children below 2 years with or without wheeze or fever have been proposed to be considered as bronchiolitis (Kabir et al., 2004). Thus, it is important to consider the diagnosis of bronchiolitis in these children to optimize its management and counsel the parents .
Prevalence of childhood asthma is substantial and asthma has often been treated as pneumonia and under-diagnosed in developing countries (Nantanda et al., 2013). Bangladesh is no longer any exception of them with low prevalence (Kabir et al., 2005).
From IMCI point of view, it is a common practice for our health care professionals to diagnose any child coming with fast breathing, or chest in-drawing, or cyanosis, or hypoxemia to level as to have ‘pneumonia’ or ‘severe pneumonia’ (WHO, 2013), irrespective of the presence or absence of bronchiolitis, asthma or other illness causing respiratory distress. As a result, the children are given broad spectrum antibiotics without looking into the actual etiology of the respiratory distress, although, it will be of extreme significance to identify the large group of children who need different modality of management resulting in optimised management and rational use of antibiotics. However, data are very limited on the magnitude of different acute respiratory disorders, their diagnosis and management in under-5 children by the untrained local doctors attending different hospitals. Thus, we sought to have the knowledge of the magnitude, diagnosis, and management of different types of ARI focusing on pneumonia, bronchiolitis, and asthma in our country.
Methodology
Study Design
It was a cross sectional study conducted between February 2008 and January 2009. The study was approved by the institutional review board named as “Ethical Review Committee” of Bangladesh Medical Research Council (BMRC). A written informed consent was obtained from the care givers or the legal guardians before enrolment in the study. It is prudent to mention that, all the participants in the study provided their written informed consent to participate in the study and the “Ethical Review Committee” approved this consent procedure.
Study Population
Two groups of children were included in the study group. One group aged 1 month to 59 months and were found hospitalised on a particular day into ward of the hospital. Another group aged 1 month to 59 months who attended the outpatient department (OPD) on that very day with different health problems. Case definitions of diagnostic criteria of different respiratory disorders have been shown in table 1.
Table 1: Clinical case definitions of different respiratory disorders
AOM: acute otitis media; CSOM: chronic suppurative otitis media; TB: tuberculosis; CXR: chest X-ray; TST: tuberculin skin test; H/O: history of;
Children having respiratory distress with signs of heart failure (tachycardia with hepatomegaly or dependent edema or heat murmur), children having respiratory distress arising from non-respiratory cause were excluded from the study.
The study was conducted in all government medical college hospitals, randomly selected twelve district hospitals and twelve upazilla hospitals from all over Bangladesh. The largest children’s hospital of the country, 350-beded Dhaka Shishu Hospital (DSH), Dhaka and Institute of Child and Mother Health (ICMH), Dhaka having the largest OPD service were also included in the study. Other important hospitals of Dhaka city included in the study were Bangabandhu Sheikh Mujib Medical University (BSMMU) and Institute of Child Health (ICH), Mirpur. The total hospitals were 43 from all over Bangladesh (15 medical colleges and 12 district hospitals, 12 upazilla hospitals, ICMH, DSH, ICH and BSMMU).
Procedure
The project manager and the four physicians were trained on the project, its goals, objectives, procedures and utility of the study for three days (including orientation and practical sessions) at ICMH. The orientation also included the clinical diagnostic criteria of respiratory disorders and hands on training on filling up of the structured questionnaires. Trainee doctors in pediatrics were trained (research team doctors) on the clinical diagnosis of various respiratory disorders and their performance were field tested before starting the data collection. The research team doctors collected data on a single day from OPD and IPD. The co-investigators were also invited to attend on the first orientation day.
The four member team of the doctors after undergoing orientation course and about how to fill up the questionnaire, started travelling to different hospitals. First the hospitals of ICMH, DSH and Dhaka Medical College Hospital (DMCH) were covered. The team first met the Head of Department (HOD) of Pediatrics on the day of data collection. The HOD of respective hospital was informed beforehand, so that, HOD could organise his staff of OPD and IPD in preparation of the ensuing visit by the research team doctors. The OPD doctors of the respective hospital referred the respiratory cases to the research team doctors after managing the cases. The research team doctors had taken face-to-face interview with care givers and filled-up the questionnaires, evaluated the diagnosis made by the local doctors of the respective hospital and made the actual diagnosis both in the OPD and IPD. In case of inpatient documentation, the management given by the local hospital doctors was also documented in the questionnaires. The documentation included total number of under five children attended the OPD, total under five children hospitalized in inpatient, and total number of respiratory cases both in OPD and IPD.
