Discussion
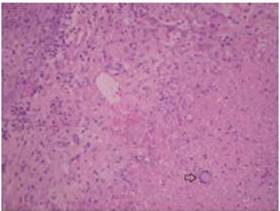
Penile tuberculosis is a rare complication of BCG therapy. Only 12 cases have been described in the literature (Lestre, 2011). A standardized terminology does not exist, and authors use various terms such is granulomatous balanoposthitis, BCG balanitis, BCG infection of penis etc (Yusuke 2006, Michelet 2008, French 2001). Traumatic catheterization and phimosis are considered risk factors for this complication (Yusuke 2006). However in most cases like in our case there is not any obvious predisposing factor. Typical appearance consists of infiltrated erythematous plaque with yellow papules and central necrosis occasionally associated with inguinal lymphadenopathy (Michelet 2008, French 2001). The diagnosis is based on history, clinical exam and histological findings (Michelet 2008). Histological appearances of these changes typically show epithelioid granuloma with central necroses and giant cells of Langhans type.
Identification of M. bovis by traditional methods (Ziehl-Neelsen stain and culture) has been stated to be problematic (Kuresi 2006, French 2001). Talbot et all (1997) has shown that multiplex polymerase chain reaction (PCR) is more effective and specific than conventional methods in BCG detection and may overcome this drawback.
The rarity of this local-regional complication makes a standardized treatment schedule more difficult. In a recent review by Lestre et al (2011) the duration of treatment has varied between 3-12 months, as well as the number of antitubercular agents used. The treatment scheme recommended for other genitourinary complications with local-regional granulomatous inflammation consists of isoniazid and rifampicine for 3 to 6 months and interruption of BCG therapy. The association of ethambutol is usually reserved for situations with hepatic, pulmonary, renal and skeletal involvement (Rischmann, 2000).
Conclusion
The clinician has to be aware of this rare complication in orderto start early therapy with antitubercular agents. Complete resolution of the lesions is the usual outcome.
References
Babjuck, M., Oosterlink, W., Sylvester, R., Kaasinen, E., Bohle, A., Palou, M. & Roupret, M. (2012). ‘Guidelines on Non-Muscle Invasive Bladder Cancer,’ EUA Guidelines, 1-15.
Google Scholar
French, C. G., Hickey, L. & Bell, D. G. (2001). “Caseating Granulomas on the Glans Penis as a Complication of Bacille Calmette-Guérin Intravesical Therapy,” Rev Urol, 3(1) 36-8.
Publisher – Google Scholar
Kureshi, F., Kalaaji, A. N., Halvorson, L., Pittelkow, M. R. & Davis, M. D. P. (2006). “Cutaneous Complications of Intravesical Treatments for Bladder Cancer: Granulomatous Inflammation of the Penis Following BCG Therapy and Penile Gangrene Following Mitomycin Therapy,” J Am AcadDermatol, 55 (2) 328-31.
Publisher – Google Scholar
Lestre, S. I. A., Gameiro, C. D., João, A. & Lopes, M. J. P. (2011). “Granulomas of the Penis: A Rare Complication of Intravesical Therapy with Bacillus Calmette-Guerin,” An Bras Dermatol, 86 (4) 759-62.
Publisher – Google Scholar
Michelet, N., Spenatto, N., Viraben, R., Cunya, J.- F., Mazetc, J. , Trechotd, P. , Barbauda, A., & Schmutza, J.- L. (2008). “BCG Infection of the Glans Penis after Intravesical BCG Therapy,” Ann DermatolVenereol, 135 (6-7) 479-83.
Publisher – Google Scholar
Rischmann, P., Desgrandchamps, F., Malavaud, B. & Chopin, D. K. (2000). “BCG Intravesical Instillations: Recommendations for Side Effects Management,” EurUrol, 37 (Suppl 1)33-6.
Publisher – Google Scholar – British Library Direct
Talbot, E. A., Wiliams, D. L. & Frothingham, R. (1997). “PCR Identification of Mycobacterium Bovis BCG,” J ClinMicrobiol, 35 (3) 566-9.
Publisher – Google Scholar – British Library Direct
Yusuke, H., Yoshinori, H., Kenichi, M. & Akio, H. (2006). “Granulomatous Balanoposthitis after Intravesical Bacillus-Calmette-Guerin Instillation Therapy,” Int J Urol, 13 (10) 1361-3.
Publisher – Google Scholar