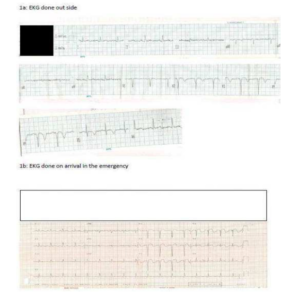
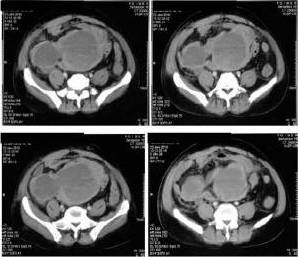
On workup, there was no evidence of anemia or thrombocytopenia. Bleeding time and clotting time was within normal range. His renal functions were mildly deranged (Sr creatinine 1.5mg/dl) however the patient was non-oliguric. The repeat ECG showed Q waves with ST elevation and T-wave inversion in leads V2 —V5. An ultrasonography of the abdomen, done by an experienced sonologist, revealed a heterogenous hypoechoic collection measuring 13.5 x 8.3 cm with evidence of internal septae, echoes and debris. A possibility of hematoma or an intraabdominal abscess was kept. Under sonographic guidance, needle aspiration from the collection was done and haemorrhagic fluid was obtained. Since the fluid was rich in polymorphs and the sugars were low, a contrast enhanced tomogram (CECT) of abdomen was done. It revealed a large hematoma in the right pelvis measuring around 17 x 11 cm. There was no evidence of any contrast extravasation, vascular disruption or aneurysm.
The patient was managed conservatively. Antiplatelets and anticoagulants were withheld. Betablockers, ace inhibitors and statins were continued. Surgical opinion was sought and conservative management was advised. The patient was followed up by serial sonograms, serial haemoglobin estimations and bleeding time estimations. There was a gradual decrease in the size of the hematoma (sonographically demonstrated). The haemoglobin remained stable and there was no increase in bleeding/clotting time. The patient improved clinically during the hospital stay. He was discharged after 10 days of admission with 7 x 5 cm residual hematoma still persisting. On further follow up, gradual decrease in the size of hematoma was noted over next 6 weeks. The patient was lost to follow up after that.
Discussion
Streptokinase is the most commonly used thrombolytic in resource constraint settings because of its cost. It is considered relatively safe but hemorrhagic complications are not uncommon. Most of these hemorragic complications are minor. (Chan WK 1996) Risk factors for hemorrhagic complications include increasing age, elevated pulse pressure, uncontrolled hypertension, recent stroke or surgery, presence of a bleeding diathesis, and severe congestive heart failure. (Awadh N et al 1994)
Bleeding following systemic thrombolysis usually stems from a vascular access site, mucosal (oral, gastrointestinal, urinary, etc.) or skin/soft tissue. Bleeding episodes tend to be more serious in patients requiring invasive procedures (Chan WK 1996).
In one prospective study, Chan, et al assessed the complications arising from use thrombolytic agents in Chinese patients with acute myocardial infarction. They observed that only 13.9% (19/136) patients had complications with the most common complication being bleeding. The commonest site of bleeding was gums followed by intracranial hemorrhage, right groin hematoma, hematuria and hemoptysis in one patient each (Chan WK 1996).
In an Indian study by Malik et al,, 29/102 patients thrombolysed using Streptokinase developed complications. Bleeding was the most common adverse effect seen in 10.7% (11patients). The most common bleeding sites were venepuncture site and GI bleed. Spontaneous hematoma on the medial side of thigh was reported in one patient only. (Malik JK 2004).
Intraperitoneal hemorrhage may result from systemic diseases, such as bleeding diathesis but blunt / penetrating abdominal trauma is the most important cause.(Willis SM 1984) Spontaneous intraparetoneal hemorrage may result from several incidentally discovered etiologies, including rupture of a vascular neoplasm, hemorrhagic cyst, or ectopic pregnancy; perforation of a duodenal ulcer or other gastrointestinal pathologies; and inflammatory erosive processes (Willis SM 1984). In our patient these possibilities were ruled out clinically as well as radiologically.
Thrombolytic induced spontaneous intraperitoneal hematomas are rarely reported. Occasional cases of subcapsular hepatic hematomas have been reported with thrombolytics like streptokinase and r-tpa (Jimenez AG et al. 1997). Kenan et al reported a case of an 80year old female developing abdominal pain and distention of increasing intensity following thrombolysis. Abdominal computed tomography demonstrated a huge intraperitoneal hematoma (Kenan Yalta et al 2007), as seen in our patient.