The research team doctors remained vigilant on every case identification and meticulously filled-up the printed questionnaire after having an interview with the care givers and thorough physical examination of the child, and maintained all records under the supervision of the co-investigators and co-investigators performed the data checking under the supervision of the principal investigator (PI). PI was solely responsible for supervising the data entry, analysis, data interpretation and writing the drafts. He maintained constant connection through the project manager with every centre and constantly guided the proceedings.
All data were rechecked and scrutinised by the PI and maintained with him. The data were cleaned and entered by an enterer into the Epi-info program and analysed in the Statistical Package for the Social Sciences (SPSS) software programme. The magnitude of the problems was assessed by measuring the proportions and the validity of the diagnoses of different types of ALRI by local doctors by comparing with trained research team doctors was performed by evaluating the sensitivity and specificity.
Results
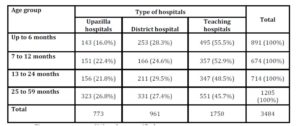
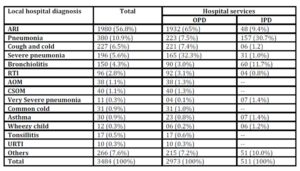
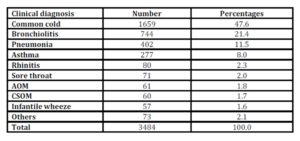
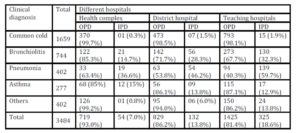
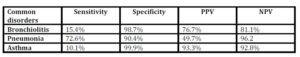
The total number of reviewed children under the age of 15 attending different hospitals was 7793 and among them the under-five children were 5157 (66%). Among a total of 5157 (OPD 4115,80% and IPD 1042, 20%) surveyed children, 3484 (67.5%) had respiratory problems. Among the respiratory problems, OPD cases were 2973 (85%) and IPD cases 511 (15%). Among the 43 hospitals surveyed; 19 teaching hospitals, 12 district hospitals, and 12 upazilla hospitals entertained 1750 (50%), 961 (28%), and 773 (22%) children respectively. Utilization of hospital beds in upazilla hospital, district hospital, and medical college hospital/ teaching hospitals was 54 (7%), 132 (14%), and 325 (19%) respectively. Children with respiratory disorders, 2113 (61%) were male and 1371 (39%) were female. Their mean age was 21.3 months. However, their different distribution has been shown in table 2. Different respiratory disorders diagnosed clinically by local doctors and by trained research team doctors have been shown in table 3 and table 4 respectively. Distribution of respiratory disorders in OPD and IPD of different categories of hospitals has been shown in table 5. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of diagnosis of bronchiolitis, pneumonia, and asthma by the local doctors were variable and have been shown in table 6.
Table 2: Distribution of ages of children attending different levels of hospitals
Table 3: Total, OPD and IPD distribution of clinical diagnoses of respiratory disorders by the local hospital doctors
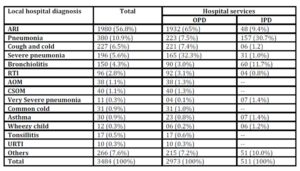
Table 4: Number and percentages of clinical diagnoses of respiratory disorders by the research team 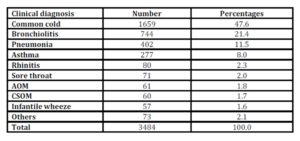
Table 5: Distribution of respiratory disorders in OPD and IPD of different categories of hospitals
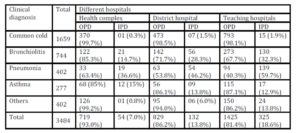
Table 6: Overall diagnostic accuracy of local hospital doctors to identify bronchiolitis, pneumonia and asthma
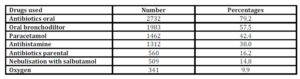
Table 7: Number and percentages of variety of medications used for study patients
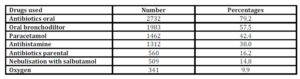
Medications used for these study children have been shown in table 7. Oral antibiotics (79%), oral bronchodilators (57.5%), paracetamol (42%), antihistamine (38%), parental antibiotics (16%), nebulized salbutamol (15%) and oxygen (10%) were important modalities. In common cold, 654/1659 (39%) cases were treated with cotrimoxazole, followed by amoxicillin (256, 15%), azithromycin (186, 11%), cefradine (108, 6.5%), ceftriaxone (106, 6%) and erythromycin (69, 4%). Cotrimoxazole was mostly (236/325, 69%) used in upazilla hospitals In bronchiolitis, most (267/744,36%) children received ceftriaxone followed by cotrimoxazole (122, 16%), amoxicillin (112, 15%), azithromycin (40, 5%) and cefradine (35, 5%). Cotrimoxazole was the most common antibiotic (51, 42%) used in upazilla hospitals . Ceftriaxone was mostly used in teaching hospitals (156/267, 58 %) followed by district hospital (84, 31%). Asthma was treated mostly with cotrimoxazole (69/277, 25%), followed by azithromycin (65, 23%), ceftriaxone (53, 19%), and amoxicillin (41, 15%). Cotrimoxazole was the most common antibiotic in upazilla hospitals (35, 51%). Pneumonia was treated mostly with ceftriaxone (191, 47.5%), followed by amoxicillin (40, 10%), cefixime (34, 8%), cotrimoxazole (34, 8%) and ampicillin (26, 6%). Ceftriaxone was uniformly prescribed in all levels of hospitals; upazilla 46%, district 49% and teaching hospitals 48%.
Discussion
This is the only study which conducted in a nationwide survey to evaluate the magnitude and pattern of respiratory disorders in under-five children and covered 43 health centres from all over the country. Our observation of 5157 children in twelve upazilla hospitals (Upazilla health complex), 12 district hospitals (Sadar/ general hospital), all 15 government medical colleges’ hospitals, and 3 large children’s hospitals of Dhaka city underscored the representative sample of the whole country. There were four main observations in this pioneer study: first- more than two-third of children were suffering from various types of respiratory disorders, second- the common respiratory problems in under-five children attending different hospitals of Bangladesh were common cold followed by bronchiolitis, pneumonia and asthma, third- doctors working in the community level often under-diagnose bronchiolitis and asthma, and fourth- use of irrational antibiotics and other medications in common cold, bronchiolitis, asthma and pneumonia.
The observation of respiratory disorders in more than two-thirds of the evaluated children in our survey is an important finding for the clinicians as well as policy makers in developing countries and this observation is consistent with the earlier studies in other developing countries (El-Sahly et al., 2000, National Institute for and Clinical, 2008).
Important clinical features that have been observed for the diagnosis of common cold, bronchiolitis, pneumonia, and asthma by the trained research team doctors were more or less consistent with our study definition. The findings indicate that policymakers in developing countries may help clinicians to find out a way to improve the skill of identifying and treating different respiratory problems. The observation of common cold and bronchiolitis as the common respiratory problems ahead of pneumonia and asthma in under-five children attending different hospitals of Bangladesh is also important for the clinicians and this is also consistent with earlier studies (El-Sahly et al., 2000, National Institute for and Clinical, 2008). This observation may help our future clinicians to be more rational about the use of antibiotics in such children. However, use of irrational antibiotics and other medications such as antihistamines and oral bronchodilators in common cold, bronchiolitis, asthma and pneumonia in our study is an alarming observation as in other developing countries (Tabatabaei et al., 2012). Observation of irrational prescribing practise by physicians may have an impact on the potential increase in resistance of many respiratory pathogens to currently available antibiotics required for treatment of such children (Gwimile et al., 2012). Moreover, another observation of poor sensitivity in diagnosing bronchiolitis and asthma by the local doctors indicates that doctors working in the community level often miss the diagnosis of bronchiolitis and asthma and may mistakenly diagnose them as childhood pneumonia. This performance of the local hospital doctors indicate that doctors are being trained like field level health workers who are supposed to classify the respiratory disorders at the first level of health care facility before giving any treatment or planning for referral. This performance of the local doctors underscores the importance of urgent need for the continued supervised training on these common respiratory problems for the local doctors by the pediatric respiratory physicians for the appropriate diagnosis and treatment in such children in order to reduce the long term morbidity and deaths especially in resource poor settings.
There were other few important observations. The OPD attendance of under-five children was 80% and IPD cases 20% in this age group indicating greater number of younger children attending the OPD. The attendance of children having respiratory disorders in different hospitals increases from small to larger hospitals (upazilla hospitals 22%, district hospitals 28% and teaching hospitals 50% respectively). Children with respiratory disorders were more treated in OPD (85%) than being hospitalised (15%) which is consistent with earlier studies (Tabatabaei et al., 2012, Stone et al., 2000). Utilisation of hospitals beds also strikingly increased from small to large hospitals (upazilla hospitals 7%, district hospitals 14% and teaching hospitals 19% respectively). This might be due to the fact that large hospitals used to have the availability of higher level of facilities for the better treatment. Our observation of male predominance in attending the all levels of hospitals might be due to the fact that male are more prioritized and simultaneously female less prioritized by their family members in our so called social culture (Chisti et al., 2008). However, the vulnerability of male sex to illness than the female sex cannot be ruled out.