Management of streptokinase induced bleeds involves application of direct pressure to minor sites of bleeds and discontinuation of the lytic agent and antiplatelet drugs. In cases of major bleeds with drop of hemoglobin or hypotension, volume replacement by blood transfusion is indicated. Cryoprecipitates may be helpful in unresponsive bleeds. Plasma infusion is usually not required if the levels of fibrinogen are 100 mg/dl or more. Aminocaproic acid, Aprotonin and Tranexamic acid are the available antifibrinolytic agents commonly used to reverse the bleeding. (Akhtar TM 1992). Aprotonin has been specifically used to control bleeding in patients requiring rescue CABG after receiving streptokinase. The recommended dose administered after streptokinase is 2 million KIU before bypass, with an additional 1-2 million KIU added to the pump prime and a continuous infusion of 0.5 million KIU per hour during surgery (Akhtar TM 1992).
In our patient, the hematoma itself could have resulted in localized compression and contained the bleeding. We had discontinued antiplatelets and anticoagulants and watched for further bleeding by monitoring haemoglobin and abdominal distention. Since these conservative measures contained the bleeding, other supportive measures like blood transfusion, antifibrinolytics and cryoprecipitates were not needed.
Surgical drainage of streptokinase induced hematomas is usually not required, as was the case in our patient. Spontaneous resolution is a rule rather than exception. In some cases of intracranial hematomas, successful outcomes have been reported with timely neurosurgical evacuation. (Al-Khuwalia TS 2005)
Conclusions
Generalized fibrinolytic state attained after institution a non specific thrombolytic can predispose a patient to bleeding complications. Mild non life threatening bleeds and superficial bleeds can be managed conservatively but patient could develop massive bleeding in anybody compartment. Spontaneous intra peritoneal hematoma is an unusual complication following thrombolysis with streptokinase. One should carefully observe patients following thrombolysis, intervention may not always be possible in acute stage. Conservative management will usually suffice in such patients.
References
Akhtar, T. M., Goodchild, C. S. & Boylan, M. K. G. (1992). “Reversal of Streptokinase Induced Bleeding with Aprotonin for Emergency Cardiac Surgery,” Anaesthesia ,47:226-228.
Publisher – Google Scholar
Al-Khuwalia, T. S., Wani, B. A., Daywood, H. A. & Khan, M. A. (2005). “Successful Outcome after Evacuation of Intracranial Hematoma Following Thrombolysis in Acute Myocardial Infarction,” Saudi Med J;vol 26(1):130-132.
Publisher – Google Scholar
Awadh, N. Ronco, J. J., Bernstein, V., Gilks, B. & Wilcox, P. (1994). “Spontaneous Pulmonary Hemorrhage after Thrombolytic Therapy for Acute Myocardial Infarction,” Chest;106:1622-4.
Publisher – Google Scholar
Chan, W. K., Chiu, A. & Yui, C. S. (1996). ‘Prevalence of Various Complications of Thrombolytic Therapy in Patients with Acute Myocardial Infarction: Experience in a Local Regional Hospital,’ J HK Coll cardiol; vol 4:77-80.
Google Scholar
Jimenez, A. G., Mao, M. C., Moan, D. F., Ferreiro, S. O., Gutierrez, M. G., Marini, M. et al. (1997). “Hepatic Bleeding and Hemorrhagic Shock Following Thrombolytic Therapy in Patients With Acute Myocardial Infarction,” Chest;111;1787.
Publisher
Malik, J. K. & Khan, G. Q. (2004). “Adverse Effect Profile of Streptokinase Therapy in Patients with Acute Myocardial Infarction: A Prospective Study,” JK Practitioner;11(2):106-109.
Publisher – Google Scholar
Willis, S. M. & Bailey, S. R. (1984). “Streptokinase-Induced Subcapsular Hematoma of the Liver,” Arch Intern Med.; 144: 2084-2085
Publisher – Google Scholar
Yalta, K., Birhan, M., Karadaş, F. & Gümüş, C. (2007). “Spontaneous Massive Intraperitoneal Hematoma Accompanied by Acute Severe Anemia after Low-Dose Thrombolytic Therapy,” Türk Kardiyol Dern Arş; 35:370-372.
Publisher