The main limitation of the study is that the study is cross-sectional, it can’t offer a proper answer on the first conclusion made about the incidence of different diagnosis in a hospital setting because of the seasonality of respiratory disorders. Seasonal occurrence of different acute and exacerbations of chronic respiratory disorders is the major driver of their health resource utilization so using a cross-sectional approach clearly underestimates some and overestimates other respiratory disorders.
In conclusion, the results of our data suggest that the magnitude of respiratory disorders in under-five children was very high and more than two-third of them suffered from common respiratory disorders such as common cold, bronchiolitis, pneumonia and asthma. Local doctors often under diagnosed bronchiolitis and asthma might be due to their over diagnosis of pneumonia. Indiscriminate use of antibiotics, antihistamine and bronchodilators are rampant for these common respiratory disorders. The findings underscore the importance of incorporation of the management of bronchiolitis and asthma in the on-going IMCI program considering the magnitude, diagnostic difficulties and mismanagement. Simultaneously, implementation of routine training on diagnostic criteria and treatment of common respiratory disorders especially in large hospitals may help to reduce the long term morbidity and deaths in such children.
Acknowledgements
We would like to express our sincere thanks to all physicians including trained researchers, local doctors, members of the nursing team and cleaners of different hospitals for invaluable support and contribution during patient enrolment and data collection. We would also like to express our gratitude to care-givers/mothers of the study participants for their consent to enrol their children in the study.
Reference
1. AHAMED, F. & KABIR, A. R. M. L. (2003) Radiological evaluation of 162 cases of bronchiolitis. . Bangladesh J Child Helath 27, 6-9.
2. AKBAR, M. S., EHSAN, A. & ALI, C. M. H. (1992) Clinical profile & management of acute Resp tract infection at Dhaka Shishu Hospital, Bangladesh J Child Health, 16, 5-8.
3. BLACK, R. E., COUSENS, S., JOHNSON, H. L., LAWN, J. E., RUDAN, I., BASSANI, D. G., JHA, P., CAMPBELL, H., WALKER, C. F., CIBULSKIS, R., EISELE, T., LIU, L. & MATHERS, C. (2010) Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet, 375, 1969-87.
Publisher – GoogleScholar
4. CHERIAN, T., MULHOLLAND, E. K., CARLIN, J. B., OSTENSEN, H., AMIN, R., DE CAMPO, M., GREENBERG, D., LAGOS, R., LUCERO, M., MADHI, S. A., O’BRIEN, K. L., OBARO, S. & STEINHOFF, M. C. (2005) Standardized interpretation of paediatric chest radiographs for the diagnosis of pneumonia in epidemiological studies. Bull World Health Organ, 83, 353-9.
GoogleScholar
5. CHISTI, M. J., DUKE, T., ROBERTSON, C. F., AHMED, T., FARUQUE, A. S., BARDHAN, P. K., LA VINCENTE, S. & SALAM, M. A. (2011) Co-morbidity: exploring the clinical overlap between pneumonia and diarrhoea in a hospital in Dhaka, Bangladesh. Ann Trop Paediatr, 31, 311-9.
Publisher – GoogleScholar
6. CHISTI, M. J., HUQ, S., DAS, S. K., MALEK, M. A., AHMED, T., FARUQUE, A. S. & SALAM, M. A. (2008) Predictors of severe illness in children under age five with concomitant infection with pneumonia and diarrhea at a large hospital in Dhaka, Bangladesh. Southeast Asian J Trop Med Public Health, 39, 719-27.
GoogleScholar
7. CHISTI, M. J., TEBRUEGGE, M., LA VINCENTE, S., GRAHAM, S. M. & DUKE, T. (2009) Pneumonia in severely malnourished children in developing countries – mortality risk, aetiology and validity of WHO clinical signs: a systematic review. Trop Med Int Health, 14, 1173-89.
Publisher – GoogleScholar
8. EL-SAHLY, H. M., ATMAR, R. L., GLEZEN, W. P. & GREENBERG, S. B. (2000) Spectrum of clinical illness in hospitalized patients with “common cold” virus infections. Clin Infect Dis, 31, 96-100.
Publisher – GoogleScholar
9. GROVER, S., MATHEW, J., BANSAL, A. & SINGHI, S. C. (2011) Approach to a child with lower airway obstruction and bronchiolitis. Indian J Pediatr, 78, 1396-400.
Publisher – GoogleScholar
10. GWIMILE, J. J., SHEKALAGHE, S. A., KAPANDA, G. N. & KISANGA, E. R. (2012) Antibiotic prescribing practice in management of cough and/or diarrhoea in Moshi Municipality, Northern Tanzania: cross-sectional descriptive study. Pan Afr Med J, 12, 103.
GoogleScholar
11. HAQUE, F., HUSAIN, M. M., AMEEN, K. M., RAHIMA, R., HOSSAIN, M. J., ALAMGIR, A. S., RAHMAN, M., RAHMAN, M. & LUBY, S. P. (2012) Bronchiolitis outbreak caused by respiratory syncytial virus in southwest Bangladesh, 2010. Int J Infect Dis, 16, e866-71.
Publisher – GoogleScholar
12. KABIR, A. L., RAHMAN, A. F. & RAHMAN, A. (2009a) ARI situation in our country: aren’t we oblivious of bronchiolitis in Bangladesh? Mymensingh Med J, 18, S50-55.
GoogleScholar
13. KABIR, A. R., MOLLAH, A. H., ANWAR, K. S., RAHMAN, A. K., AMIN, R. & RAHMAN, M. E. (2009b) Management of bronchiolitis without antibiotics: a multicentre randomized control trial in Bangladesh. Acta Paediatr, 98, 1593-9.
Publisher – GoogleScholar
14. KABIR, A. R. M. L. (2002) Bronchiolitis : was there an epidemic? Bangladesh J Child Health 26, 1-2.
15. KABIR, A. R. M. L., AMIN, M. R. & MOLLAH, A. H. (2004) Proposed guidelines for the management of bronchiolitis Bangladesh J Child health 28, 95-99. .
16. KABIR, A. R. M. L., HAQUE, N. & RAHMAN, Q. (2003a) Report on aetiology of lower respiratory tract infection in children, ICMH
17. KABIR, A. R. M. L. & MRIDHA, A. A. (2003) The perception and practice of 245 Health Care Providers (HCPs) working at district and upazilla level on the management of ARI cases, Research report, ICMH.
18. KABIR, M. L., HAQ, N., HOQUE, M., AHMED, F., AMIN, R., HOSSAIN, A., KHATOON, S., AKHTER, S., SHILPI, T., HAQ, R., ANISUZZAMAN, S., KHAN, M. H., AHAMED, S. & KHASHRU, A. (2003b) Evaluation of hospitalized infants and young children with bronchiolitis – a multi centre study. Mymensingh Med J, 12, 128-33.
GoogleScholar
19. KABIR, M. L., RAHMAN, F., HASSAN, M. Q., AHAMED, F. & MRIDHA, M. A. (2005) Asthma, atopic eczema and allergic rhino-conjunctivitis in school children. Mymensingh Med J, 14, 41-5.
20. NANTANDA, R., TUMWINE, J. K., NDEEZI, G. & OSTERGAARD, M. S. (2013) Asthma and Pneumonia among Children Less Than Five Years with Acute Respiratory Symptoms in Mulago Hospital, Uganda: Evidence of Under-Diagnosis of Asthma. PLoS One, 8, e81562.
Publisher – GoogleScholar
21. NATIONAL INSTITUTE FOR, H. & CLINICAL, E. (2008) Respiratory tract infections. Paediatr Nurs, 20, 31.
22. STONE, S., GONZALES, R., MASELLI, J. & LOWENSTEIN, S. R. (2000) Antibiotic prescribing for patients with colds, upper respiratory tract infections, and bronchitis: A national study of hospital-based emergency departments. Ann Emerg Med, 36, 320-7.
Publisher – GoogleScholar
23. TABATABAEI, S. A., FAHIMZAD, S. A., SHAMSHIRI, A. R., SHIVA, F., SALEHPOR, S., SAYYAHFAR, S., KHANBABAEI, G., ARMIN, S., TABATABAEI, S. R., KHATAMI, A. & KADIVAR, M. (2012) Assessment of a new algorithm in the management of acute respiratory tract infections in children. J Res Med Sci, 17, 182-5.
GoogleScholar
24. VERMA, N., LODHA, R. & KABRA, S. K. (2013) Recent advances in management of bronchiolitis. Indian Pediatr, 50, 939-49.
Publisher – GoogleScholar
25. WALKER, C. L., RUDAN, I., LIU, L., NAIR, H., THEODORATOU, E., BHUTTA, Z. A., O’BRIEN, K. L., CAMPBELL, H. & BLACK, R. E. (2013) Global burden of childhood pneumonia and diarrhoea. Lancet, 381, 1405-16.
GoogleScholar
26. WHO (1984) Memorandum from WHO meeting. A programme for controlling ARI in children Bull WHO 62, 47-58.
27. WHO (2013) Pocket book for hospital care of children: guidelines for the management of common childhood illness 2nd ed. Geneva: World Health Organization.